Modern general practice model
Modern general practice
General practice is the bed rock of the NHS. In response to the twin challenges of rising volume and increasing complexity of need, a wide range of general practices across England have innovated and have created the principles of ‘modern general practice’. These elements have been set out in NHS England’s Delivery plan for recovering access to primary care.
Modern general practice is the foundation of a transformation journey to better align capacity with need, improve patient experience and improve the working environment for general practice staff by:
- optimising contact channels; offering patient choice of access channel (telephone, online and in person) via highly usable and accessible practice websites, online consultation tools and improved telephone systems.
- structured information gathering at the point of patient contact (regardless of contact channel) to understand what is being asked of the service.
- using one care navigation (and workflow) process across all access channels to assess and prioritise need safely and fairly, and to efficiently get patients to the right healthcare professional or service, in the appropriate time frame (including consideration of continuity of care) moving away from a ‘first come first served approach’.
- better allocating existing capacity to need, making full use of a multi-professional primary care team, community services and ‘self access’ options where appropriate, and helping GPs and practice staff to optimise use of their time to where it’s needed most.
- building capability in general practice teams to work together and to access, understand and use data, digital tools and shared knowledge to lead, plan, implement, improve and sustain change.
Modern general practice uses digital tools, transformation support, funding and incentives as part of a system wide delivery plan, which also includes expansion of clinical pharmacy and improvements across the primary care-secondary care interface to support general practice sustainability and primary care transformation.
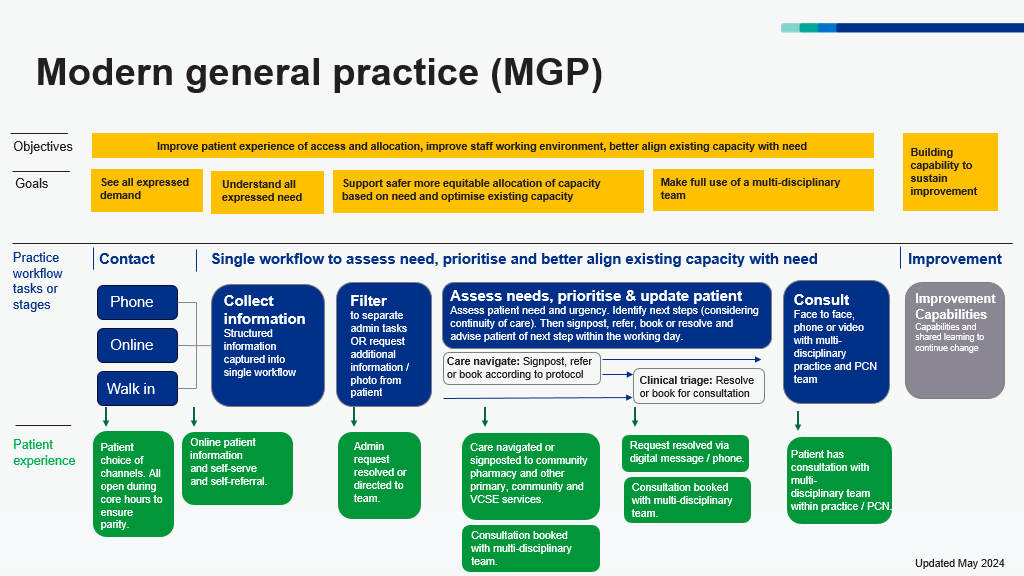
Figure 1: modern general practice model (updated May 2024)
Figure 1 above shows that the overall objectives of the modern general practice model are better alignment of capacity with demand, an improved working environment for staff and improved patient experiences. There are 3 access routes to general practice for patients which are telephone, online and walk in. Information is collected at the point of contact to help care navigate patients to the right service at the right time, based upon need and not first come, first served.
What other support is available?
Practices can access nationally-funded flexible, practical, hands-on support to help them with modern general practice from NHS England’s national General Practice Improvement Programme by contacting their integrated care board.
This support is available to a proportion of practices identified as most benefitting by their integrated care board, alongside locally available offers, as part of the transition to system-owned delivery of support.
If you want to learn more about modern general practice and the General Practice Improvement Programme you can watch this video from Dr Minal Bakhai, GP and our National Director for Primary Care Transformation, on FutureNHS (requires login).
There is also a set of 5 ‘how to’ guides to support general practice teams.
They provide know-how and learning from practices and primary care networks across the country about tested new systems, processes and approaches that are helping the transformation to modern general practice. They support all practices and primary care networks to adapt this shared knowledge to their local context and realise the benefits more quickly and easily. In particular, they help ensure patients get the care they need, from the most appropriate health professional, first time.
The guides:
1. How to improve care navigation in general practice (May 2024)– helps practices create or improve a single care navigation model or process so patient requests by phone, online or in person are directed to the right care professional first time. It helps practices make full use of a multi-professional practice team and other local health services. The guide also helps practices to effectively integrate online consultation, messaging and appointment booking tools into their practice workflow. This guide is accompanied by a skills matrix template tool.
2. How to align capacity with demand in general practice (May 2024) – helps practices measure and understand daily patterns of patient contacts and type of need in order to forecast how much and what type of capacity is needed on any given day. Practices can use this data to review rotas and clinics, to help smooth peaks and troughs and better align capacity to need, giving practice teams back a sense of control.
This guide is accompanied by the following tools:
- Appropriate appointment data collection sheet
- Demand and capacity data spreadsheet
- Digital triage calculator
3. How to improve telephony journeys in general practice (May 2024) – helps practices shorten call queues and improve patient journeys using call-backs, recorded messages, signposting, keypad and voice options.
4. Creating highly usable and accessible GP websites for patients (September 2022) – helps improve online journeys for patients via GP websites and apps, making it easier for patients to request the help they need, including using online forms to request medical care, ordering repeat prescriptions online and accessing other administrative help. This guide is accompanied by the GP website benchmarking and improvement tool.
5. How to improve care-related processes in general practice (May 2024) – helps practices manage common processes more efficiently; including new and repeat prescriptions, long-term condition recalls and new patient registrations.
Understanding demand and capacity
To establish a modern general practice model, it is essential for practices to have as complete a view as possible of all demand coming into the practice by all routes and to understand the nature and pattern of this demand, eg across different days of the week and at different times of year.
It is also important for practices to understand the capacity available in terms of staff time and skills. It is then possible to design and implement processes to match capacity to demand more effectively.
Improving the experience of telephoning the practice and using online access routes
The modern general practice model involves providing a smooth, equitable experience of access to patients across phone, online and walk-in routes.
Supporting practices to move to and optimise the capability of cloud-based telephony is essential to help provide a better experience for patients (eg so patients can be provided with queue position and callback options) and to enable practices to proactively manage peaks in demand through real time data monitoring and to support evidence-based service decisions.
Well-designed practice websites are also critical and need to give clear information on how to request help and what steps patients can take for themselves.
Online forms (provided via ‘online consultation tools’) should be available via the practice website and via tools like the NHS App to provide an easy route for patients to explain what they need and to request support.
Improvements to other tools and integration of digital services are also important to the model to allow increased self-service and more streamlined flows between different services.
Enhancing navigation and triage processes
The modern general practice model moves away from the 8am phone call queue and ‘first come, first served’ process for allocating appointments.
Instead, the model requires consistent structured information to be collected at the point of contact – to let the practice know about symptoms, ask a question, make a request or follow up about something – with patients either providing this information via an online form or to reception staff who capture the information about their needs.
Patient needs can then be consistently assessed and prioritised (triaged), allowing practices to provide patients with the most appropriate care or other response, from the right member of the practice team, including signposting or referring patients to other appropriate services.
The ability to better allocate patients to the right health professional or service supports effective use of all staff time and skills, including staff employed through the Additional Roles Reimbursement Scheme (ARRS).
It also supports improved ability and capacity to provide continuity of care for those that would benefit most, including vulnerable patients and those with long-term conditions.
The use of different consultation modalities, including text or online messages, is also important to facilitate flexible working for staff (which supports retention) and provides a variety of options for patients to receive care and advice in the most effective way depending on their needs.
Management of non-patient-facing practice workload
The modern general practice model gives practice staff better control over their workload with demand more consistently understood and managed, and the consistency of processes and workflows improved.
Alongside these changes, other improvements can also be made to streamline non-patient-facing processes in the practice, increase efficiency and reduce burden on staff.
This could also improve the trust that patients hold in practices as they will receive the care they need when they need it, from the person best suited to help them, preventing wasted visits and multiple calls to the surgery.
The General Practice Improvement Programme helps practices and primary care networks (PCNs) to implement the modern general practice model by supporting change to be made and by providing tools, guidance and resources to make the change easier – building on what other practices have learnt and developed.
Where practices have innovated and created the different elements of the modern general practice model, these have been collated and codified and are being shared more widely, helping practices and PCNs make changes more easily and realise the benefits more quickly.