Executive summary
This annex provides details of performance and work being undertaken to improve services in our wider priority operational areas.
Primary care and community health services
1. As at the end of July 2024, there have been 380.8 million GP appointments in the previous 12 months. This includes COVID-19 vaccinations and Primary Care Network appointments, and is an increase of 73.5 million appointments (23.9%) compared to 2019/20.
2. The majority (51.6%) of all appointments took place on the same day or day after booking, an increase of 0.6 percentage points from July 2023.
3. Nearly 9 out of ten appointments that were not usually booked in advance (88.3% took place within 14 days of booking) which is an increase of 1.2 percentage points from July 2023.
4. Progress is being made against the ambitions in the Primary Care Access Recovery Plan and its goal of making it easier and quicker for patients to get the help they need:
- in June 2024, just over 4 million repeat prescriptions were ordered through the NHS App against a target of 3.5 million by March 2025
- in June 2024, there were 20.5 million record views through the NHS App against a target of 15 million views per month by March 2025
- self-referrals across all pathways reached 225,360 in May 2024 against a target of 225,971 per month by March 2025
- uptake of Pharmacy First, and other expanded services, has been positive and activity continues to grow
5. A Health Insight Survey was launched on 23 July with the first wave published on 12 September, providing patient experience on GP access, dentistry, community pharmacy, and the elective waiting list. We are currently developing our approach to share insights with regional teams to support improvement activity. The survey will run every 4-weeks, so the next publication will be available on the 10 October. The first wave had 103,990 respondents:
- 47.1% of the respondents had tried to contact their GP practice in the last 28 days. Of these respondents 76.8% were able to make contact on the same day and of these, 60.9% found it easy to contact their GP practice and 67.4% had a good overall experience with their GP practice.
- 52.1% of respondents reported having an NHS dentist compared to 13.5% who reported having no dentist.
6. In July 2024, 1,097,192 referrals were waiting for a first treatment from a community health service.
7. The largest waiting lists in July 2024 were for adult musculoskeletal services (342,593), children and young people’s community paediatric service (132,962) and adult podiatry and podiatric surgery (127,984).
8. The services with the largest percentage of the total waiting list waiting over 52 weeks in July 2024 were children and young people (CYP) community paediatric service (26% waiting over 52 weeks), CYP occupational therapy (8%), and CYP speech and language (7%). To address this, work is underway on data definitions of service lines, to prepare for a potential national standard. In addition, we are looking to conduct a deep dive for Community Paediatrics and CYP community therapies to give a baseline position and understanding of these services, including quantitative data on what is driving demand, workforce models, service pathways, capacity issues.
Mental health
9. Mental Health remains one of the NHS’s top priorities and we are committed to improving services and addressing the long-standing treatment gap. The NHS continues to deliver at pace against public commitments despite pressures remaining across the sector through increased demand and prevalence, and capacity constraints.
10. The access to transformed models of community mental health (CMH) commitment with patients accessing services aligned with Primary Care Networks (PCNs) for new integrated models of community mental healthcare is being achieved with 467,978 people receiving two or more contacts as of June 2024.
Access to transformed community mental health services
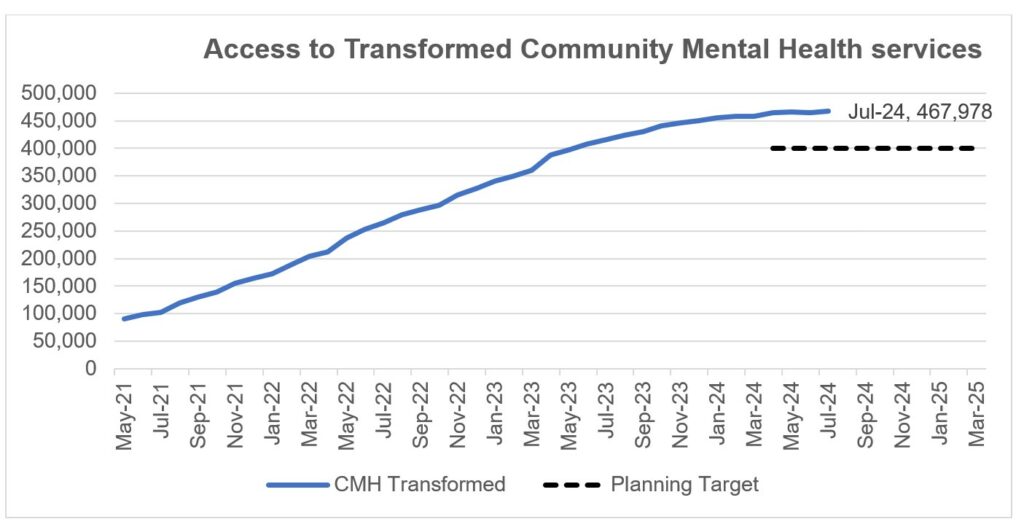
11. According to interim contact-based data, as of April 2024, 10% of people waiting for a second contact in Adult CMH services had been waiting at least 116 weeks compared to 100 weeks in December 2023. Those waiting for their second contact will include people with severe mental illness (SMI), and people seeking support for self-care and neurodevelopmental conditions.
12. In Autumn 2024, NHS England will publish full CMH metrics, which will begin to show the percentage of people receiving meaningful help within four weeks of referral in Adult CMH and CYP services. We expect a focus on data quality improvement in 2024/25 to enable more accurate data from April 2025 onwards.
13. In 2024/25 the NHS committed to increasing the number of adults and older adults completing a course of treatment for anxiety and depression via NHS Talking Therapies to 700,000, with at least 67% achieving reliable improvement and 48% achieving reliable recovery. In July 2024, 62,036 adults completed a course of treatment, with reliable improvement of 66.9% and reliable recovery of 47.3%.
14. Access to Individual Placement and Support (IPS) services has increased, with over 38,000 people reported to have accessed an IPS service in the 12 months to July 2024, compared to 30,000 in the year to July 2023. To further increase access, NHS England is working with IPS Grow (a voluntary, community and social enterprise organisation supporting delivery of IPS) to disseminate learnings from five pilot sites aiming to increase referrals from primary care, as well as increase recruitment and retention of staff in the IPS workforce.
15. The Urgent and Emergency Mental Health pathway continues to be under significant pressure, experiencing high bed occupancy (95–97%) since May 2022. Improving inpatient flow is a key priority in 2024/25. NHS England is supporting systems to improve flow and reduce out of area placements, with support on key issues including data and good practice. Joint working is underway with the Get It Right First Time programme to offer additional support to challenged systems.
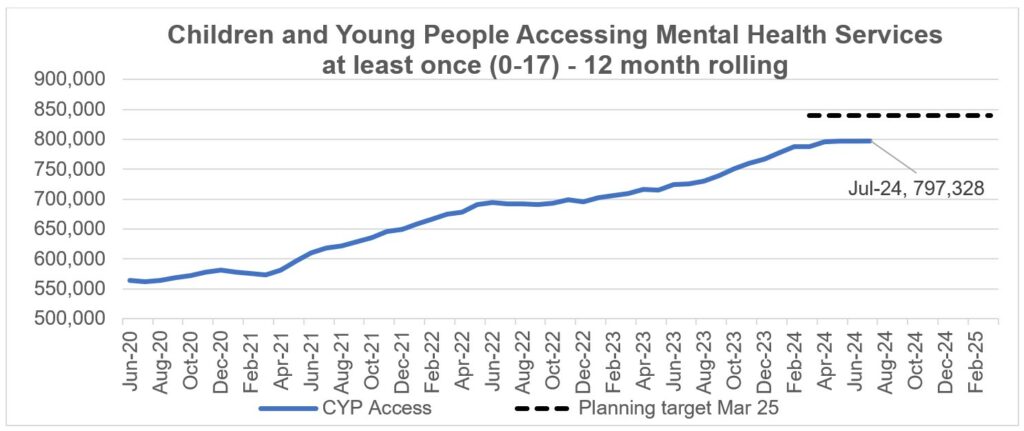
16. As of July 2024, 797,328 CYP aged 0–17 received support (1+ contacts) from an NHS-funded service.
17. CYP eating disorder (ED) pathways continue to be challenged. As of June 2024, 70% of routine CYP ED referrals were seen within four weeks and 67.1% of urgent referrals were seen within one week. NHS England continues to help providers to improve the quality and completeness of data submissions which aims to support improved reporting of performance against the 95% access and wait standard.
Children and young people accessing mental health services at least once (0-17) – 12 month rolling
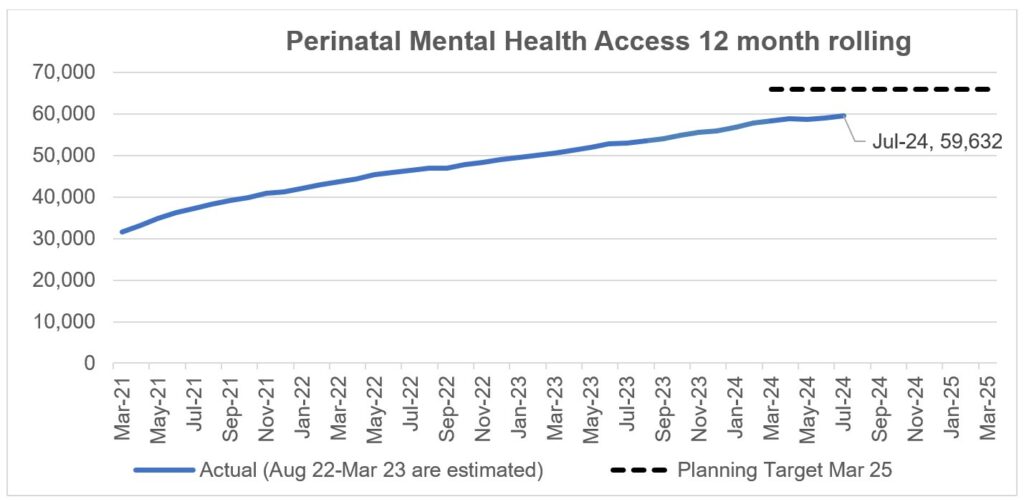
18. Access to specialist perinatal mental health (PMH) and maternal mental health services (MMHS) has seen steady growth since March 2021. In the 12 months to July 2024, 59,632 women accessed these services which is an increase from 58,991 in the 12 months to June 2024.
Perinatal mental health access 12 month rolling
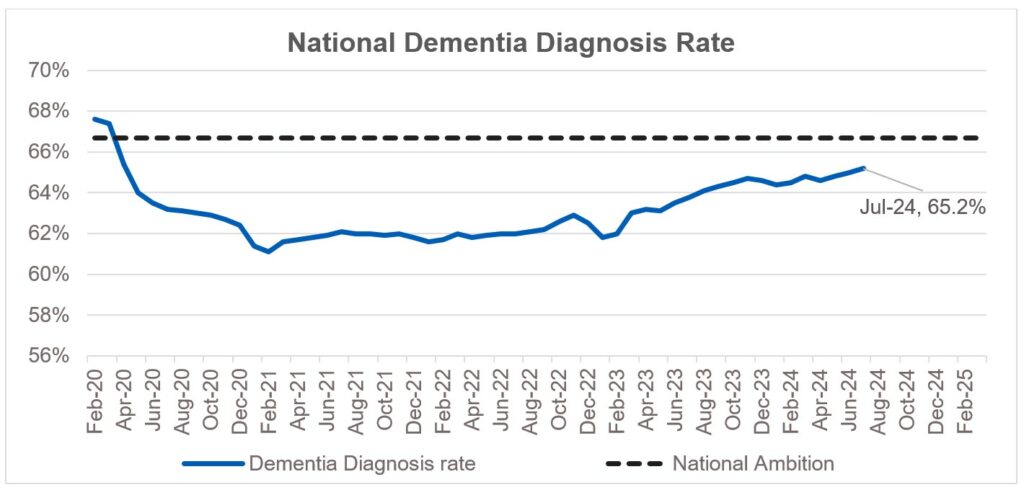
19. The dementia diagnosis rate (DDR) has been steadily improving since January 2023; for July 2024 the DDR is 65.2% against the ambition of 66.7% by March 2025 which is an increase of 0.2% compared with June 2024 (65%). The number of people with a recorded dementia diagnosis has reached a record high at 490,000. NHS England has funded an evidence-based improvement project to fund two trusts in each region to pilot the DiADeM (Diagnosing Advanced Dementia Mandate) tool designed to improve the diagnosis of dementia in care homes. All pilots completed at the end of May 2024 and learning will be shared later in 2024/25.
National dementia diagnosis rate
20. NHS England has committed to developing reporting against the nationally-held data and information set out in the Patient and Carer Race Equality Framework (PCREF) for 2024/25.
Learning disabilities and autism
21. There continues to be a steady reduction in the number of adults with a learning disability or who are autistic in a mental health inpatient setting. Provisional data for July 2024 shows there were 1,835 adult inpatients, a reduction of 4.7% from the inpatient population as of March 2024.
22. As of July 2024, provisional data shows there were 190 inpatients under the age of 18 with a learning disability or who are autistic. In line with the trends seen for adult inpatients, since March 2017 there has been a decrease in under 18 inpatients with both a learning disability and autism, and those with a learning disability only, but an increase in the number of patients with autism only.
23. There has been an increase in the number of people receiving an annual health check compared to the same period last year. Between April and July 2024 18.6% of people on GP learning disability registers received a check, compared to 16.8% between April and July 2023. This equates to over 8,800 more checks being completed. We remain on trajectory to achieve the 75% annual health check target by March 2025.
Proportion of people aged 14+ with a Learning Disability on the GP register receiving annual health check
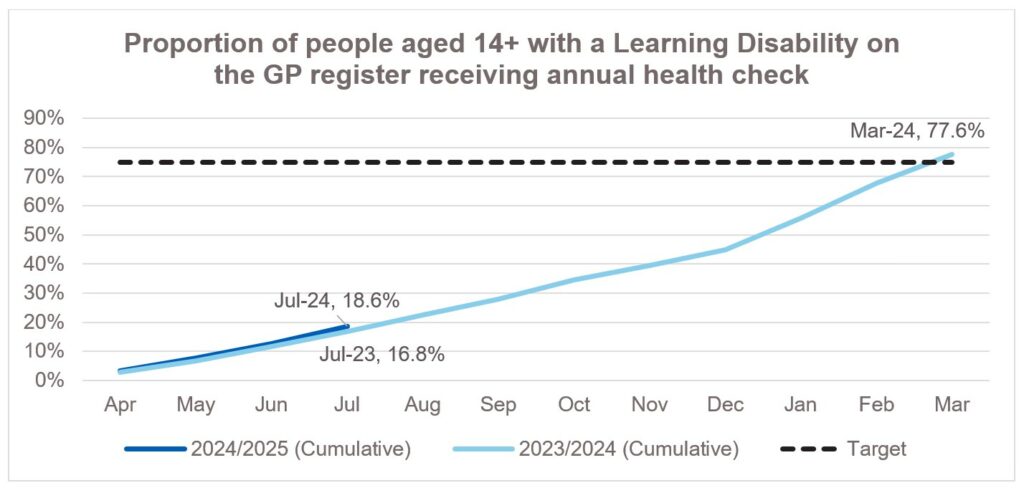
Proportion of people aged 14+ with a learning disability on the GP register receiving annual health check
24. In addition, work is continuing to increase the size and accuracy of GP learning disability registers. As of July 2024 there were 335,552 people on registers aged 14 and over, representing an increase of 16,076 (5%) compared to the position in July 2023.
Children and young people
25. The national inpatient Paediatric Early Warning Score (PEWS) continues to be rolled out across all paediatric inpatient settings, ensuring early identification of deterioration in children. Recently, an electronic audit tool has been introduced for sites still using paper-based PEWS charts, facilitating immediate and ongoing evaluation of its impact. Phase 2 of the PEWS programme is progressing with the development of an Emergency Department prototype chart.
26. NHS England remains focused on delivering its commitments related to Children and Young People (CYP), including treating over 3,000 children and young people in Complications of Excess Weight (CEW) clinics. These clinics have exceeded the target of treating 1,000 children annually for severe obesity-related complications.
27. Progress is being made against the CYP priorities set out in 2024/25 planning guidance though services remain pressured:
- as of July 2024, over 290,000 children were on waiting lists for community services. 11 out of the 17 services we regularly track have waiting lists exceeding 52 weeks
- the longest waits are reported for speech and language therapy and community paediatrics, whilst the demand for autism assessments is exceeding capacity
- paediatric intensive care units (PICU): PICUs have been operating at over the commissioned 80% capacity for 8-10 months of the year, leading to significant pressures on staffing, morale, and the ability to provide training and maintenance during quieter periods
28. Health Inequalities: NHS England continue to make progress against the CYP CORE20Plus5 clinical areas.
- asthma – reduction in admissions
- diabetes – greater access to technology
- we continue to pilot epilepsy nurses
- dental extractions – we continue to support local systems to reduce waiting times
Prevention and long-term conditions
29. An expression of interest process has been completed to identify sites to take part in proof-of-concept pilots implementing blood pressure check services in wider primary care settings. 19 integrated care boards (ICBs) have been successful in securing funding, with nine optometry and 10 dental case finding pilots supported. Some sites have begun to offer blood pressure checks, and all sites are expected to have commenced checks by December 2024. The pilots will run until Summer 2025 and the evaluation partner will report on their findings by the end of August 2025.
30. Over 1.6 million referrals have been made into the NHS Diabetes Prevention Programme to date. The NHS Type 2 Diabetes Path to Remission Programme is now available across to the whole of England, and over 28,000 referrals have been made to date. This initiative supports participants to improve their diabetes control, reduce diabetes-related medication and wherever possible to put their type 2 diabetes into remission.
Recovery support programme
31. The Recovery Support Programme (RSP) provides national mandated intensive support to trusts and ICBs in NHS Oversight Framework segment 4 that have complex, deep-seated concerns around leadership, governance, finance, patient safety, quality, or performance. The Programme now has 21 trusts (4 legacy special measures) and 3 ICBs enrolled.
Publication reference: public board paper (BM/24/35(i)(Pu)

