Implementing phase 3
Contents
- Urgent actions to address inequalities in NHS provision and outcomes 2
- Mental health planning 13
- Restoration of adult and older people’s community health services 18
- Using patient initiated follow-ups as part of the NHS COVID-19 recovery 19
- 2020/21 Phase 3 planning submission guidance 27
- COVID-19 data collections: changes to weekend collections 44
Classification: Official
Publications approval reference: C0716
Implementing phase 3 of the NHS response to the COVID-19 pandemic
7 August 2020
Further to the letter of 31 July 2020 about the third phase of the NHS response to COVID-19, this document provides a range of supplementary materials to support implementation.
1. Urgent actions to address inequalities in NHS provision and outcomes
Summary
COVID-19 has further exposed some of the health and wider inequalities that persist in our society. We are therefore asking you to work collaboratively with your local communities and partners to take the following eight urgent actions:
- Protect the most vulnerable from COVID-19, with enhanced analysis and community engagement, to mitigate the risks associated with relevant protected characteristics and social and economic conditions; and better engage those communities who need most support.
- Restore NHS services inclusively, so that they are used by those in greatest need. This will be guided by new, core performance monitoring of service use and outcomes among those from the most deprived neighbourhoods and from Black and Asian communities, by 31 October.
- Develop digitally enabled care pathways in ways which increase inclusion, including reviewing who is using new primary, outpatient and mental health digitally enabled care pathways by 31 March.
- Accelerate preventative programmes which proactively engage those at greatest risk of poor health outcomes; including more accessible flu vaccinations, better targeting of long-term condition prevention and management programmes such as obesity reduction programmes, health checks for people with learning disabilities, and increasing the continuity of maternity carers.
- Particularly support those who suffer mental ill health, as society and the NHS recover from COVID-19, underpinned by more robust data collection and monitoring by 31 December.
- Strengthen leadership and accountability, with a named executive board member responsible for tackling inequalities in place in September in every NHS organisation, alongside action to increase the diversity of senior leaders.
- Ensure datasets are complete and timely, to underpin an understanding of and response to inequalities. All NHS organisations should proactively review and ensure the completeness of patient ethnicity data by no later than 31 December, with general practice prioritising those groups at significant risk of COVID-19 from 1 September.
- Collaborate locally in planning and delivering action to address health inequalities, including incorporating in plans for restoring critical services by 21 September; better listening to communities and strengthening local accountability; deepening partnerships with local authorities and the voluntary and community sector; and maintaining a continual focus on implementation of these actions, resources and impact, including a full report by 31 March.
Introduction
COVID-19 has shone harsh light on some of the health and wider inequalities that persist in our society. Like nearly every health condition, it has become increasingly clear that COVID-19 has had a disproportionate impact on many who already face disadvantage and discrimination. The impact of the virus has been particularly detrimental on people living in areas of greatest deprivation, on people from Black, Asian and Minority Ethnic communities, older people, men, those who are obese and who have other long-term health conditions, people with a learning disability and other inclusion health groups, those with a severe mental illness and those in certain occupations1. COVID-19 risks further compounding inequalities which had already been widening2.
Please take urgent action, in collaboration with local communities and partners, to increase the scale and pace of progress in reducing health inequalities, and regularly assess progress.
It is an integral part of the third phase of the NHS response to COVID-19, as set out in the letter to the NHS on 31 July. As such, the actions set out here focus on the immediate tasks of continuing to protect those at greatest risk of COVID-19, restoring services inclusively and accelerating targeted prevention programmes, underpinned by improvements in leadership and accountability, data and insight and collaborative planning.
These measures will help lay the foundations for further action, particularly to enhance prevention and contribute to the concerted cross-governmental and societal effort needed to address the wider determinants of health; building on the strategy set out in the NHS Long Term Plan and the NHS’s legal duties with regards to equality and health inequalities.
1 For example, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892085/disparities_review.pdf
2 See Chapter 5 https://www.gov.uk/government/publications/health-profile-for-england-2019
Action 1: Protect the most vulnerable from COVID-19
Systems (integrated care systems/sustainability and transformation partnerships), working with local authorities and other partners, should regularly update plans for protecting people at greatest risk during the pandemic. This includes ensuring that people who may be clinically extremely vulnerable to COVID-193 infection are identified and supported to follow specific measures – such as shielding – when advised, and to access restored health and care services when required.
As part of these plans, systems are asked to explicitly consider risks associated with people’s relevant protected characteristics4, and wider socio-economic, cultural and occupational risk factors in the local area. Plans should set out how insight into different types of risk and wider vulnerability within their communities will be improved, including through population health management and risk stratification approaches and deeper engagement with those at risk of exclusion, including carers. They should also ensure information on risks and prevention is accessible to all communities and reflects the need for culturally competent prevention campaigns.
Alongside these system plans, protection of NHS staff against COVID-19 also remains a key priority. NHS employing organisations have been completing COVID-19 risk assessments of staff by the end of July and taking subsequent action.
3 Specific groups of people have been defined by Government as clinically extremely vulnerable to COVID-19, based on expert advice and the earliest available clinical evidence. Clinicians have also been able to identify individuals as clinically extremely vulnerable based on their professional judgement and add them to the Shielded Patient List. As evidence regarding the impact of the virus increases, a new predictive risk model is being developed on behalf of the Department of Health and Social Care, that reflects a wider range of factors such as demographics alongside long-term health conditions, to better understand cumulative risk of serious illness for individuals if they catch COVID-19. Options for applying this model across a variety of health and care settings, including developing a tool to support conversations between patients and clinicians on individual risk, are being considered. More information will be provided over the summer as this work progresses.
4 See full list of protected characteristics at https://www.equalityhumanrights.com/en/equality-act/protected-characteristics
Action 2: Restore NHS services inclusively
The third phase of the NHS response to COVID-19 focuses on accelerating the return to near-normal levels of non-COVID health services. As part of that, and as the letter on 31 July highlights, specific actions may be needed to support any groups of patients who might have unequal access to diagnosis and treatment, including proactively reaching out to these patients.
To monitor this objective of an inclusive restoration of services, monthly NHS reporting will in future include measures of performance in relation to patients from the 20% most deprived neighbourhoods (nationally and locally, using the Index of Multiple Deprivation), as well as those from Black and Asian communities where data is available.
Monitoring will compare service use and outcomes across emergency, outpatient and elective care, including cancer referrals and waiting time activity. Over time, we will develop key metrics on clinical needs, activity and outcomes, including end of life care, mental health, children’s health services, and primary care. We will also consider how to expand the approach to established performance standards and seek to improve data and insights on service performance experienced by people with a disability. All local NHS organisations should adhere to this approach in their internal and public performance reports, and swift action should be taken to rectify inequalities which are identified.
Our national and regional teams will also undertake specific reviews of the scope for specialised services to further address health inequalities. This will include monitoring the restoration of services to improve identification and engagement across all patient groups, assessing the scope for improving outcomes for those experiencing the greatest inequalities, and improving underlying recording of ethnicity and other relevant protected characteristics in datasets relevant to specialised services, including clinical databases, registries and audits. Specialised commissioning will require mandatory recording of ethnicity in clinical databases cited in specialised services service specifications by 31 March 2021.
These indicators should be considered alongside wider sources of community-based insight and the measurement of commitments set out in the NHS Long Term Plan. By 31 October 2020, we will further refine analysis of local inequality to support this wider work5.
5 This analysis will also benefit from the work of the new NHS Race and Health Observatory
https://www.england.nhs.uk/2020/05/nhs-england-and-nhs-confederation-launch-expert-research-centre-on-health-inequalities/
Action 3: Develop digitally enabled care pathways in ways which increase inclusion
During the response to COVID-19, the health and care system has seen unprecedented levels of uptake of digital tools and services, helping keep patients, carers, friends, relatives and clinicians safe and ensuring that essential care can continue. Digitally enabled services provide an opportunity to create a more inclusive health and care system, creating more flexible services and opening up access for people who might otherwise find it hard to access in person, for example due to employment or stigmatisation.
The shift needs to be carefully designed to ensure it does not affect health inequalities for others, due to barriers such as access, connectivity, confidence or skills. All NHS organisations are therefore asked to ensure that no matter how people choose to interact with services, they should receive the same levels of access, consistent advice and the same outcomes of care. To monitor this, new care pathways should be tested for achieving a positive impact on health inequalities, starting with four: 111 First; total triage in general practice; digitally enabled mental health; and virtual outpatients. For each, systems should assess empirically how the blend of different ‘channels’ of engagement (face-to-face, telephone, digital) has affected different population groups, including those who may find any particular channel more difficult to access, and put in place mitigations to address any issues. System reviews, with agreed actions, should be published on all four by 31 March 2021.
5 This analysis will also benefit from the work of the new NHS Race and Health Observatory https://www.england.nhs.uk/2020/05/nhs-england-and-nhs-confederation-launch-expert-research-centre-on-health-inequalities/
Action 4: Accelerate preventative programmes which proactively engage those at greatest risk of poor health outcomes
Some of the most significant, specific contributions the NHS can make to reduce health inequalities are to improve preventative services, maternity services and services for children and young people, including immunisation. The best approaches use an integrated and personalised model of care that takes account of wellbeing and wider social and economic needs. Local NHS systems will need to address local priorities, in collaboration with partners. At the same time, we expect consistent national progress on the following four areas:
- Improving uptake of the flu vaccination in underrepresented ‘at risk’ groups: This coming winter, we may be faced with co-circulation of COVID-19 and flu. It is therefore essential to increase flu vaccination levels for those who are living in the most deprived 20% of neighbourhoods, those from BAME communities and people with a learning disability, and significantly reduce the gap in uptake compared with the population as a whole. We recognise this may be challenging given the expansion of the flu programme and the constraints of infection prevention and control for this winter. It will therefore require high quality, dedicated and culturally competent engagement with local communities, employers and faith groups.
- General practice, working with analytical teams and wider system partners, including social care and voluntary sector organisations, should use the capacity released through the modified QOF requirements for 2020/21 to develop priority lists for preventative support and long-term condition management, such as for obesity management and hypertension. These should reflect how health needs and care may have been exacerbated during the COVID-19 pandemic. Priority groups for programmes such as obesity prevention, smoking cessation, and alcohol misuse, cardiovascular, hypertension, diabetes and respiratory disease prevention and long-term condition management should be engaged proactively, recognising the extra barriers to engagement which COVID-19 has brought, reflecting the wider strategy for restoring primary care services. For example, local areas should focus on generating referrals into the NHS Diabetes Prevention Programme on individuals of South Asian, Black African and Black Caribbean ethnicity and those from the most deprived communities.
- As set out in the Phase 3 letter of 31 July, GP practices should ensure that everyone with a learning disability is identified on their register and that annual health checks are completed. As a minimum, by 31 March systems should aim to ensure that primary care practices reach an annual rate of seeing at least 67% of people on their learning disability register through higher quality health checks, accelerating progress towards the NHS Long Term Plan target of 75% by 2023/24. This approach is backed by a £140 per person fee, a primary care network incentive, and quality improvement tools. We expect every system to monitor and achieve this goal. To improve their GP learning disability register, it is particularly important to ensure people with a learning disability from a BAME background are known and included.
There is also a fundamental need to improve the provision of comprehensive physical health checks and follow-up interventions for people with severe mental illnesses (SMIs). At present, there is good completion rates of some of the individual elements of the comprehensive check. However, at a national level we are falling short of our ambition to provide this check for 60% of people with SMI. Given the very significant health inequalities faced by those with SMI, of reduced life expectancy of 15-20 years, further rapid progress is needed. We will also review incentives to improve completion rates from 2021/22. - In maternity care, implementing continuity of carer for at least 35% of women by March 2021, with the number of women receiving continuity of carer growing demonstrably towards meeting the goal of most women. As part of this, by March, systems should ensure that the proportion of Black and Asian women and those from the most deprived neighbourhoods on continuity of carer pathways meets and preferably exceeds the proportion in the population as a whole. This is in line with the NHS Long Term Plan commitment that by 2024 75% of women from these groups will receive continuity of carer, and is more urgent in light of the increased risk facing Black and Asian women of both poor maternity outcomes and outcomes from COVID-19.
Action 5: Particularly support those who suffer mental ill-health
Mental ill-health is a significant contributor to long-term health inequalities, and the immediate and longer-term social and economic impacts of COVID-19 have the potential to contribute to or exacerbate mental health problems.
In response, systems have been asked to validate their plans to deliver the mental health transformation and expansion programme over the next eight months. These plans should pay particular attention to advancing equalities in access, experience and outcomes for groups facing inequalities across different mental health pathways, such as BAME communities, LGBT+ communities, children and young people with neurodevelopmental disorders, and older people. To underpin this, providers and systems should improve the quality and flow of mental health data to allow more robust monitoring of disproportionalities in access and experience and take action where problems are identified. Building on the monitoring of IAPT, by 31 December providers must enhance the overall quality and completeness of ethnicity and other protected characteristics data provided to the national Mental Health Services Data Set.
The Advancing Mental Health Equalities Taskforce will set out further advice and support by 31 October6.
6 Advice is also already available from
https://www.rcpsych.ac.uk/improving-care/nccmh/care-pathways/advancing-mental-health-equality
Action 6: Strengthen leadership and accountability
These actions and wider measures to increase the pace and scale of progress to reduce inequalities rest on clear and accountable leadership. All systems and every NHS organisation should therefore identify, before October, a named executive board-level lead for tackling inequalities. Primary care networks should also nominate their clinical director or an alternative lead to champion health equality.
As outlined in the NHS People Plan published on 30 July, addressing health inequalities will be enhanced by ensuring that we reflect the diverse communities we serve. We are committed to strengthening the culture of belonging and trust which enables this. Each NHS board has therefore been asked to publish an action plan showing how over the next five years its board and senior staffing will, in percentage terms at least, match the overall BAME composition of its overall workforce, or its local community, whichever is the higher. We are ourselves committed to ensuring that at least 19% of our people come from a Black, Asian or minority ethnic background at every level, including director level, by 2025.
Action 7: Ensure datasets are complete and timely
Given the importance of data and insight to understanding need and monitoring progress, all NHS organisations must review the quality and accuracy of their data on patient ethnicity, as recommended by the Public Health England report Understanding the impact of COVID-19 on BAME groups,7 and ensure these characteristics are recorded for all patients by 31 December 2020. As part of these measures, retrospectively updating and completing the COVID-19 Hospital Episode Surveillance System (CHESS) is essential.
Specific action is needed to improve the recording of ethnicity within general practice. We expect that to start, by no later than 1 September, through seeking to confirm the ethnicity of the adults who are eligible for flu vaccination; groups who are also typically likely to be at risk of COVID-19. By the end of September, we will aim to have developed a joint plan with primary care partners to extend that to all patients as quickly as possible. It will also be important to improve GP registration for those without proof of identity or address.
The use of data on protected characteristics to improve care and planning will be enhanced by combining with better recording of wider risks, using risk prediction tools. Action is also needed locally to improve the understanding of the needs of inclusion health groups, such as people who are homeless and refugees, and of the impact of intersectionality.
6 Advice is also already available from
7 https://www.rcpsych.ac.uk/improving-care/nccmh/care-pathways/advancing-mental-health-equality
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892376/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf
8 People are often disadvantaged by multiple sources of disadvantage and discrimination which can compound each other
Action 8: Collaborate locally in planning and delivering action
Systems (integrated care systems and sustainability and transformation partnerships) will need to support and oversee delivery of these actions, understanding population needs and building partnerships to address health inequalities. By 21 September 2020, system plans to restore critical NHS services should take account of all the actions set out above. Systems should assess progress regularly and provide an overall account of delivery against the actions in this note by 31 March 2021. They should also look to strengthen accountability to their local population and listen to their concerns, particularly those at risk of health inequalities. Data should be regularly published at the lowest meaningful geographical level possible to support this.
Areas with the greatest inequalities have received additional funding through the CCG allocation formula. These resources should be targeted at the areas of greatest deprivation and used to support these actions and local priorities for addressing inequality. Systems will be asked to review how resources have been used to address health inequalities over the financial year by 31 March 2021.
The collaboration seen during COVID-19 with local government and the voluntary, community and social enterprise sector, and the population health management approaches deployed, should be used to inform the development of longer-term plans to address the underlying causes of health inequality from 2021/22. Plans are likely to particularly benefit from bolstering the primary care workforce, especially in deprived areas, including ensuring primary care networks make full use of the Additional Roles and Reimbursement Scheme and help increase the number of GPs in under-doctored areas. Systems should also support NHS organisations seeking to serve as effective ‘anchor’ institutions, learning from the new NHS England and NHS Improvement/Health Foundation network.
Putting these actions into practice is a shared endeavour. We will seek rapid feedback on areas of action where national collaboration and learning may be valuable alongside the local work of systems, places and neighbourhoods.
Task and finish group on accelerating NHS progress on tackling health inequalities during the next stage of COVID-19 recovery
Dr Owen Williams OBE (Chair) – CEO Calderdale and Huddersfield NHS Foundation Trust
Evelyn Asante-Mensah OBE – Chair, Pennine Care NHS Foundation Trust
Charlotte Augst – CEO, National Voices
Nicola Bailey – Chief Officer, NHS County Durham CCG
Linda Charles-Ozuzu – Regional Director of Commissioning, NHS England and NHS Improvement
Samantha Clark – CEO, Learning Disability England
Kiren Collinson – Clinical Chair, Oxford CCG
Dr Vin Diwakar – Regional Medical Director, NHS England and NHS Improvement
Amanda Doyle – Chief Clinical Officer for West Lancashire CCG, Blackpool CCG and Fylde and Wyre CCG, and ICS Lead for Lancashire and South Cumbria
Professor Kevin Fenton – Regional Director, Public Health England
Donna Hall CBE – Chair, New Local Government Network
Jacob Lant – Head of Policy and Public Affairs, Healthwatch England
Patricia Miller – CEO, Dorset County Hospital NHS Foundation Trust
Patrick Nyarumbu – Regional Director of Nursing Leadership and Quality, NHS England and NHS Improvement
Jagtar Singh – Chair of Coventry and Warwickshire Partnership NHS Trust
Robin Tuddenham – Chief Executive, Calderdale Council
We are also grateful to members of the Health and Wellbeing Alliance, and other partners and colleagues in providers, commissioners and systems who have helped inform and develop the actions.
2. Mental health planning
Here we outline the steps we are taking to support the next phase of our COVID-19 response, in which mental health needs may increase significantly. It continues to be a requirement that the Mental Health Investment Standard (MHIS) is met in every CCG in 2020/21. We will be repeating the independent audits of the MHIS and we expect to see historic underinvestment in Mental Health addressed in every CCG.
As with the rest of the NHS the Phase 3 Mental Health planning process closes on 21 September, with an interim submission on 1 September, allowing us to allocate the additional funding required to meet the MHIS. The national mental health team will work closely with your teams over the coming weeks to support this planning process. We need to grow services, recruit staff and make the necessary changes to ensure we still meet the ambitions outlined in the NHS Long Term Plan (LTP).
STPs / ICSs should continue to strive to achieve the specific deliverables for 2020/21 set out in the NHS Mental Health Implementation Plan 19/20–23/24 to the best of their abilities, recognising that COVID-related practical constraints (including staff absence, social distancing or disruption to referral pathways) may restrict what they are able to deliver in practice and use of technology enabled support will need to continue. We need to make sure our trajectories for 2020/21 are a realistic reflection of the context we are in. Mental health providers should organise themselves at STP/ ICS level (including identifying a lead mental health provider), and work with their STP/ICS to ensure that plans are adequate to meet the activity requirements in 2020/21. To support moving towards a “System by Default” way of working from April 2021, ICS/STP leads and a lead Mental Health Provider will be asked to sign off on their Phase 3 Mental Health plans, confirming that the MHIS investment covers all the priority areas for the programme. Where a Provider Collaborative exists, it may be that existing partnership arrangements can support this way of working, as well as other local partnerships.
Our priority is to maintain momentum and continue to deliver the LTP. The LTP is a solid foundation to address the impact of COVID-19, which will improve the quality of mental health services and expand access to 2 million more people each year by 2023/24. We can confirm that the total annual allocations for all SDF (Transformation Funding) programmes in 2020/21 remain in place and sites should proceed with delivery. The mechanism for flowing funding will be confirmed shortly.
Our partners find themselves operating in an increasingly challenging environment. The partnerships we have created in recent months with local authorities, the third sector and other parts of the health system are central to successful delivery of the programme and need to be maintained. We must make sure that over the next few months we work with patients, staff and families, by ensuring that they play a central and meaningful role in our decision making and reshaping of services. The NHS-commissioned Working Well Together toolkit provides practical steps on how to do this. NHS-Led Provider Collaboratives offer a model for achieving and strengthening these local partnerships and their implementation this year is critical.
We are beginning to see increased acuity in presentations to our services. To ready ourselves for winter and a potential second wave, we must use the Phase 3 planning process to ensure we invest across the entire health pathway, and not just in beds. This means continuing our investment in 24/7 crisis lines and alternatives to admission, as well as strengthening and investing in community services to help people to stay well and avoid escalations where possible. This is how we will transform the quality and reach of mental health care in this country.
Workforce growth remains the key enabler but also constraint to our ambition. When systems come to sign off investment plans for 2020/21, they should do so with the confidence that they have triangulated activity, finance and workforce trajectories and produced a plan that is feasible.
Evaluating the role of digital transformation must also be a central feature of this planning exercise as it offers a major opportunity to modernise care. However, in many cases, it should not be a replacement for face-to-face support. Systems are encouraged to review the impact of digital transformation in their area before moving into this next phase.
Local services should do all they can to meet the dementia diagnosis target, but our shared commitment to older adults goes beyond that, and we must also focus on ensuring that access to talking therapies, community mental health care and 24/7 crisis support meets the needs of older adults.
Addressing health inequalities remains a priority for our work on mental health. The Advancing Mental Health Equality Resource and IAPT Positive Practice Guides for Older People and BAME communities should be used to the best of their advantage.
We can now bring about the eradication of dormitories in mental health settings, supported by extra capital of £250 million in 2020/21 with a further sum next year. We ask mental health providers with dormitory provision to work with regional finance and estates colleagues to identify schemes that can proceed immediately, to ensure that we deliver this clear patient benefit without delay.
We will discuss 2020/21 plans during our upcoming Q1 Deep Dive round. As of Q2 2020/21, national assurance activity and data collections will resume with performance being discussed in the quarterly deep dives.
Areas of focus for the rest of 2020/21
The expansion of Improving Access to Psychological Therapies (IAPT) services should be at the forefront of this next phase as they provide NICE recommended treatment for the most common mental health problems and accept self-referral. The specialised support IAPT can offer to those with PTSD, anxiety, depression or to those who have spent lengthy time in an ICU, are all the more vital in the context of COVID-19. For this reason, we must use this year to grow and bring in more trainees to the service. Money is available to augment salary replacement costs to help with the expected, significant, surge in demand for IAPT services. Where regions did not achieve IAPT targets last year, recovery trajectories must be provided as part of the planning process.
Services should conduct proactive reviews for all patients on community Mental Health teams’ caseloads and increase therapeutic activity and supportive interventions to prevent relapse or escalation of mental health needs for people with SMI in the community. In 2020/21, the year-on-year baseline funding uplift for community-based services for people with SMI, including EIP services and Physical Health Checks for People with SMI, is £162 million. The cumulative baseline uplift since 2018/19 is now £251 million. This is a significant component of CCG baseline funding increases and we encourage services to invest this as soon as possible to increase staffing to required levels. Services should also use this funding to promote and prioritise physical health for people with SMI, and accelerate LTP transformation where possible, including for adult eating disorders, mental health rehabilitation, and ‘personality disorders’ services. The ambition to eliminate inappropriate out of area placements for adult acute care by April 2021 stands and good community care is an important facet to delivering this ambition.
Children and young people have been significantly impacted by COVID-19, through the disruption to multi-agency support and through the closure of schools and colleges. As schools prepare to welcome children and young people back, services should ensure that local access to pathways, consultation and advice is clearly advertised. They should continue to expand provision, focusing on the needs of the most vulnerable such as those with autism or neurodisability, making full use of the £47 million year-on-year uplift in 2020/21 CCG baseline funding for CYP mental health services (including crisis and eating disorders). The baseline funding uplift since 2018/19 is now £83 million. The National Quality Improvement Taskforce for children and young people’s mental health, learning disability and autism inpatient services has resumed its work and will be getting in touch with providers in the coming weeks. Community and inpatient services should continue working to improve pathways of care across their services.
This year will be the largest flu vaccination programme and we must do all we can to protect our staff and patients. We are already engaging with the vaccination programme team to make sure the specific needs of the mental health sector are considered and will be working closely with regional colleagues.
Support for NHS staff
We have launched a health and wellbeing offer for all NHS staff, which includes a telephone and text helpline and access to support for issues such as debt, bereavement, stress, domestic violence etc.
We are aware that many systems are putting in place local offers to support health and social care frontline staff. As signalled in the Winter Wellbeing plan, we are supporting a number of pilot sites across the country, testing an approach to improving staff mental health by establishing resilience hubs working in partnership with Occupational Health programmes. These pilots will undertake proactive outreach and assessment, and coordinate referrals access to prompt and evidence-based treatment and support for a range of needs, with a view to making the case for further roll out in future years.
The direct and indirect effects of COVID-19 will probably have psychological and social impacts that will have an effect on mental health and planning for some years to come. We will continue to address the impact of COVID-19 for the rest of this year, and beyond. Services should continue to ensure delivery of safe care in appropriate settings, addressing risks to both the mental and physical health of patients and staff in line with published guidance.
3. Restoration of adult and older people’s community health services
This guidance on the restoration of adult and older people’s community health services supersedes the prioritisation guidance for community health services first published on 20 March 2020 and updated on 2 April 2020, which is withdrawn.
All the service areas listed in the 20 March 2020 and 2 April 2020 guidance should now be fully reinstated, including where needed home visits for vulnerable adults, subject to appropriate infection control protections in line with Public Health England advice, and any other relevant NHS England guidance.
4. Using patient initiated follow-ups as part of the NHS COVID-19 recovery
Introduction
This section provides practical information about implementing patient initiated follow-up (PIFU) processes in secondary care. This guidance has been informed by the experience of providers and specialties that implemented PIFU as part of their COVID-19 response or before the pandemic, and guidance published by the national cancer programme.
In line with the personalised care agenda, PIFU can play a key role in enabling shared decision-making and supporting patients with self-management, by helping them know when and how to access the right clinical input. Used alongside clinical waiting list reviews, remote consultations and a ‘digital first’ approach, it is a useful tool for provider recovery.
Benefits of patient initiated follow-up
| Benefits to patients | Benefits to clinicians | Benefits to organisations and systems |
|
|
|
9 Coleridge S, Morrison J. Patient-initiated follow-up after treatment for low risk endometrial cancer: a prospective audit of outcomes and cost benefits. Int J Gynecol Cancer Published Online First: 5 May 2020.
10 Wickham-Joseph R, Luqman I, Cooper N, et al. P166 Patient-initiated follow-up for low-risk endometrial cancer: an economic evaluation. Int J Gynecol Cancer 2019; 29: A160.
11 Hewlett S, et al. Patient initiated outpatient follow up in rheumatoid arthritis: six year randomised controlled trial. BMJ 2005; 330: 171.
When to use patient initiated follow-ups
Individual services should develop their own guidance, criteria and protocols on when to use PIFUs. PIFU pathways can be used for patients of any age, provided the patient and their clinician agree that it is right for them. In some cases, it may be appropriate for the patient to share the responsibility with a carer or guardian. Some general guidance is given below.
- For PIFU to be suitable for a patient, they should meet the following conditions:
at low risk of urgent follow-up care and satisfies criteria established by the specialty - is confident and able to take responsibility for their care for the time they will be on the PIFU pathway, eg they do not have rapidly progressing dementia, severe memory loss or a severe learning disability
- understands which changes in their symptoms or indicators mean they should get in touch with the service, and how to do so
- has the tools to understand the status of their condition (eg devices, leaflets, apps) and understands how to use them
- has the health literacy and knowledge, skills and confidence to manage their follow-up care (patient activation); if they do not, the patient may benefit from support to improve these areas in line with the personalised care approach
- understands how to book their follow-up appointments directly with the service, and how long they will be responsible for doing this; for some patients who are unable to book their appointments directly, administrative staff at their care home or GP surgery may be able to help.
If any of the following conditions are met, the appropriateness of PIFU for the patient needs to be carefully considered:
- the patient’s health issues are particularly complex
- there are clinical requirements to see the patient on a fixed timescale (timed follow-ups), although
- it is important to note that a blend of PIFU and timed follow-ups can also be offered (eg for cancer pathways)
- the clinician has concerns about safeguarding for the patient
- the patient takes medicines that require regular and robust monitoring in secondary care
- the patient is not able to contact the service easily (eg lack of access to a telephone ).
12 Whear R, et al. Patient initiated clinics for patients with chronic or recurrent conditions managed in secondary care: a systematic review of patient reported outcomes and patient and clinician satisfaction. BMC Health Serv Res 2013; 13: 501.
13 Batehup L, et al. Follow-up after curative treatment for colorectal cancer: longitudinal evaluation of patient initiated follow-up in the first 12 months. Support Care Cancer 2017; 25: 2063–73.
14 Goodwin VA, et al. Implementing a patient‐initiated review system for people with rheumatoid arthritis: a prospective, comparative service evaluation. J Eval Clin Practice 2016; 22(3): 439-445.
Clinical specialties most suited for patient initiated follow-ups
PIFU can be used in a wide variety of clinical specialties, both medical and surgical:
|
|
Implementing patient initiated follow-ups
Example high-level plan for implementing PIFU
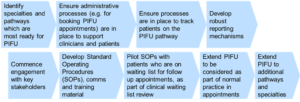
Example implementation checklist adapted from work by Somerset CCG.
| Strong clinical leadership and engagement | Identify the specialties and pathways most ready for PIFU, by considering the following:
Arrange workshops and give clinicians protected time to plan and design their own PIFU processes. |
| Effective planning and programme management | Identify service managers responsible for delivering PIFU. Set regular meetings of service managers to discuss emerging barriers. Identify stakeholders, eg:
Develop engagement plan. |
| A simple patient narrative | Keep the story simple, consistent and focused on benefits, including the opportunity to empower patients. Develop patient information leaflets and a method for their distribution (eg via post, email, text message). Communicate clearly to patients about symptoms to watch out for and how to book an appointment. Engage with patient groups and adapt rollout strategy as necessary. Gather feedback from patients to enable continuous improvement. |
| Locally determined eligibility criteria and protocols | Clinical leads define the PIFUs for their own specialty, follow-up periods and appropriate patients. Work with admin and IT teams to define how patients will be reflected on booking systems and clinic outcomes. Identify staff resources required to take calls from patients requesting PIFU appointments. Work with IT to integrate clinic outcomes for PIFU patients into electronic medical records. Integrate PIFU with patients’ personalised care and support plans. Carry out a desk review of patients on the
Embed consideration of PIFU in normal practice for patient appointments. |
| Accurate reporting systems for tracking PIFU activity | Understand how best to record a patient as being on the PIFU pathway locally. Analyse baseline activity and performance. Estimate the impact of PIFU on service appointments and waiting list, and set up processes to monitor this regularly. Set up performance reporting for the service (see section on data collection). Have a system for recording discharges at the end of defined follow-up time period. |
| Flexible clinic systems | Create flexible clinic capacity to accommodate PIFU appointments. Set up a user-friendly system for patients to book follow-ups. Switch off default follow-up letters for patients on the PIFU pathway. |
Data collection
Implementing PIFU may create challenges for recording and reporting activity, therefore you may wish to consider implementing local reporting measures that provide insight into the following for each service.
Headline metrics
- Total number and proportion of patients on the PIFU pathway.
- Patient outcomes, eg recovery rates, relapse rates.
- Waiting times.
- DNA rates.
Process measures
- Number and proportion of patients who are:
- put on a PIFU pathway following an appointment
- discharged to primary care from PIFU pathway
- discharged to primary care without being put on a PIFU pathway
- taken off the PIFU pathway and put back on the routine follow-up pathway.
- Average time between an individual patient’s appointments at different stages of treatment.
- Number of patients on the PIFU pathway who:
- made contact with the service and had an appointment booked
- made contact with the service but had their issues resolved without requiring an appointment.
- Patient demographics and numbers of patients for whom specific conditions are being managed.
Other outcomes and experience measures
- Patient and staff experience measures.
- Changes in patients’ knowledge, skills and confidence (activation) using Patient Activation
- Measure or similar measures.
- Workforce productivity measures.
Case studies and other resources
General resources
Personalised care resources and policy documents
Letter to GPs about PIFU: Cambridge University Hospitals NHS Foundation Trust
Patient-facing information: The Mid Yorkshire Hospitals NHS Trust; The Royal Free London NHS Foundation Trust
Equality Impact Assessment, Guildford and Waverley CCG
Specialty or condition-specific resources
Cancer:
- Living with and beyond cancer: handbook for implementing personalised stratified follow-up pathways
- Personalised care and support tools: Cheshire & Merseyside Cancer Alliance
- Patient centred follow-up video for breast cancer: East of England Cancer Alliance
- Breast cancer patient leaflet: Sandwell and West Birmingham Hospitals NHS Trust
- Gynaecological cancers recommendations and guidance on PIFU: British Gynaecological Cancer Society
Ear, nose and throat services guidance and case study: Transforming elective care services: ENT, pp27-29.
Gynaecology services guidance and case study: Transforming elective care services: Gynaecology, pp 29-32.
Inflammatory bowel disease case study: Outpatients: The future – Adding value through sustainability, pp 11-14.
Orthopaedics case study: Transforming musculoskeletal and orthopaedic elective care services, pp 31-32.
Rheumatology case study: University Hospitals of Morecambe Bay NHS Foundation Trust and rheumatology patient leaflet, Royal Berkshire NHS Foundation Trust.
5. 2020/21 Phase 3 planning submission guidance
1. Introduction
This section outlines the submission process for the activity, performance, and workforce planning returns as we plan for the remainder of 2020/21. It includes the list of activity and performance metrics (Appendix 1) and links to the technical definitions for activity, performance and workforce measures.
1.1 Background
The third phase of NHS response to COVID-19 letter from Sir Simon Stevens and Amanda Pritchard issued 31 July 2020 recognises that working across Sustainability and Transformation Partnerships (STPs) and Integrated Care Systems (ICSs) has been essential for dealing with the pandemic and the same is true in recovery. We are asking systems to now plan and deliver the goals set out for Phase 3. The planning metrics reflect this by focusing on service demand as reflected in referrals, acute and diagnostic activity, acute bed capacity, and associated ambitions for elective care, cancer, mental health, and learning disabilities and autism.
1.2 Overview
A fundamental principle of this Phase 3 implementation process is that it will be STP/ICS led.
The process for submission of a small number of core metrics will be as follows:
- Draft numerical submission by 1 September submitted through Strategic Data Collection Service (SDCS) by STPs/ICSs. The accompanying short plan commentary should be submitted by email to the relevant regional planning mailbox (see Section 7).
- Final submission to be made by 21 September. Submissions will again be submitted via SDCS and the relevant regional planning mailbox.
- Submission of system level ‘Local People Plans’, as requested in ‘We are the NHS: People Plan 2020/21 – action for us all’, also to be made by 21 September as a key enabler of Phase 3 STP/ICS plans. Plans should also be submitted by email to the relevant regional planning mailbox (see Section 7) alongside the plan commentary as set out above.
STPs/ICSs are expected to work across their partner organisations to produce plans that consider alignment between CCGs and providers, and correlation between activity and workforce.
1.3 Timetable
| Key tasks | Date |
| Phase 3 letter issued | 31 July |
| Guidance and template issued | 7 August |
| Draft submission of the STP/ICS activity/performance and workforce templates. Draft submission of the associated STP/ ICS activity/ performance/workforce narrative commentary |
1 September |
| Final submission of the STP/ICS activity/ performance and workforce templates. Final submission of the associated STP/ICS activity/ performance/workforce narrative commentary. Submission of system level ‘Local People Plans’ |
21 September |
2. STP/ICS plan collection
2.1 Activity and Performance
The set of planning metrics has been reduced to align with the priorities outlined in the ‘third phase of NHS response to COVID-19’ letter, and can be found at Appendix 1.
Systems are asked to provide a provide a brief commentary on the key strategic actions and assumptions that underpin the activity metrics within the STP/ICS plan template (see Section 5).
STPs/ICSs are asked to provide forecasts of activity and performance measures to cover the last 7 months of the 2020/21 financial year.
The measures being requested in Phase 3 are a subset of those requested as part of previous operational planning rounds, with a few additional amendments.
- Additional outpatient categories to capture face to face and telephone/video attendances separately
- Additional COVID/Non-COVID split for 1+ day non elective attendances
- Cancer data is requested as a count of activity rather than performance measures around waiting times,
2.2 Workforce
We are the NHS: People Plan 2020/21 – action for us all has been published in parallel. It asks that, in response, all systems should develop a Local People Plan. The submission of these Local People Plans is being aligned to the final submission of STP/ICS Phase 3 plans, and they should reinforce and expand on the workforce element of the STP/ICS planning template (see Section 5).
This submission is intended to collect STP/ICS workforce plans for the last 7 months of the 2020/21 financial year. For 2020/21 the workforce plan is profiled for each month, including 2020/21 forecast outturn values.
The sections in the provider input workforce tab of the template are as follows:
- WTE- Substantive, bank and agency WTE forecasts by staff group and by professions, in post.
- Validations: Summary of any errors highlighted, to be cleared before final submission.
2.3 Support available
Support materials will be made available on the NHS Planning FutureNHS collaboration platform as they become available. Regional leads will be the primary link to STPs/ICSs throughout the preparation, review and assurance of operational plans.
3. Detailed guidance
3.1 Commissioner assignment
For the outpatient, admitted patient care and A&E data sets, the Prescribed Specialised Services Identification Rules (PSS IR) Tool and Commissioner Assignment Method (CAM) have been applied within the National Commissioning Data Repository (NCDR) to identify which commissioner is responsible for purchasing each unit of activity.
A number of changes to the PSS IR Tool were introduced in April 2020. NHS Digital have released the latest version of the tool on their website15.
3.2 Activity breakdown by Commissioner/Provider
Although the more detailed commissioner/provider categories are not required as part of this return, there are a few subsets of activity measures which are still requested to ensure a full picture of activity is captured.
CCG based activity will include the following “of which” category:
- Independent Sector (IS) activity – the subset of total activity commissioned by the CCG which will be commissioned directly from the independent sector. This activity is in addition to, and should therefore exclude any:
- activity planned to be delivered by providers covered under the existing nationally agreed contract; or
- activity that would be delivered by those same providers under a re-procured national framework (see the ‘Phase 3 of COVID-19 response and NHS recovery’ letter).
Provider based activity will include the following “of which” category:
- Specialised Commissioning – the subset of total activity which is expected to be commissioned by Specialised Commissioning rather than CCG or other sources.
Independent Sector Activity as part of the national contract / framework
The STP/ICS should set out:
- activity planned to be delivered by providers covered under the existing nationally agreed contract; or
- activity that would be delivered by those same providers under a re-procured national framework (see the ‘Phase 3 of COVID-19 response and NHS recovery’ letter).
This will cover elective and diagnostic activity and is requested as a weekly rather than monthly breakdown. It should not include any activity already recorded under the CCG and Provider input tabs.
This is the only part of the template where IS activity delivered under the national contract / re-procured national framework should be captured. Activity delivered by independent sector providers that are covered by the current national contract should be excluded from the CCG and Provider input tabs.
4. STP/ICS plan template
The template will be configured by each STP/ICS through selecting your organisation from the drop-down menu. You will then be asked to provide data for all measures for your relevant CCGs and providers, which will be used to calculate a total STP/ICS view. Each provider will appear only once, using mapping derived from system control totals.
Data should be recorded by month from September 2020 onwards. April 2020 data will be prepopulated for activity wherever these figures are published and available, however there will be no prepopulated data for performance or workforce measures. Please consult the activity, performance and workforce technical definitions for details of the source data should you wish to consult previously published figures.
4.1 Data sharing
This tab contains important information about how the data submitted in the return will be shared within the system post submission. STPs/ICSs and organisations are asked to take a shared, open-book approach to planning.
To support the development and assurance of plans and to monitor progress, NHS England and NHS Improvement intend to share plans with other NHS organisations and STP/ICS partners, including the production of assurance tools and the pre-population of plans in the final submission template. If you do not consent to the sharing of plans in this way, you can opt out via the relevant tick box in the template.
4.2 Validations
The validation summary provides an overview of all hard validations included in the template. Any validation which has triggered on this page will prevent your file from being submitted. It is important that this page is reviewed prior to submission and any outstanding issues resolved. All validations contain hyperlinks to each cell to reconcile and assist with the error clearance process. Please adhere to these guidelines to help minimise error:
- Avoid dragging and dropping as this can corrupt formulas; please use ‘copy’ and ‘paste special values’ for data extracted from other sources.
- The correct signage and currency must be used – e.g. WTE figures should be rounded to two decimal places. Activity number should be provided as whole numbers etc.
- Ensure when submitting that data is not linked to other workbooks.
- No required cell should be left blank – if no activity or WTE value of the type indicated has been planned for then a 0 should be entered. All data should be entered as numbers, with the exception of comments fields – do not use “N/A”, “NIL” etc.
- Check the validation section summary to ensure all errors are cleared before submission.
4.3 STP/ICS selection
This page allows you to select your STP/ICS and will populate the rest of the return accordingly. All providers and commissioners are assigned to a single STP/ICS, and this configuration cannot be changed within the template. Please record all data relating to a particular organisation, and not just the portion that relates to the parent STP/ICS.
4.4 STP/ICS overview
This tab provides an aggregate view of all data submitted throughout the template, giving an overall STP/ICS position. It also includes some additional calculations and visualisations to assist in the assessment of your data to ensure it reflects your expected position. Please review this tab before submission, with particular reference to:
- the overall STP/ICS position and whether the activity and workforce positions align with each other and the expected financial position
- whether activity levels account for seasonality and meet the expectations laid out in the planning letter and
- the level of alignment in activity volumes between providers and commissioners – although it is not expected that volumes will match an indication is provided on this tab to highlight where provider and commissioner values show a high level of variation.
4.5 CCG input
This tab requires the input of activity and performance profiles for September 2020 to March 2021. Full definitions are in the technical definitions document – wherever possible total fields will be auto-calculated. One table must be completed for each CCG assigned to the STP/ICS.
Validations are present against each data row, with a summary of the status of these validations at the top of the page. Hyperlinks are also used to allow the user to navigate to each individual CCG table.
All activity figures should be provided in whole numbers and take account of seasonality and other factors. Comments boxes are also provided to allow for additional commentary to explain the planned profiles.
4.6 Provider input – activity
This tab is the provider equivalent of the CCG input tab, covering provider activity and performance measures.
Providers are only allocated to a single STP/ICS and data submitted here should represent the entirety of the provider’s expected activity, not just the activity occurring on behalf of CCGs within the STP/ICS.
All activity figures should be provided in whole numbers and take account of seasonality and other factors. Comments boxes are also provided to allow for additional commentary to explain the planned profiles.
4.7 Independent Sector
This tab requires a weekly breakdown of the expected independent sector activity from providers covered by the current national contract, or those same providers under a re-procured framework (once in place) across the STP/ICS footprint. This should not include any activity captured elsewhere in the template (e.g. other locally commissioned arrangements) and relates to elective and diagnostic activity only.
Data should be provided per week, but otherwise follows the definitions for the relevant measures as set out in the technical definitions. All figures must be entered as whole numbers.
4.8 Provider input – workforce
This section collects whole-time equivalent (WTE) forecast information by staff and professional groups for substantive, bank and agency staff numbers.
Substantive staff WTE should be based on WTEs from the electronic staff record (ESR), or similar workforce system, adjusted for:
- secondments in and secondments out;
- recharges in and recharges out; and
- staff provided or received through provider-to-provider contracts.
The all-staff total represents the total planned workforce. The substantive staff section should represent planned substantive staffing levels, while any staffing gaps between the substantive position and total planned workforce should be captured in bank and agency figures to indicate how the shortfall is planned to be filled.
For each heading, the provider is required to provide the planned monthly profile of WTEs for the 2020/21 financial year.
Occupational codes are mapped against each of the roles and have been included as a guide for trusts.
4.9 STP/ICS input
This tab collects information provided for an entire STP/ICS footprint, covering various performance measures not required/appropriate for collection at provider or commissioner level. This tab also includes measures relating to ambulance trusts. As with the provider tab, each ambulance trust has been assigned to a single STP/ICS, but it is expected that the submission will encompass all activity for that ambulance trust, and not just that activity which relates to the STP/ICS.
5. STP/ICS plan commentary
5.1 Commentary on patient activity and workforce numbers in plans
STPs/ICSs need to provide an explanation of the key elements of their delivery plans that drive the patient activity and performance elements of their plans.
In your commentary, please also set out how key services will be restored inclusively to help address health inequalities.
| Area | Areas and assumptions to be covered by commentary |
| Elective |
|
| Non-elective |
|
| Cancer | Key actions and assumptions that underpin planned treatment volumes and waiting time performance
|
| Diagnostics |
|
| Workforce |
|
5.2 Local People Plans
STPs/ICSs are asked to provide their system level response on the priorities set out within ‘We are the NHS: People Plan 2020/21 – action for us all’. This narrative should include:
- a summary of the system response to the actions across the sections of the Plan:
- Looking after our people
- Belonging in the NHS
- New ways of working and delivering care
- Growing for the future
- any key risks to delivery and further support required to meet each of the actions.
The actions set out within the Local People Plan should be fully aligned with the Phase 3 workforce template and narrative submissions as set out above.
6. Submission process
Each STP/ICS will submit a single completed template to SDCS. This system will then collate the returns and produce extracts post submission.
STPs/ICSs are requested to submit the accompanying plan commentary in a word document at the same time alongside the SDCS template. The commentary should be submitted by email to the regional planning mailbox as set out in Section 7. Local People Plans should also be submitted by email to the regional planning mailbox.
All submitters for the STP/ICS should receive an email from SDCS service shortly before the window opens, to confirm they are the correct submitter. If you do not receive this invitation at least 1 d y before the window opens please contact the NHS Digital Data Collections team to request a log in16.
Data can be submitted at any point once the submission window is open via the SDCS website17
Guidance on the SDCS system can be accessed on the NHS Digital website18
Wherever possible, on submission validation will be used to ensure plans are complete and that files which breach hard validations cannot be submitted (e.g. missing or invalid data). Please ensure that you review the validation section of your return before submission – this will indicate any remaining errors which would cause your file to be rejected.
6.1 Sign off
The template does not include details of the internal sign off process within each STP/ICS. It is assumed that by submitting the return the STP/ICS confirms that the plan is a reflection of the collective intentions of the system for the rest of the year, that activity and workforce plans align and that the plan is agreed by all STP/ICS partners.
16 The data collections team can be contacted at data.collections@nhs.net
17 https://datacollection.sdcs.digital.nhs.uk/
18 https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/strategic-data-collection-service-sdcs
7. Key planning contacts and resources
7.1 Regional contacts
STPs/ICSs should initially contact their region for advice on planning, using the contact details below:
| Location | Contact information |
| North East and Yorkshire | england.nhs-NEYplanning@nhs.net |
| North West | england.nhs-NWplanning@nhs.net |
| East of England | england.eoe2021operplan@nhs.net |
| Midlands | england.midlandsplanning@nhs.net |
| South East | england.planning-south@nhs.net |
| South West | england.southwestplanning@nhs.net |
| London | england.london-co-planning@nhs.net |
7.2 National and wider technical issues
| Subject area | Contact information |
| SDCS collection portal | data.collections@nhs.net |
| NHS National Planning Team – activity and performance, workforce and general planning queries | england.nhs-planning@nhs.net |
| Integrated Planning Tool | england.covid-ipt@nhs.net |
7.3 FutureNHS collaboration platform
General updates and resources will be provided on the NHS Planning FutureNHS collaboration platform throughout the Phase 3 planning round.
You will need a FutureNHS account to access pages, and can get this at: https://future.nhs.uk/connect.ti/system/home following the registration process outlined.
7.4 Integrated Planning Tool
An Integrated Planning Tool (IPT) has been developed to support STPs/ICSs in completing Phase 3 returns.
The IPT brings existing data and models together into a single system for planning. It is designed to assist STPs/ICSs in developing local plans and understanding the resource constraints and implications of planned activity.
How to access and further information
For further information regarding the tool, details on how to access and support sessions being made available please refer to the NHS COVID-19 Data Store FutureNHS collaboration platform.
8. Information governance
Information governance requirements on the collection of data from acute, specialist, mental health, community, and ambulance trusts relating to annual operational and strategic planning, intended data uses and further sharing are included in the relevant templates.
Data will be shared within NHS England and NHS Improvement. Any further data sharing will be subject to an opt-out clause as detailed in the appropriate submission template.
Further support and information on information governance can be provided by: england.ig-corporate@nhs.net
Appendix 1: Activity and performance metrics
| Measure Reference | Sub Category | Measure Name |
| E.A.3 | IAPT Roll Out | |
| E.B.18 | Number of 52+ Week RTT waits | |
| E.B.3a | RTT Waiting List | |
| E.B.26 | E.M.26a; E.M.26b; E.M.26c; E.M.26d; E.M.26e; E.M.26f |
Diagnostic Test Activity |
| E.B.30 | Urgent cancer referrals | |
| E.B.31 | Cancer treatment volumes | |
| E.B.32 | Number of patients waiting 63 or more days after referral from cancer PTL | |
| E.H.9 | Improve access to Children and Young People’s Mental Health Services (CYPMH) | |
| E.H.12 | E.H.12a; E.H.12b | Inappropriate adult acute mental health Out of Area Placement (OAP) bed days |
| E.H.13 | People with severe mental illness receiving a full annual physical health check and follow up interventions | |
| E.H.15 | Number of women accessing specialist perinatal mental health services | |
| E.H.17 | Number of people accessing Individual Placement and Support | |
| E.H.27 | Number of people receiving care from new models of integrated primary and community care for adults and older adults with severe mental illnesses | |
| E.K.1 | E.K.1a; E.K.1b; E.K.1c |
Reliance on inpatient care for people with a learning disability and/or autism |
| E.K.3 | Annual Health Checks delivered by GPs for those on the LD register | |
| E.M.7 | E.M.7a; E.M.7b | Referrals made for a First Outpatient Appointment (General & Acute) |
| E.M.8-9 | E.M.8c; E.M.8d; E.M.9c; E.M.9d | Consultant Led Outpatient Attendances (Specific Acute) |
| E.M.10 | E.M.10a; E.M.10b | Total Elective Spells (Specific Acute |
| E.M.11 | E.M.11a; E.M.11c; E.M.11d | Total Non-Elective Spells (Specific Acute) |
| E.M.12 | E.M.12a; E.M.12b | Type 1-4 A&E Attendances |
| E.M.23 | Ambulance conveyance to ED | |
| E.M.26 | General and Acute Bed Occupancy |
6. COVID-19 data collections: changes to weekend collections
As part of our COVID-19 response, we have been running a number of COVID-19 related data collections over the weekend. The reduction in the national incident level for the COVID-19 response from level 4 to level 3 stated that weekend collections would be stopping from Saturday 8 August onwards – here are more detail on these changes.
In the event of the incident increasing in severity once more, we may need to stand up working on a 7-day per week basis and would be in touch at that point.
For most of the weekend collection we will open the collections for submission on a Saturday/Sunday as normal, but instead of the collection closing that same day, it will remain open until the deadline for the Monday collection. This allows organisations to make no submissions over the weekend (and submit Saturday, Sunday and Monday submissions on a Monday morning), or to continue to upload data over the weekend. This excludes the reporting of deaths, which will continue daily.
The table below list the collections that are covered by this change and, for each one, describes the way in which weekend data will be collected going forwards:
| Collection name | Changes to weekend collections |
| COVID-19 daily sitreps (including NHS Acute, NHS MHLDA, IS Acute and IS MHLDA) | Saturday and Sunday collections will open at 08:00 as usual on Saturday/Sunday morning but will remain open until 11:00 on Monday morning. |
| Daily discharge collections (including acute and community) | Collections in respect of Saturday and Sunday would open at the normal times but would remain open for submission until Monday. |
| UEC sitrep | Collections in respect of Saturday and Sunday would open at the normal times but would remain open for submission until Monday. |
| NHS111 MDS daily | We would not open collections on a Saturday or Sunday. The weekly MDS data already collected on a Monday will be used instead. |
| NHS111 staffing daily | We would not open collections on a Saturday or Sunday. |
| Daily deaths data | Continue daily |
