Introduction
This document presents the results of all NHS trusts and NHS foundation trusts (termed ‘providers’) in England. The Department of Health and Social Care (DHSC) uses the provider sub-consolidation as part of the DHSC group accounts. We are very grateful to NHS providers for their co-operation in reporting their data to us.
These accounts are presented separately from those of NHS England as NHS England is not the parent body of NHS trusts and NHS foundation trusts.
The introduction describes the legal requirements for NHS trust and NHS foundation trust accounts and organisational changes in the provider sector in 2021/22 and 2022/23.
NHS trusts
Paragraph 11A(3) of Schedule 4 of the National Health Service Act 2006 (the 2006 Act) (as inserted by Section 87 of the Health and Care Act 2022) requires each NHS trust to prepare annual accounts for each financial year ending 31 March. These annual accounts must be audited by auditors appointed by the NHS trust.
NHS trusts that cease to exist as separate legal entities during the year (including on authorisation as an NHS foundation trust) prepare accounts for their final period as directed by the Secretary of State and have them audited.
NHS foundation trusts
Paragraph 25 of Schedule 7 to the 2006 Act (as amended by paragraph 31(3) of Schedule 5 to the Health and Care Act 2022) requires each NHS foundation trust to prepare annual accounts for the period beginning on the date it is authorised and ending the following 31 March and for each successive 12-month period. These annual accounts must be audited by auditors appointed by the NHS foundation trust’s council of governors. The trust must lay a copy of the accounts, and any auditor’s report on them, before Parliament and send them to NHS England.
NHS foundation trusts that cease to exist as separate legal entities before the end of the year continue to prepare accounts for their final period as directed by NHS England and have them audited, but do not present them to the council of governors.
Basis of preparation for consolidated NHS provider accounts
Section 65Z4 of the National Health Service Act 2006 (as inserted by Section 14 of the Health and Care Act 2022) requires NHS England to prepare, for each financial year, a set of accounts that consolidates the annual accounts of all NHS trusts and NHS foundation trusts. The Secretary of State has given directions on the content and form of these consolidated accounts and the principles to be applied in preparing them. The Comptroller and Auditor General is required to examine, certify and report on the consolidated NHS provider accounts and send a copy of his report to the Secretary of State and NHS England. NHS England is required to lay the consolidated provider accounts and the Comptroller and Auditor General’s report before Parliament.
Organisation terminology
NHS Improvement, as the operating name for the NHS Trust Development Authority and Monitor legal entities, was the organisation responsible for the oversight of NHS providers during the first quarter of 2022/23. From 2019, NHS Improvement operated jointly with NHS England. On 1 July 2022 the NHS Trust Development Authority and Monitor were abolished and their functions transferred to NHS England. These consolidated accounts reference other documents issued by NHS England: in some cases these will have been issued by predecessor legal bodies. Documents issued by the NHS Trust Development Authority and Monitor before they were abolished are treated, from 1 July 2022, as having been issued by NHS England.
Changes in legal status of NHS providers
These consolidated NHS provider accounts incorporate the results of all NHS trusts and NHS foundation trusts. Entities for which legal status changed in 2021/22 or 2022/23 are as follows:
| NHS trusts | NHS foundation trusts | All providers | ||
|---|---|---|---|---|
| 1 April 2021 | Number of providers at start of year Includes dissolution of Brighton and Sussex University Hospitals NHS Trust on acquisition by University Hospitals Sussex NHS Foundation Trust | 70 | 145 | 215 |
| 1 June 2021 | Dissolution of North West Boroughs Healthcare NHS Foundation Trust on acquisition by Mersey Care NHS Foundation Trust. |
| -1 | 214 |
| 1 October 2021 | Dissolution of The Pennine Acute Hospitals NHS Trust on acquisition by Salford Royal NHS Foundation Trust; entity renamed as Northern Care Alliance NHS Foundation Trust. | -1 |
| 213 |
| 31 March 2022 | Number of providers at end of year | 69 | 144 | 213 |
| 1 April 2022 | Dissolution of Northern Devon Healthcare NHS Trust on acquisition by Royal Devon and Exeter NHS Foundation Trust; entity renamed as Royal Devon University Healthcare NHS Foundation Trust. | -1 |
| 212 |
| 31 March 2023
| Number of providers at end of year | 68 | 144 | 212 |
Review of financial performance of NHS providers
| 2022/23 | 2021/22 | |
|---|---|---|
| Number of NHS providers in existence during the year |
212 |
215 |
| Surplus/(deficit) before impairments and transfers | (£457 million) | £562 million |
| Number of NHS providers recording a deficit before impairments, transfers and consolidation of charitable funds | 105 | 74 |
| Capital expenditure (purchases and new or modified leases of property, plant and equipment and intangible assets – accruals basis) See ‘capital expenditure’ section below for information on impact of new leasing accounting standard in 2022/23. | £7,803 million | £6,917 million |
The NHS made substantial progress on many of its strategic priorities for 2022/23, including delivering record numbers of urgent cancer diagnostic tests and significantly reducing long waits for elective care, nearly eliminating two year waits by July 2022, but there was substantial pressure on emergency performance. The progress against priorities was delivered against an ongoing environment of high levels of COVID infection, industrial action impacting on productivity and increased costs due to inflation.
The Health and Care Act 2022 established 42 integrated care boards on 1 July 2022, replacing 106 clinical commissioning groups. Further information on the role of integrated card boards can be found on the NHS England website.
The implementation in the NHS of a major new accounting standard for leasing means there are significant changes to financial reporting this year. IFRS 16 Leases brings on balance sheet the majority of leased assets, materially increasing non-current assets and borrowings across NHS providers. Lease payments previously charged to expenditure as incurred have been replaced with depreciation and interest charges.
More information on the implementation of IFRS 16 is given in accounting policy 1.10 and note 14.6 to the financial statements.
The provider sector delivered a net deficit before impairments and gains and losses on transfers by absorption for the year ended 31 March 2023 of £457 million (2021/22 £562 million net surplus) and held cash of £12.8 billion as at 31 March 2023 (31 March 2022:
£15.6 billion). NHS providers are not required to break even in every year. Providers are required to exercise their functions in line with the relevant plans of the integrated care board to achieve balance across the integrated care system as a whole, allowing for local allocation and prioritisation of available resources.
The following table shows the profile of NHS providers that made up the sector during 2022/23. Providers are classified by their principal services but they may also provide other services.
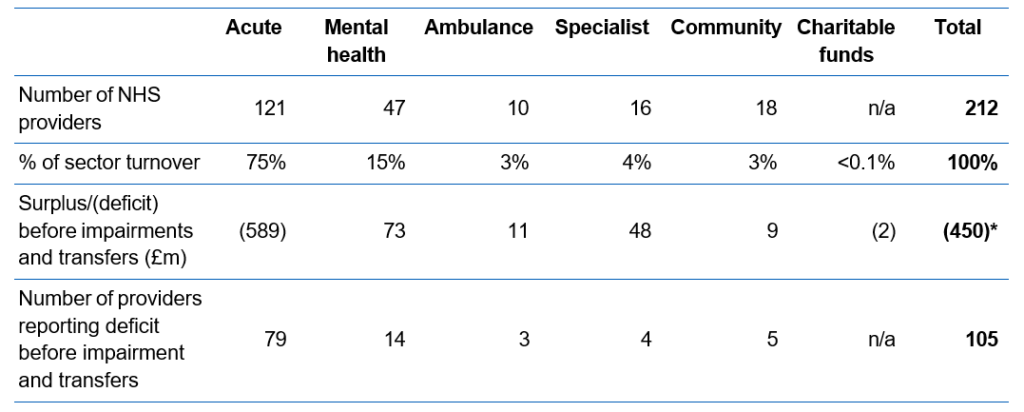
* Following the initial application of IFRS 16 Leases, lessee and lessor accounting treatments are no longer aligned. The aggregate of the surplus/(deficit) from individual provider accounts does not equal the consolidated deficit in these accounts due to the impact of eliminating lease arrangements between NHS providers.
The results for the year showed that, excluding the consolidation of charitable funds, 107 NHS providers (50%) (2021/22: 141 (66%)) delivered a surplus or broke even and 105 providers (50%) (2021/22: 74 (34%)) reported a deficit before impairments and transfers by absorption. The gross deficit of all providers in deficit increased from £141 million in 2021/22 to £1,009 million in 2022/23. Of the 141 trusts that reported a surplus in 2021/22, 57 (40%) reported a deficit in 2022/23, while 23 (31%) of the trusts reporting a deficit in 2021/22 reported a surplus in 2022/23.
Figure 1 shows the distribution of providers’ surplus or deficit for 2022/23 and 2021/22. The two lines are plotted independently.
Where NHS charitable funds are locally deemed to be controlled by an NHS provider, the financial results of the charities are consolidated in these accounts. 44 NHS providers consolidated charitable funds, contributing an aggregate deficit of £2 million (2021/22: 43 providers consolidated a £12 million surplus) and net assets of £348 million (31 March 2022: £352 million).
The NHS Oversight Framework sets out the principles for system accountability and improvement support where appropriate. Providers who are in segment 4 of the oversight framework are entered into the Recovery Support Programme (RSP). This programme provides focused and integrated support to systems as well as individual organisations. As at 31 March 2023, 13 providers reporting a deficit were also receiving support in the RSP (31 March 2022: 7 providers). This support may not be finance related in all cases.
208 of 212 NHS provider financial statements received unqualified true and fair audit opinions at the time of finalising these accounts on 15 January 2024 (2021/22: 195). The results of two providers have been consolidated based on unaudited accounts information provided by the Trust. Further information on these two providers is provided in note 31 to these consolidated financial statements. The impact of current constraints in the local audit environment is discussed in the annual governance statement. University Hospitals of Leicester NHS Trust received a modified audit opinion qualified in two respects: evidence for plant and equipment asset existence, and the impact of additional qualifications in previous years’ financial statements affecting comparative figures. More information is provided in note 32 to the financial statements.
One provider (2021/22: 19) received an opinion qualified for a limitation of scope in respect of inventories where sufficient assurance could not be obtained over material inventory balances at a previous year end. This arose because restrictions on movement in response to the COVID-19 pandemic prevented some providers from performing year-end inventory counts and/or auditors from attending such counts in previous years. The impact is not material to these consolidated accounts.
All providers have prepared financial statements on a going concern basis. HM Treasury’s Financial Reporting Manual (FReM) defines that a public sector body will be a going concern where continuation of the provision of services is anticipated in the future. The same definition is applied by NHS providers in preparing their financial statements. The accounting policies contain our going concern assessment for these consolidated accounts.
Operating income
In the year to 31 March 2023, 212 NHS providers generated total operating revenues of
£121.2 billion, an increase of £8.6 billion (7.6%); a real terms increase of 0.9% when adjusted for inflation. The increase includes additional funding for ‘agenda for change’ pay uplifts in 2022/23.
NHS-led provider collaboratives became more established during 2022/23, providing a new model of commissioning of mental health, learning disability and autism services to bring specialist care into a community setting. Increased income is recognised by lead providers who are commissioning services from other healthcare bodies.
Operating expenditure
Total operating expenditure increased by 9.1% from £110.9 billion in 2021/22 to £121.0 billion in 2022/23; a real terms increase of 2.3% when adjusted for inflation.
79% (£8.0 billion) of the increase in operating expenditure related to employee costs, which is largely driven by the pay awards for 2022/23. A focus on reducing waiting lists and the impact of industrial action has required increased use of temporary staff further driving up employee costs. Tackling backlogs has also increased supplies, services and drugs costs. This includes higher spend on cancer drugs alongside higher treatment volumes with significant reductions in the number of patients waiting more than 62 days for cancer diagnosis or treatment.
Other premises costs in the chart above have previously included expenditure on operating leases. The implementation of IFRS 16 Leases in 2022/23 brought the majority of lease arrangements on balance sheet with a reduction in lease payments charged to operating expenditure and an increase in depreciation recognised.
The roll-out of provider led collaboratives for the secondary commissioning of certain specialist mental health and learning disability services as well as initiatives for the reduction of elective waiting lists have led to an increase in healthcare services purchased by NHS providers from non-NHS bodies which forms part of the other movements in operating expenditure.
Impact of impairments
Impairments to the carrying value of assets are charged to operating surplus except where previous revaluation surpluses remain: in such cases a reduction is first recognised in the revaluation reserve to the extent of the remaining surplus for that asset. Where the impairments are the result of a permanent loss, such as fire damage, they are always charged to expenditure. In 2022/23 net impairments charged to income and expenditure were £1,054 million (2021/22: £700 million). A further £518 million of net impairments was charged to reserves (2021/22: £140 million), reducing previously recognised revaluation surpluses. Providers also recognised revaluation surpluses directly in reserves totalling £2,431 million (2021/22: £1,534 million). This results in a net upwards valuation movement on non-current assets of £859 million compared to only £694 million in 2021/22.
There were 135 NHS providers recording a net impairment within surplus/deficit in 2022/23 (2021/22: 133) while 64 providers recorded net reversals of impairments (2021/22: 63). This increase in net impairments includes £192 million of impairments to right of use assets newly recognised on balance sheet following the implementation of IFRS 16 Leases.
Of the £1,054 million of net impairments charged to income and expenditure, 91% arose from changes in market price, compared to 84% in 2021/22. These impairments reflect market conditions at the time of valuation and not a deterioration in the service potential of the asset. Further details of impairments are provided in note 9 to the accounts.
Net finance costs
Net finance costs in 2022/23 showed a net decrease of £43 million to £1,757 million. The significant increase in the Bank of England base rate during 2022/23 enabled providers to generate interest income on cash balances which outweighed the increase in contingent rent on private finance initiative and similar schemes as well as interest charges arising on lease liabilities recognised following the implementation of IFRS 16 Leases.
Working capital and borrowings
At 31 March 2023, NHS providers held cash and cash equivalents of £12.8 billion; equivalent to 6.1 weeks’ operating costs in a sector with annual revenue of £110.5 billion (31 March 2022: 7.8 weeks). This revenue figure excludes the 6.3% NHS pension contribution made by NHS England and the 2022/23 non-consolidated pay award.
The number of receivables days is broadly stable between year ends at 13.3 days in 2022/23 (2021/22: 13.0 days). Payable days decreased to 40.6 days in 2022/23 from
42.5 days in 2021/22. Providers are monitored on their reported timeliness in paying suppliers. Both calculations exclude the impact of the 2022/23 non-consolidated pay award accrued at the year end.
Total long-term and working capital borrowing at 31 March 2023 was £16.1 billion (31 March 2022: £11.3 billion). This increase in borrowings is mainly a result of implementing IFRS 16 Leases. As at 31 March 2023 the provider sector recognised
lease liabilities of £5,760 million (31 March 2022: £351 million). More information is provided about lease liabilities recognised upon implementation of the new standard on 1 April 2022 in note 14.6 to the financial statements.
Capital expenditure
Providers’ ability to invest in capital schemes is limited by constraints in DHSC’s capital expenditure limit. This capital expenditure limit was increased to reflect the implementation of IFRS 16 Leases, where new leases commencing in 2022/23 are capitalised rather than recognised in expenditure. In 2022/23 the provider sector incurred an additional £619 million of gross capital expenditure (after the elimination of inter-provider leases) as a consequence of applying the new standard.
Integrated care systems are allocated capital budgets termed capital envelopes to cover day-to-day operational capital investment which allows for local prioritisation of available resources within the system. These allocations are supplemented with centrally allocated funds to cover nationally strategic projects such as new hospitals and hospital upgrades. Further resource was also available in 2022/23 to cover national programmes such as elective recovery, diagnostics and the programme to eradicate dormitories from mental health facilities.
Total purchases and new or modified leases of property, plant and equipment and intangible assets were £7.8 billion (2) (2021/22: £6.9 billion). More than half (63%) of capital spend was on land and buildings, with a further 19% on plant, equipment and transport, 11% on information technology, and 7% on other capital (Figure 3).
Figure 3: proportion of capital spend by type, 2022/23
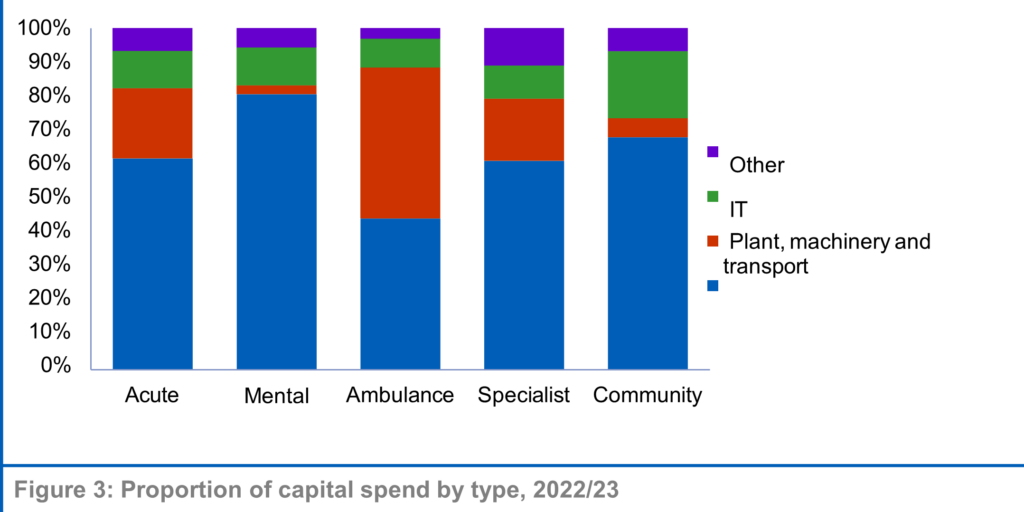
(2) This figure includes new leases and lease remeasurements excluding peppercorn leases. It excludes the reinstatement of assets at the end of a lease and capitalised dilapidation provisions.
The NHS is committed to investing in the redevelopment of estates to support the delivery of high-quality healthcare and maintain patient safety. As examples of the breadth of schemes that have been developed: in March 2023, Derbyshire Healthcare NHS Foundation Trust broke ground on the development of two new mental health in- patient units being built at the Kingsway Hospital and Chesterfield Royal Hospital sites. The 54 en-suite single rooms in each facility will replace the existing dormitory accommodation. University Hospitals Plymouth NHS Trust opened a new 40 bed, two ward discharge unit at Mount Gould Hospital in March 2023. The unit will enable the trust to discharge medically fit patients to support their recovery and return home and release beds for patients waiting for elective and urgent care. Further information on capital developments in each provider can be found in their annual reports and accounts.
Since 2019 the NHS in England has been undertaking a programme to identify cases of reinforced aerated autoclaved concrete (RAAC) in the NHS estate, a type of building material with an intrinsic risk of failure. Where RAAC is identified, appropriate mitigations are put in place and plans developed for eradication. Earlier phases of the programme focused on sites with the greatest impact, including planning for replacement in the most affected cases under the ‘New Hospitals Programme’. As the programme of work expands, further examples of RAAC have been identified since the 31 March 2023 year end. In all cases where RAAC has been found mitigations have been put in place to manage the impact on service provision. The impact on the valuation of assets at 31 March 2023 cannot be quantified precisely without commissioning new professional valuations.
However using estimation techniques such as assessing the floor area of spaces affected by RAAC in relation to the total floor area of the hospital asset, we are satisfied that the impact on the 31 March 2023 balance sheet is not material to the accounts.
Events after the reporting period
As at 31 March 2023 there were 212 NHS providers. Since this date two NHS providers have been dissolved and their services transferred to existing providers. More details can be found in note 34 to the financial statements. As at the date of authorisation of these accounts, there are 210 NHS providers.
Wider context
More information on the performance of the NHS in 2022/23 and priorities going forward can be found in NHS England’s annual report and accounts.
Amanda Pritchard Chief Executive Officer, 21 January 2024.
Statement of accounting officer’s responsibilities and accountability framework
I am designated as the Accounting Officer for NHS England. In this capacity I am responsible for ensuring that NHS England prepares consolidated NHS provider accounts to send to the Secretary of State and the Comptroller and Auditor General. I am not the accountable/accounting officer for each individual NHS trust/NHS foundation trust; this is the role of each local chief executive. An NHS trust’s chief executive is designated as the accountable officer when their appointment is confirmed by NHS England. NHS foundation trust chief executives are designated as the accounting officer by the NHS Act 2006.
Professor Stephen Powis was the accounting officer for NHS Improvement (being the Monitor and NHS Trust Development Authority legal entities) for the 2021/22 financial year and the first part of the 2022/23 financial year up to 30 June 2022. On 1 July 2022 Monitor and the NHS Trust Development Authority were abolished and their functions transferred to NHS England. I, as Chief Executive of NHS England, received assurances from Professor Stephen Powis at this date.
NHS trusts
The Secretary of State is responsible for determining, with HM Treasury’s approval, the form of accounts each NHS trust must adopt. This is described in the Department of Health and Social Care’s Group Accounting Manual (GAM), which is based on HM Treasury’s Financial Reporting Manual (FReM). NHS England has set out the responsibilities of each NHS trust accountable officer to ensure:
- there are effective management systems in place to safeguard public funds and assets
- the trust achieves value for money from the resources available to it
- the trust’s expenditure and income have been applied to the purposes intended by Parliament and conform to the authorities which govern them
- effective and sound financial management systems are in place
- the Trust’s annual accounts give a true and fair
NHS England has set out the responsibilities of NHS trust directors to:
- apply suitable accounting policies consistently
- make reasonable judgements and estimates
- make a statement within the accounts on whether applicable accounting standards have been followed, and to disclose and explain any material departures and
- prepare the financial statements on a going concern basis and disclose any material uncertainties over going concern.
NHS foundation trusts
NHS England is responsible for determining, with the Secretary of State’s approval, the form of accounts each NHS foundation trust must adopt. The NHS foundation trust annual reporting manual (FT ARM), which is based on the FReM, sets out the responsibilities of each NHS foundation trust accounting officer to:
- apply suitable accounting policies consistently
- make reasonable judgements and estimates
- make a statement within the accounts on whether applicable accounting standards have been followed, and to disclose and explain any material departures
- ensure the use of public funds complies with the relevant legislation, delegated authorities and guidance
- confirm that the annual report and accounts, taken as a whole, is fair, balanced and understandable and provides the information necessary for patients,
regulators and stakeholders to assess the NHS foundation trust’s performance, business model and strategy and
- prepare the financial statements on a going concern basis and disclose any material uncertainties over going concern.
Consolidated NHS provider accounts
In discharging its responsibilities in accordance with the directions to NHS England issued by the Secretary of State, NHS England has prepared consolidated NHS provider accounts on a basis consistent with the individual NHS providers’ accounts and consolidated in accordance with International Financial Reporting Standards (IFRS), as amended for NHS providers by the FReM, the FT ARM and the GAM.
The Secretary of State’s directions require NHS England to prepare these consolidated NHS provider accounts to:
- give a true and fair view of the state of affairs of NHS trusts and foundation trusts collectively as at the end of the financial year and the comprehensive income and expenditure, changes in taxpayers’ equity and cash flows for the financial year then ended
- disclose any material expenditure or income that has not been applied for the purposes intended by Parliament or material transactions that have not conformed to the authorities that govern them.
As far as I am aware, there is no relevant audit information of which the auditors of the consolidated NHS provider accounts are unaware. As Accounting Officer I have taken all the steps I ought to have taken to make myself aware of any relevant audit information and to establish that the auditors are aware of this information.
Amanda Pritchard Chief Executive, 21 January 2024.
Annual governance statement
This annual governance statement (AGS) for the NHS provider sector has been prepared in the context of the accountability framework set out above. It has been prepared as a consolidation of the sector position based on reference to:
- the segmentation of providers under the NHS Oversight Framework
- disclosures in local annual governance statements and
- the audit reports issued by local external
Scope of responsibility
NHS England’s Board is not responsible for the internal control and systems of NHS providers; this is the responsibility of each NHS provider’s board.
NHS trusts
As accountable officer, each NHS trust’s chief executive is accountable to NHS England and is responsible for maintaining a sound system of internal control that supports the achievement of the trust’s policies, aims and objectives. In addition, the chief executive, as accountable officer, has responsibility for safeguarding public funds and the organisation’s assets as set out in the NHS trust accountable officer memorandum.
NHS foundation trusts
As accounting officer, each NHS foundation trust’s chief executive has responsibility to Parliament for maintaining a sound system of internal control that supports the achievement of the trust’s policies, aims and objectives. In addition, the chief executive, as accounting officer, has responsibility for safeguarding public funds and the organisation’s assets as set out in the NHS foundation trust accounting officer memorandum.
Purpose of the system of internal control
NHS England’s system of internal control is designed to support the achievement of its policies, aims and objectives and ensure compliance with legal and other obligations on NHS England and NHS trusts and foundation trusts. As part of this system, NHS England has the following processes to ensure these accounts provide a ‘true and fair’ view of the affairs of NHS providers:
- contributing to the development of guidance to NHS trusts and NHS foundation trusts through the Department of Health and Social Care’s (DHSC’s) Group Accounting Manual (GAM); this has been approved by HM Treasury
- providing guidance to foundation trusts through the NHS foundation trust annual reporting manual (FT ARM); this has been approved by the Secretary of State
- relying on the external auditors appointed by each NHS trust/NHS foundation trust’s council of governors to ensure the truth and fairness of each set of accounts consolidated into these accounts; these auditors have each undertaken an audit in accordance with the Code of audit practice (audit code), issued by the Comptroller and Auditor General, supported by the National Audit Office (NAO)
- appointing the Quality Assurance Directorate of the Institute of Chartered Accountants in England and Wales and Audit Quality Review department of the Financial Reporting Council to review the quality of the work of NHS foundation trust auditors and consider their The audits of NHS trusts are reviewed under similar arrangements by Statute, not overseen by NHS England
- attending the NAO’s Local Auditors’ Advisory Group and associated technical networks, to which senior representatives from each of the audit suppliers appointed as auditors of NHS providers are invited; the forum members discuss technical audit and accounting issues in the public sector, including those concerning NHS bodies and
- consideration by NHS England’s management and by its Audit and Risk Assurance Committee of the consolidated accounts and the processes established to derive them.
Each NHS provider’s annual report and accounts includes an AGS for the year ended 31 March 2023. Each individual AGS explains how the accountable/accounting officer has reviewed the effectiveness of internal control during the period and highlights any significant control issues where the risk cannot be effectively controlled.
Timeliness of local accounts
In preparing the consolidated provider accounts based on consolidation schedules from NHS providers, we are reliant on each provider submitting an audited annual report and accounts to us. We and the Department of Health and Social Care issue directions to NHS providers on the timing by which these should be submitted.
The vast majority of NHS providers and their auditors continued to meet the deadline set for submission of audited accounts in 2022/23 and we recognise the significant efforts by providers and audit firms made to achieve this. The compliance rate was broadly similar to 2021/22, but 2021/22 was a year which showed significant deterioration compared to historic norms. In 2022/23 a small number of provider audited accounts were significantly late; this has delayed the preparation of these consolidated accounts.
There are many reasons why a set of audited accounts may go beyond the deadline: for example this may reflect illness in the preparer finance team or audit team, or a significant issue may be encountered that takes time to resolve, which may reflect weaknesses in a Trust’s preparation of its accounts. It is important that auditors can complete their work independently of outside influence and take the necessary time to ensure their audit opinion is the right one and supported by appropriate audit evidence. However standing back from the level of individual engagements, it is clear that success in enabling providers to achieve the audited accounts deadline, to which all firms sign up collaboratively, varies significantly between audit firms. For example of the five NHS providers audited by one audit firm, only one had submitted audited accounts by 31 August, two months after the deadline.
NHS England continues to work to improve timeliness in financial reporting including:
- encouraging auditors to give clear reporting to audit committees where the preparer’s quality of draft accounts or working papers needs to improve
- working closely with providers to ensure they appoint external auditors in good time, which helps increase the likelihood of deadlines being achieved
- regular engagement with partners including the Department of Levelling Up, Housing and Communities and the Financial Reporting Council on policy matters affecting the broader local audit system: we believe strongly that firms having sufficient capacity across their wider portfolio of work to enable effective interim audits at NHS bodies is important for success
- working with providers where financial reporting issues arise to ensure they are able to address findings effectively
- regular engagement with the audit firms and responding to their feedback to continue to strengthen the NHS financial reporting landscape, and working with partners to make sure training and guidance is available for preparers
- liaising with broader stakeholders on wider matters that can cause delays in NHS accounts, for example sign offs of local government pension scheme audits, which directly affects a handful of NHS providers with a corresponding impact on these consolidated accounts.
We acknowledge that 2022/23 was a complex year for financial reporting and audit in the NHS, in particular the implementation of IFRS 16, the mid-year transition from CCGs to ICBs meaning there was an increased number of bodies in 2022/23 requiring audit, and the growing backlog of audits in local government putting pressure on audit teams. We will continue to take the steps including those outlined above to improve overall timeliness in NHS financial reporting. The Department of Health and Social Care has an ambition to return to laying the main national consolidated accounts (being the DHSC group, NHS England group and consolidated provider accounts) before Parliament in advance of the summer Parliamentary recess in July. Significant improvements in overall timeliness of NHS financial reporting and audit would be required if this is to be achievable in the years ahead.
Overview of internal control systems at NHS trusts and NHS foundation trusts
NHS Oversight Framework
The NHS Oversight Framework for 2022/23 provides the framework for overseeing the delivery of high quality, sustainable care with a focus at both local system and organisational level and identifying potential support needs.
The Framework describes a process to identify where NHS organisations may benefit from or require support to meet the standards required of them in a sustainable way and deliver the overall objectives for the sector in line with the priorities set out in the 2022/23 Operational Planning Guidance, the NHS Long Term Plan and the NHS People Plan.
To provide an overview of the level and nature of support required across systems, inform oversight arrangements and target support capacity as effectively as possible, NHS England regional teams allocate NHS organisations to one of four ‘segments’.
A segmentation decision indicates the scale and general nature of support needs, from no specific support needs (segment 1) to a requirement for mandated intensive support (segment 4). A segment does not determine specific support requirements. By default, all NHS organisations are allocated to segment 2 unless the criteria for moving into another segment are met. These criteria have two components:
a. objective and measurable eligibility criteria based on performance against the six oversight themes using the relevant oversight metrics (the themes are: (i) quality of care, access and outcomes; (ii) people; (iii) preventing ill-health and reducing inequalities; (iv) leadership and capability; (v) finance and use of resources; (vi) local strategic priorities)
b. additional considerations focused on the assessment of system leadership and behaviours, and improvement capability and capacity.
An NHS trust or foundation trust will be placed in segment three or four where it has been found to have significant support needs that may require formal intervention and mandated support. They will be subject to enhanced direct oversight by NHS England (in partnership with their ICB) and, depending on the nature of the problem(s) identified, additional reporting requirements and financial controls.
While NHS trusts were exempt from the requirement to apply for and hold a licence in 2021/22 and 2022/23, NHS England ensured that NHS trusts were treated via equivalent methods to those applied to NHS foundation trusts. This included giving directions where necessary to ensure compliance. NHS trusts were issued licences on 1 April 2023 and from 2023/24 will be subject to the same licence conditions as NHS foundation trusts.
Segmentation of NHS providers is updated regularly. The table below summarises NHS providers’ segmentation as at 31 March 2023. A prior year comparative is not provided as this table provides a snapshot at that point in time and the design and application of the Oversight Framework may evolve over time.
|
Segmentation at 31 March 2023 | ||||
| Number of NHS trusts | Number of NHS FTs | Total number of providers | % of sector | |
|
1 |
10 |
23 |
33 |
16% |
|
2 |
27 |
65 |
92 |
43% |
|
3 |
25 |
44 |
69 |
33% |
|
4 |
6 |
12 |
18 |
8% |
|
Total |
68 |
144 |
212 |
|
NHS providers in segment 3 or 4
Where an NHS provider is triggering a specific concern, NHS England will work with the ICB to understand why this concern has arisen and if a support need exists. Based on this assessment, NHS England will agree the subsequent level of support that is required. Where there is a need for mandated support by NHS England the provider will be placed into segment 3 or 4, depending on the complexity of the support need.
A segment 3 decision will result in a bespoke support offer led by the NHS England regional team drawing on system and national expertise as required.
Segment 4 decisions are reserved for those trusts experiencing long standing complex issues or serious failures in areas such as quality, safety, leadership, governance or financial plans. A segment 4 decision will always trigger a referral to NHS England’s national Recovery Support Programme (RSP). Decisions on referrals into this programme are made by an executive committee of NHS England based on recommendations from Regional Directors or the Care Quality Commission. Where a referral into the RSP for a trust is agreed a dedicated Improvement Director will be appointed to work alongside the Trust leadership as well as the ICB and regional team to oversee the development and delivery of an improvement plan. A diagnostic review will be undertaken to identify underlying drivers that need to be addressed and embed improvement upstream to prevent further deterioration and enable stabilisation.
Enforcement action
Where an NHS provider is in breach of its licence conditions (or where NHS England has reasonable grounds for suspecting a breach), NHS England may also consider the use of its enforcement powers. These powers include, among others, agreeing enforcement undertakings or issuing directions to the provider to secure compliance and ensure the breach does not recur. Details of any enforcement action is publicly available via the Provider Directory on our website.
In exceptional circumstances an NHS trust or NHS foundation trusts may be placed in trust special administration. Administration is a regime for ensuring the continuity of essential services in the event of provider financial distress. No trusts or foundation trusts were subject to trust special administration in 2021/22 or 2022/23.
NHS trusts’ and NHS foundation trusts’ significant internal control weaknesses
Sources of information
In the information that follows, NHS England has collated a number of sources of information to disclose the position for NHS providers.
NHS Oversight Framework segment 3 or 4
Where an NHS provider is in Oversight Framework segment 3 or 4 and is receiving mandated support, the support offered to the provider will be defined in terms of the Oversight Framework themes.
NHS England placing an NHS provider into segment 3 or 4 and mandating support would normally indicate the existence of control weaknesses or failings in the trust’s control environment.
Other significant control issues
NHS providers may also declare other matters as significant control issues. NHS England’s FT ARM for NHS foundation trusts and AGS guidance for NHS trusts gives guidance on how to determine whether an internal control matter is ‘significant’ but does not prescribe an approach; this is a matter for each trust’s board. The table that follows includes all cases where trusts have disclosed one or more significant control weaknesses in their annual governance statement.
External auditor’s conclusion on use of resources
In addition to the ‘true and fair’ audit opinion on the accounts, external auditors of NHS trusts and NHS foundation trusts are required to conclude whether the trust has made proper arrangements for securing economy, efficiency and effectiveness in its use of resources. Where the auditor identifies significant issues, the auditor reports that they are unable to satisfy themselves that the trust has made these proper arrangements.
Such reporting does not imply that the ‘true and fair’ audit opinion on the provider’s accounts is qualified. These conclusions are listed in the table that follows. In each case we summarise if this modification relates to the same matters as the reason for Oversight Framework segmentation as 3 or 4 by NHS England
Defining a significant internal control issue for this document
Our starting point for this consolidated annual governance statement is where a trust has locally assessed and disclosed a significant internal control issue in its own annual governance statement.
In addition, regardless of whether these have been reported locally, we also deem the following to be evidence of significant internal control weaknesses:
- NHS Oversight Framework segmentation of 3 or 4 by NHS England during the year
- the external auditor modifying their use of resources
In the table that follows we also disclose notes on other non-standard forms of the auditor’s reporting. We do not consider that entries here necessarily represent a significant internal control weakness.
Summary of results
The table below provides a summary of the detail that follows:
|
2022/23 |
2021/22 | |
|
Number of providers receiving mandated support from NHS England during the year |
94 |
89 |
|
Total number of modified conclusions relating to arrangements for securing economy, efficiency and effectiveness in the provider’s use of resources |
63 |
41* |
|
Number of providers where ‘true and fair’ audit opinion has been modified (qualified) in respect of inventory counts and associated impact |
1 |
19 |
|
Number of providers where ‘true and fair’ audit opinion has been modified (qualified) for another reason |
1 |
1 |
|
Providers consolidated without an audit report |
2 |
Was 3, now 0 |
* There were 40 providers with modified conclusions relating to arrangements for securing economy, efficiency and effectiveness in the provider’s use of resources at the time of finalising the consolidated provider accounts for 2021/22. The audit report for University Hospitals of Leicester NHS Trust was issued in May 2023 and includes a modification to the use of resources conclusion making this final total 41.
Providers consolidated without an audit report
The consolidated provider accounts for 2021/22 describes how that document was finalised with 3 providers not having received their audit report. These have now been subsequently received: Wirral Community Health and Care NHS Foundation Trust in February 2023, Surrey and Sussex Healthcare NHS Trust in March 2023 and University Hospitals of Leicester NHS Trust in May 2023. More information on University Hospitals of Leicester NHS Trust is provided below.
The consolidated provider accounts in 2022/23 have been prepared using unaudited information for two providers as the audit reports remained outstanding at the time of finalising these disclosures on 15 January 2024. These providers are:
- Buckinghamshire Healthcare NHS Trust
- East Suffolk and North Essex NHS Foundation Trust
Individually, the financial statements of the trusts are not material to the consolidated provider accounts and the delay does not reflect any financial reporting or governance matters at the trusts to our knowledge. Some elements of the financial statements are material in aggregate to the consolidated provider accounts. More information is provided in note 31 to the consolidated financial statements.
Modifications of ‘true and fair’ audit opinion: inventory
In 2021/22, 19 providers received audit opinions qualified for a limitation of scope in respect of inventories where sufficient assurance could not be obtained over material inventory balances at a previous year end with impacts on inventory movements in the current or comparative year. Where inventory is material to a provider, international standards on auditing prescribe that the auditor must attend one or more inventory counts. These qualified opinions arose because restrictions on movement in response to the COVID-19 pandemic prevented some providers from performing year-end inventory counts and/or auditors from attending such counts in previous years. For the affected prior year ends, NHS providers were able to employ a variety of procedures to assure themselves of the material accuracy of inventory balances at the year end.
In 2022/23, one provider continued to receive a qualified audit opinion for a limitation of scope for this matter. This arose where the absence of an audited inventory count at 31 March 2021 meant there was uncertainty over the comparative 2021/22 operating expenditure.
The inventory balances at these trusts and associated movements are not material to these consolidated provider accounts. Given the effect of the pandemic, we do not consider a true and fair audit qualification arising from a lack of audit evidence on inventory at the statement of financial position date to constitute a significant internal control issue for the trust.
Modifications of ‘true and fair’ audit opinion: University Hospitals of Leicester NHS Trust
In the consolidated provider accounts for 2021/22 we described the recent history of financial reporting for University Hospitals of Leicester NHS Trust. The Trust’s 2021/22 accounts were subsequently finalised on 15 May 2023 with a qualified audit opinion in two respects: evidence for plant and equipment asset existence, and comparative figures covered by the 2020/21 audit adverse opinion and the impact on the statement of comprehensive income in 2021/22.
The Trust’s 2022/23 accounts were finalised with an audit opinion on 31 August 2023, meeting the target for timing for financial reporting for the Trust set by NHS England and meaning the Trust’s audited accounts have been included in these consolidated accounts. The audit opinion is qualified in two respects: evidence for plant and equipment asset existence, and the impact of additional qualifications in previous years’ financial statements affecting comparative figures for 2021/22. In its auditors’ annual report covering the 2021/22 and 2022/23 financial years, the Trust auditor notes that “progress has been made in responding to the issues with governance and internal control during these two years” but that “as the Trust recognises, there is still a significant way to go to fully address the challenges that the Trust faces”.
The timeliness of the Trust’s financial reporting has notably improved and the scale of qualifications reported by the Trust’s auditors has reduced. However it continues to be the case that local qualified accounts are highly anomalous within the context of NHS bodies. The Trust intends to complete its 2023/24 accounts in line with the national timetable and has a programme of work to achieving the lifting of the qualifications affecting the accounts.
List of providers with matters to report
The tables below list the NHS trusts and NHS foundation trusts for which there are matters to report in the relevant columns. It therefore does not list all NHS providers. Column (3) lists significant internal control issues disclosed in local annual governance statements, excluding matters relating to the same issues as covered by NHS England’s mandated support or individual mentions of the impact of the COVID-19 pandemic. Therefore, the absence of a tick in this column does not necessarily mean the provider disclosed no significant internal control issues in its local AGS.
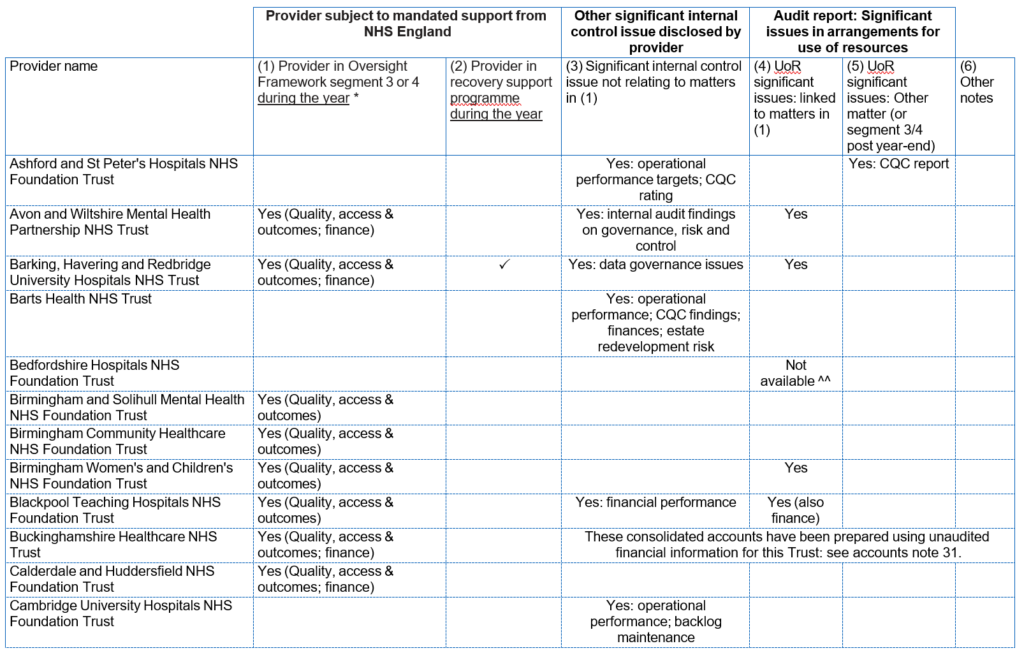
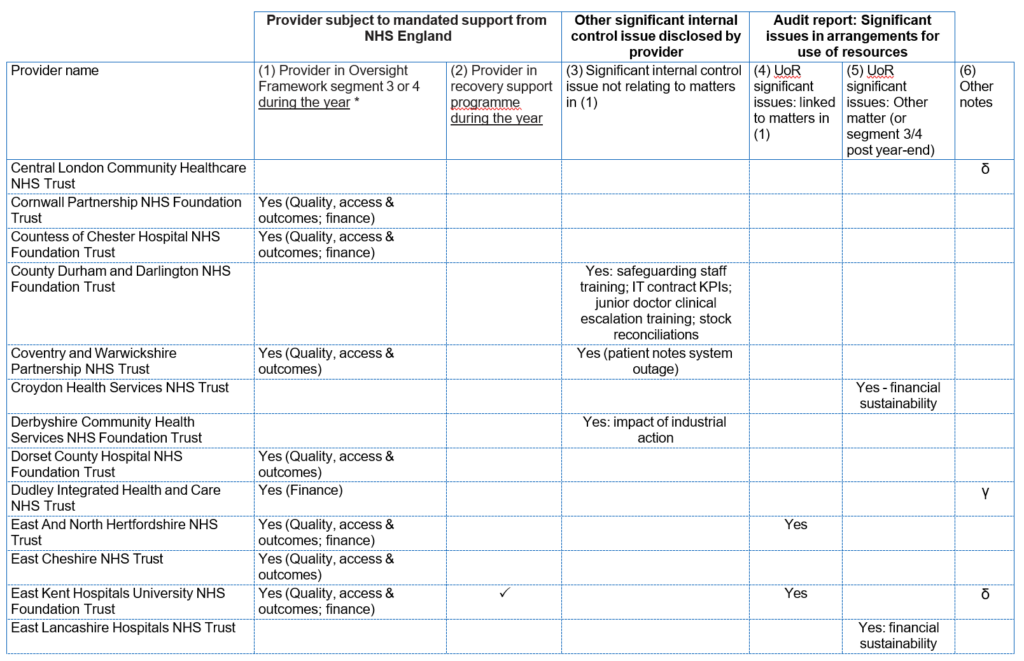
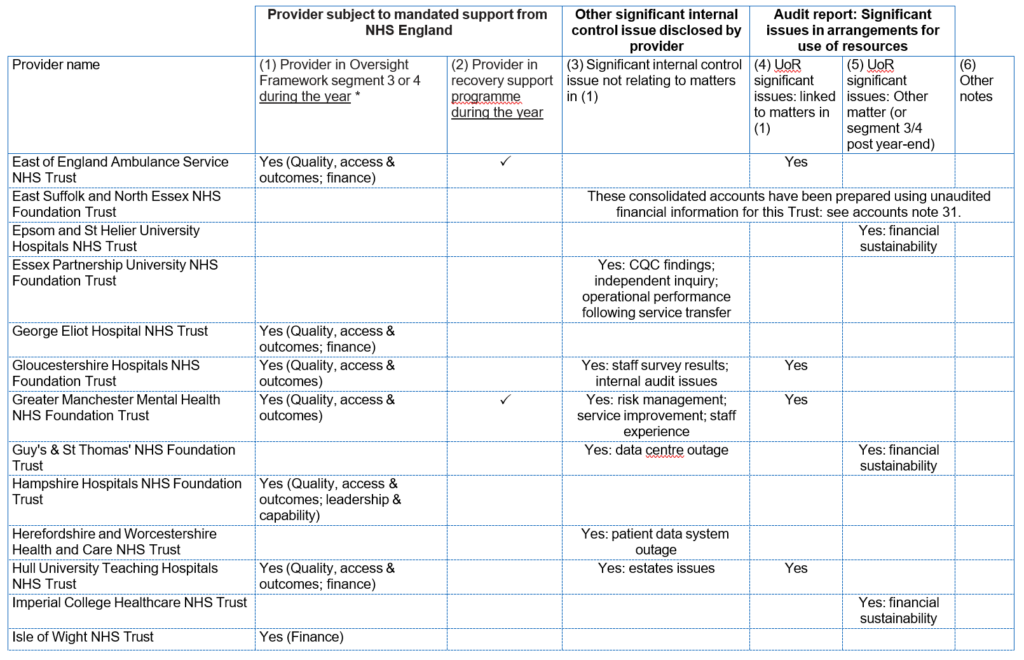
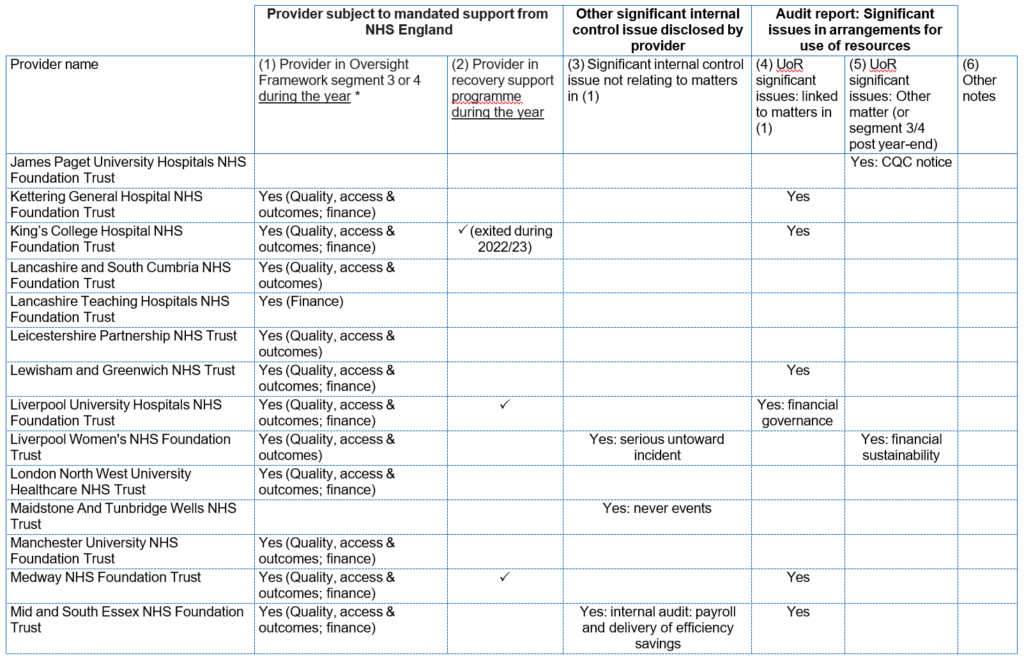
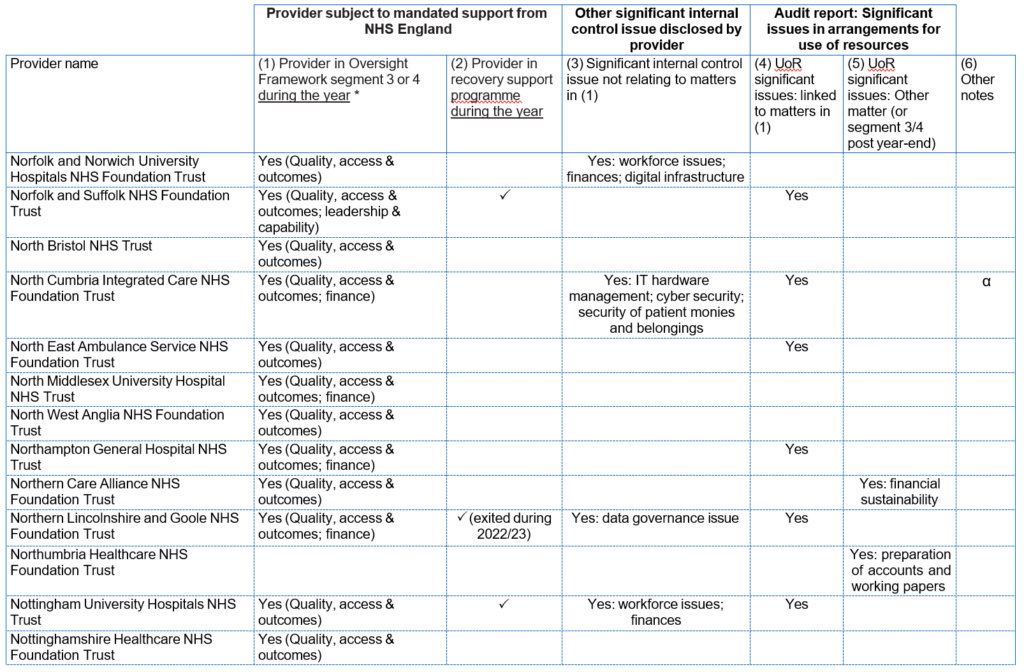
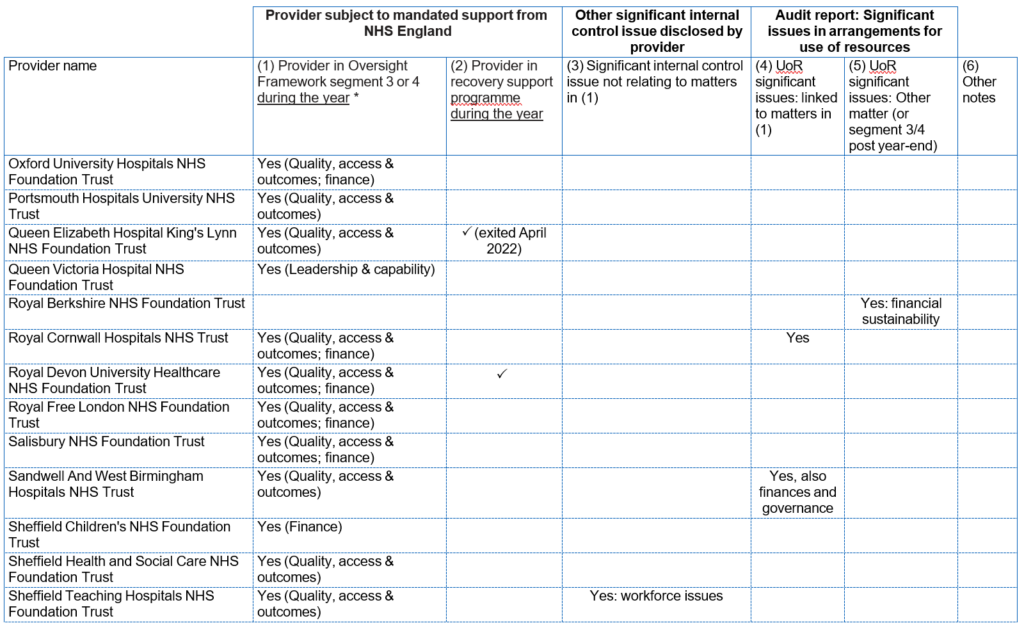
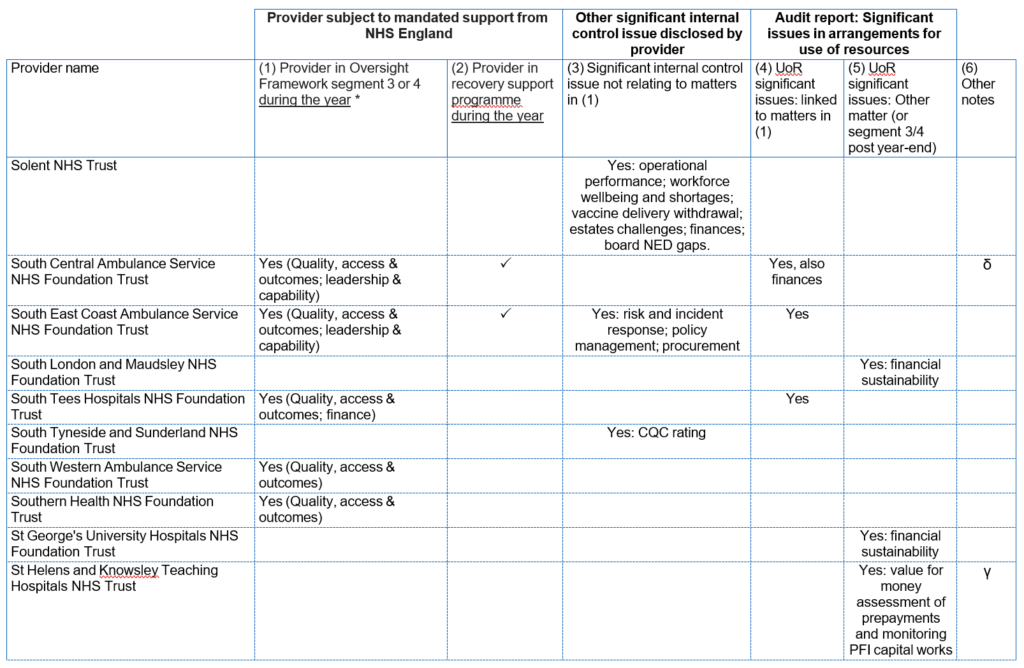
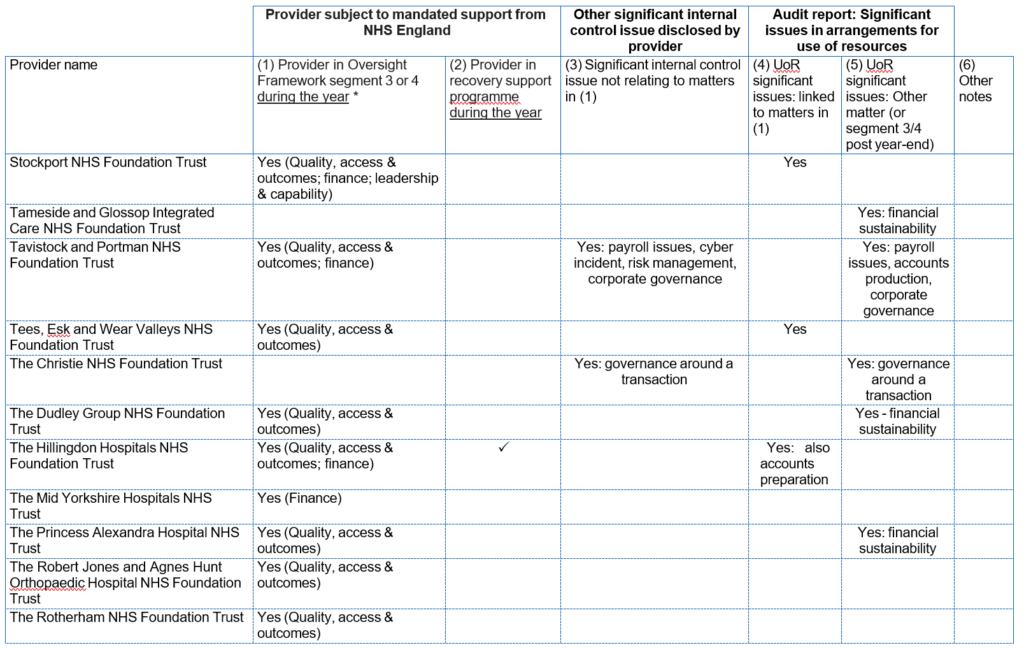
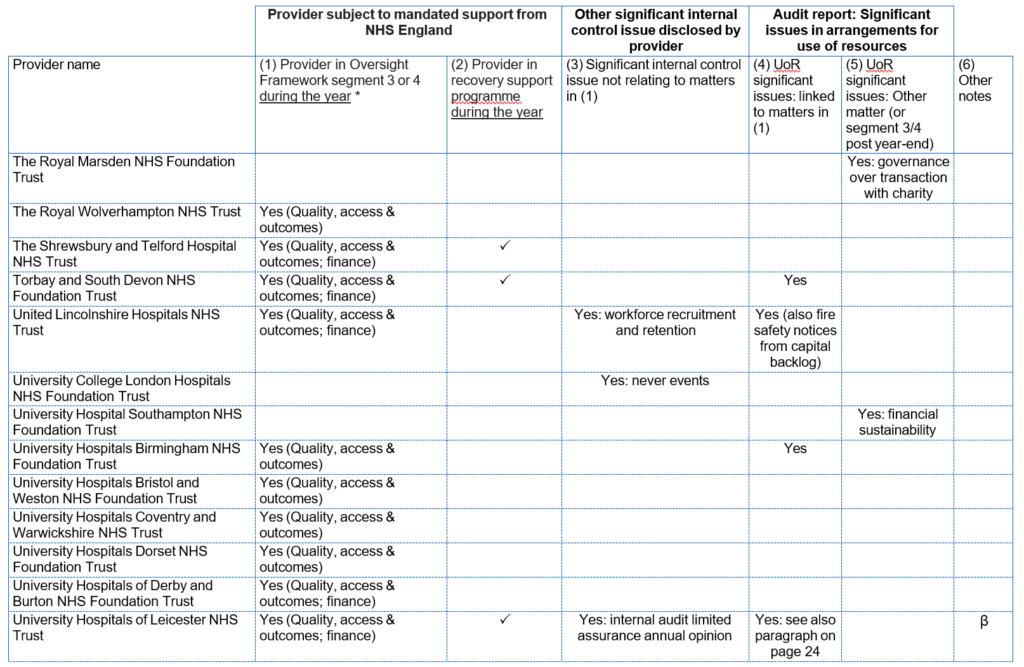
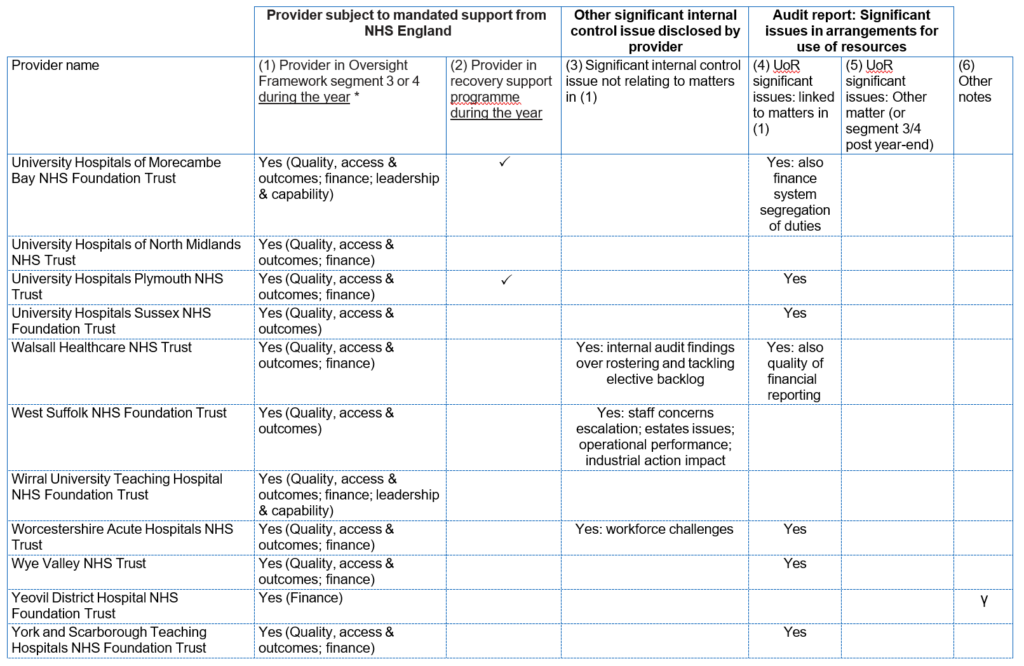
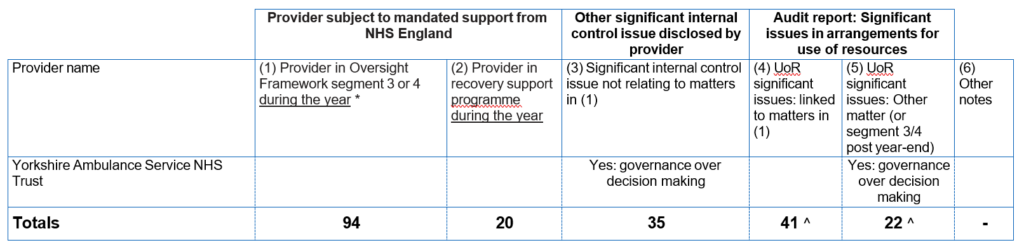
Notes for column (6) – note we do not consider these items as significant internal control issues:
α 1 provider: modified audit opinion due to inventory counts
β 1 provider: modified audit opinion at University Hospitals of Leicester NHS Trust
γ 3 providers are denoted with this symbol in the table to indicate that the auditor included an ‘emphasis of matter’ relating to the organisation demising or significantly changing its organisational form with services transferring to or from other trusts, either during the reporting year or anticipated in the future
δ 3 providers with modification to audit report relating to remuneration report. Further information is available in the individual trust accounts.
Other notes:
^ No audit report has been issued for Buckinghamshire Healthcare NHS Trust and East Suffolk and North Essex NHS Foundation Trust at the time of finalising the disclosures in these consolidated accounts on 15 January 2024: see above and note 31 to the financial statements.
^^ The auditor’s conclusion on use of resources arrangements had not been issued for Bedfordshire Hospitals NHS Foundation Trust at the time of finalising the disclosures in these consolidated accounts on 15 January 2024.
* Approach for column (1):
- The explanation for each provider shows the support offerings for each provider in segment 3 or 4 at any point during the year. In some cases a trust may receive a combination of mandated and targeted support with all such support needs included here.
- In many cases our support also relates to the leadership and capability theme in the Oversight Where this is the case the underlying issues will usually relate to other themes so this is not always additionally listed here, unless it is a primary matter.
Auditor referrals of matters arising
Under Section 30 of the Local Audit and Accountability Act 2014 for NHS trusts, and under Schedule 10 to the NHS Act 2006 for NHS foundation trusts, where an auditor believes that the body or an officer of the body:
- is about to make, or has made, a decision which involves or would involve the incurring of expenditure which is unlawful, or
- is about to take, or has taken, a course of action which, if pursued to its conclusion, would be unlawful and likely to cause a loss or deficiency
The auditor should make a referral to the Secretary of State (for NHS trusts)/NHS England (for NHS foundation trusts).
37 NHS trusts (2021/22: 384*) and no NHS foundation trusts (2021/22: none) were subject to such referrals in 2022/23. These referrals relate to a failure by the trust to meet the statutory breakeven duty target. This requires an NHS trust to achieve a cumulative breakeven over a three or five-year period. The underlying issues in trust finances are disclosed as part of the detail on significant internal control issues presented above. The statutory breakeven duty does not apply to NHS foundation trusts.
* This figure was 36 at the time of finalising the consolidated provider accounts for 2021/22. Auditors submitted subsequent section 30 referrals relating to the NHS trust breakeven duty at University Hospitals of Leicester NHS Trust in January 2023 and Surrey and Sussex Healthcare NHS Trust in March 2023 which are referenced in 2021/22 audit reports, making this total now 38.
Amanda Pritchard Chief Executive, 21 January 2024.
The certificate of the Comptroller and Auditor General to the Houses of Parliament
Opinion on consolidated financial statements
I certify that I have audited the Consolidated NHS Provider Accounts for the year ended 31 March 2023 under the National Health Service Act 2006.
The Consolidated NHS Provider Accounts comprise the:
- Consolidated Statement of Financial Position as at 31 March 2023;
- Consolidated Statement of Comprehensive Income, Consolidated Statement of Cash Flows and Consolidated Statement of Changes in Equity for the year then ended; and
- the related notes including the significant accounting
The financial reporting framework that has been applied in the preparation of the consolidated financial statements is applicable law and UK adopted International Accounting Standards.
In my opinion, the financial statements:
- give a true and fair view of the state of affairs of NHS trusts and NHS foundation trusts, taken collectively, as at 31 March 2023 and of their deficit for the year then ended; and
- have been properly prepared in accordance with the National Health Service Act 2006 and Secretary of State directions issued thereunder.
Opinion on regularity
In my opinion, in all material respects, the income and expenditure recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
Basis for opinions
I conducted my audit in accordance with International Standards on Auditing (UK) (ISAs UK), applicable law and Practice Note 10 Audit of Financial Statements and Regularity of Public Sector Bodies in the United Kingdom (2022). My responsibilities under those standards are further described in the Auditor’s responsibilities for the audit of the financial statements section of my certificate.
Those standards require me and my staff to comply with the Financial Reporting Council’s Revised Ethical Standard 2019. I am independent of NHS England and of NHS trusts and NHS foundation trusts, taken collectively, in accordance with the ethical requirements that are relevant to my audit of the financial statements in the UK. My staff and I have fulfilled our other ethical responsibilities in accordance with these requirements.
I believe that the audit evidence I have obtained is sufficient and appropriate to provide a basis for my opinion.
Conclusions relating to going concern
In auditing the financial statements, I have concluded that NHS England’s use of the going concern basis of accounting in the preparation of the consolidated financial statements is appropriate.
Based on the work I have performed, I have not identified any material uncertainties relating to events or conditions that, individually or collectively, may cast significant doubt on NHS trusts’ and NHS foundation trusts’ collective ability to continue as a going concern for a period of at least twelve months from when the financial statements are authorised for issue.
My responsibilities and the responsibilities of the Accounting Officer with respect to going concern are described in the relevant sections of this certificate.
The going concern basis of accounting for the Consolidated NHS Provider Accounts is adopted in consideration of the requirements set out in HM Treasury’s Government Financial Reporting Manual, which require entities to adopt the going concern basis of accounting in the preparation of the financial statements where it is anticipated that the services which they provide will continue into the future.
Other information
The other information comprises information included in the Consolidated NHS Provider Accounts but does not include the consolidated financial statements nor my auditor’s certificate and report. The Accounting Officer is responsible for the other information.
My opinion on the financial statements does not cover the other information and, except to the extent otherwise explicitly stated in my certificate, I do not express any form of assurance conclusion thereon.
In connection with my audit of the financial statements, my responsibility is to read the other information and, in doing so, consider whether the other information is materially inconsistent with the financial statements, or my knowledge obtained in the audit, or otherwise appears to be materially misstated.
If I identify such material inconsistencies or apparent material misstatements, I am required to determine whether this gives rise to a material misstatement in the financial statements themselves. If, based on the work I have performed, I conclude that there is a material misstatement of this other information, I am required to report that fact.
I have nothing to report in this regard.
Opinion on other matters
In my opinion, based on the work undertaken in the course of the audit, the information given in the review of financial performance of NHS providers, statement of accounting officer’s responsibilities and accountability framework and the annual governance statement for the financial year for which the financial statements are prepared is consistent with the consolidated financial statements and is in accordance with the applicable legal requirements.
Matters on which I report by exception
In the light of the knowledge and understanding of NHS trusts and NHS foundation trust, taken collectively, and their environment obtained in the course of the audit, I have not identified material misstatements in the review of financial performance of NHS providers, statement of accounting officer’s responsibilities and accountability framework and the annual governance statement .
I have nothing to report in respect of the following matters which I report to you if, in my opinion:
- adequate accounting records have not been kept by NHS England or returns adequate for my audit have not been received from branches not visited by my staff; or
- I have not received all of the information and explanations I require for my audit; or
- the annual governance statement does not reflect compliance with HM Treasury’s guidance
Responsibilities of the Accounting Officer for the financial statements
As explained more fully in the statement of accounting officer’s responsibilities and accountability framework, the accounting officer is responsible for:
- maintaining proper accounting records;
- preparing the information which comprises the review of financial performance of NHS providers, statement of accounting officer’s responsibilities and accountability framework and the annual governance statement in accordance with the National Health Service Act 2006, and with the directions made thereunder by the Secretary of State;
- the preparation of the consolidated financial statements in accordance with the applicable financial reporting framework and for being satisfied that they give a true and fair view;
- such internal controls as the accounting officer determines is necessary to enable the preparation of financial statements to be free from material misstatement, whether due to fraud or error; and
- assessing NHS trusts’ and NHS foundation trusts’ collective ability to continue as a going concern, disclosing, as applicable, matters related to going concern and using the going concern basis of accounting unless the accounting officer anticipates that the services provided by NHS trusts and NHS foundation trusts will not continue to be provided in the future.
Auditor’s responsibilities for the audit of the financial statements
My responsibility is to audit, certify and report on the financial statements in accordance with the National Health Service Act 2006.
My objectives are to obtain reasonable assurance about whether the financial statements as a whole are free from material misstatement, whether due to fraud or error, and to issue a certificate that includes my opinion. Reasonable assurance is a high level of assurance but is not a guarantee that an audit conducted in accordance with ISAs (UK) will always detect a material misstatement when it exists. Misstatements can arise from fraud or error and are considered material if, individually or in the aggregate, they could reasonably be expected to influence the economic decisions of users taken on the basis of these financial statements.
Extent to which the audit was considered capable of detecting non-compliance with laws and regulations including fraud
I design procedures in line with my responsibilities, outlined above, to detect material misstatements in respect of non-compliance with laws and regulations, including fraud. The extent to which my procedures are capable of detecting non-compliance with laws and regulations, including fraud is detailed below.
Identifying and assessing potential risks related to non-compliance with laws and regulations, including fraud
In identifying and assessing risks of material misstatement in respect of non-compliance with laws and regulations, including fraud, I considered the following:
- the nature of the sector, control environment and operational performance including the design of NHS trusts’ and NHS foundation trusts’ accounting policies and performance
- inquired of management, NHS England’s head of internal audit and those charged with governance, including obtaining and reviewing supporting documentation relating to NHS England’s policies and procedures on:
- identifying, evaluating and complying with laws and regulations and whether they were aware of any instances of non-compliance;
- detecting and responding to the risks of fraud and whether they had knowledge of any actual, suspected, or alleged fraud; and
- the internal controls established to mitigate risks related to fraud or non-compliance with laws and regulations including NHS England’s controls relating to NHS England’s compliance with the National Health Service Act 2006 and Managing Public Money.
- discussed with the engagement team regarding how and where fraud might occur in the consolidated financial statements and any potential indicators of fraud.
As a result of these procedures, I considered the opportunities and incentives that may exist within NHS trusts and NHS foundation trusts for fraud and identified the greatest potential for fraud in the following areas: revenue recognition, posting of unusual journals, complex transactions, and bias in management estimates. In common with all audits under ISAs (UK), I am also required to perform specific procedures to respond to the risk of management override.
I obtained an understanding of NHS trusts’ and NHS foundation trusts’ framework of authority as well as other legal and regulatory frameworks in which NHS trusts and NHS foundation trusts operate, focusing on those laws and regulations that had a direct effect on material amounts and disclosures in the financial statements or that had a fundamental effect on the operations of NHS trust and NHS foundation trusts. The key laws and regulations I considered in this context included the National Health Service Act 2006, the Health and Social Care Act 2012, the Health and Care Act 2022, Managing Public Money, employment law, and tax legislation.
In addition, I considered regulations and regularity relating to exit packages and, in particular, special severance payments, as I identified the completeness and regularity of special severance payments as a significant risk.
Audit response to identified risk
To respond to the identified risks resulting from the above procedures:
- I reviewed the financial statement disclosures and testing to supporting documentation to assess compliance with provisions of relevant laws and regulations described above as having direct effect on the financial statements;
- I enquired of management and the Audit and Risk Assurance Committee concerning actual and potential litigation and claims;
- I reviewed minutes of meetings of those charged with governance and the board and internal audit reports;
- in addressing the risk of fraud through management override of controls, testing the appropriateness of journal entries and other adjustments; assessing whether the judgements made in making accounting estimates are indicative of a potential bias; and evaluating the business rationale of any significant transactions that are unusual or outside the normal course of business; and enquiring with the auditors of NHS trusts and NHS foundation trusts about the findings of their audits with respect to management override of control; and
- in addressing the risk of fraud in revenue recognition, I notified the auditors of NHS trusts and NHS foundation trusts of the need to consider the presumed risk of fraud in revenue recognition and enquired with them around the findings of their audits with respect to fraud in revenue recognition.
I communicated relevant identified laws and regulations and potential risks of fraud to all engagement team members and remained alert to any indications of fraud or non-compliance with laws and regulations throughout the audit.
A further description of my responsibilities for the audit of the financial statements is located on the Financial Reporting Council’s website at: www.frc.org.uk/auditorsresponsibilities. This description forms part of my certificate.
Other auditor’s responsibilities
I am required to obtain evidence sufficient to give reasonable assurance that the expenditure and income recorded in the financial statements have been applied to the purposes intended by Parliament and the financial transactions recorded in the financial statements conform to the authorities which govern them.
I communicate with those charged with governance regarding, among other matters, the planned scope and timing of the audit and significant audit findings, including any significant deficiencies in internal control I identify during my audit.
Gareth Davies, Comptroller and Auditor General
22 January 2024
National Audit Office
157-197 Buckingham Palace Road Victoria
London SW1W 9SP
Report of the Comptroller and Auditor General to the Houses of Parliament
Introduction
1. The National Health Service Act 2006 requires NHS England to prepare a Consolidated NHS Provider Accounts (“CPA”) for each financial The CPA is a consolidation of the 212 NHS trusts and NHS foundation trusts (“NHS providers”). The CPA is in turn consolidated into the Department of Health and Social Care (DHSC) group accounts. I consider the CPA to be a significant component of DHSC and my audit of the CPA must be complete before I complete my audit of DHSC.
2. I am required to examine, certify, and report on the I provide an opinion on whether the CPA gives a “true and fair” view of the finances of NHS providers, taken collectively. I also provide an opinion on whether the transactions recorded in the CPA have been applied to the purposes intended by Parliament and whether they conform to the authorities which govern them (“regularity”).
3. In this report I set out my observations on the performance of NHS providers in delivering accounts to support the timely production of the CPA.
Audit completion delays of NHS providers
4. NHS providers are audited by a number of different audit firms. NHS providers are free to appoint their external auditors (“local auditors”). Local auditors must comply with the Code of Audit Practice (“the Code”). Under the Local Audit and Accountability Act 2014, I am responsible for the preparation, publication, and maintenance of the Code. The Code sets out what local auditors are required to do to fulfil their statutory responsibilities under the Local Audit and Accountability Act 2014. For 2022-23 the NHS provider audits were undertaken by nine audit firms.
5. The Code stresses the need for local auditors to report on a timely basis. Section 1.19 of the Code requires local auditors to report on a timely basis. Timely reporting includes producing audit reports in time, insofar as the auditor can do so under auditing standards, to allow local bodies to comply with the requirements placed on them to publish their audited financial statements. It also means ensuring that when matters of concern arise during the audit, the auditor raises them promptly with the body and considers whether the matter needs to be brought to public attention at the appropriate time.
6. The timetable set by NHS England and DHSC for the 2022-23 group accounts required local auditors to complete the statutory audits of NHS providers by 30 June 20232. The statutory deadline, under the Government Resources and Accounts Act 2000, requires government departments to lay their annual reports and accounts in Parliament by 31 January, ten months after the financial year end. Although the CPA does not have a statutory deadline for being laid in Parliament, as the CPA is a significant component of the DHSC group, the CPA accounts must be completed to the same timetable as DHSC.
7. DHSC committed to laying their 2022-23 annual report and accounts before the end of 2023. At a Public Accounts Committee hearing on 20 March 2023, regarding the timeliness of the DHSC annual report and accounts 2021-22, DHSC committed to aiming to lay its 2022-23 accounts before the 2023 Parliamentary Christmas recess and then to gradually improve the timeliness in future years. DHSC’s stated aim was to bring forward the laying date by two months each year to eventually enable laying before the Parliamentary summer recess. Before the Covid-19 pandemic, DHSC and NHS England (covering both the NHS England group account and the CPA) routinely laid their annual reports and accounts in Parliament before the Parliamentary summer The last time this happened was for the 2018-19 annual report and accounts. For the 2022-23 accounts, NHS England, DHSC and my staff agreed a target date of 30 November 2023 for audit certification of the CPA, to enable laying before the 2023 Parliamentary Christmas recess.
8. Of the 212 NHS providers, 163 had their 2022-23 annuals report and accounts audited by 30 June 2023. 163 NHS provider audits were completed by 30 June 2023, meaning just over three quarters of NHS providers achieved the target date set by NHS England. By 31 October 2023, 203 (95.8%) NHS provider audits were This was the latest practical date to enable certification of the CPA and DHSC annual report and accounts by 30 November 2023.
9. At the point NHS England finalised the CPA, two NHS provider audits remained outstanding, and these entities account for material transactions and balances in the CPA. By Christmas 2023, 210 NHS provider audits were completed, with the remaining two audits outstanding as the CPA was finalised. NHS England has had to perform alternative procedures to obtain sufficient assurance that the material transaction streams in the outstanding NHS providers are not materially misstated, in the context of the CPA. My staff have reviewed the procedures performed by NHS England and are content that in the context of the CPA, the results are sufficient and appropriate. I have therefore issued a clean “true and fair” audit opinion in respect of the CPA 2022-23. Note 31 to the accounts provides details of the transactions and balances relating to these two NHS providers.
10. NHS England clearly recognises the risks that late auditor reporting can represent and has been proactive in using its influence to support NHS providers and local auditors with timely delivery. As set out in the annual governance statement, NHS England demonstrates a clear understanding of the risks around late auditor reporting, including the delays this has caused to the laying of its own annual report and accounts. NHS England has set out the range of interventions they have used to support NHS providers and local auditors to try and accelerate the audit of NHS provider accounts and it is critical this work continues for 2023-24.
11. In 2023-24 NHS England should continue its role in proactively monitoring audit progress of NHS provider accounts. NHS England has been proactive in 2022-23 in monitoring the progress of late NHS provider accounts, including engaging with the local auditors, my staff, HM Treasury and the Financial Reporting Council (which regulates local audit firms). NHS England remain concerned about the capacity of local auditors to bring forward certification to enable the CPA, and hence DHSC, to lay their annual reports and accounts in Parliament significantly earlier than has happened over the last four financial years.
12. I also have concerns given the wider local audit challenges set out in my report, Timeliness of local auditor reporting on local government in England4. There could still be some risk in the delivery of NHS local audits due to the wider local audit system issues and significant delays in local government audits as the auditors work to clear this blacklog.
Gareth Davies, Comptroller and Auditor General
22 January 2024
National Audit Office
157-197 Buckingham Palace Road Victoria
London SW1W 9SP
Consolidated statement of comprehensive income for the year ended 31 March 2023
table
Consolidated statement of financial position as at 31 March 2023
Table
* A new leasing standard, IFRS 16 Leases , was implemented on 1 April 2022. Right of use assets and borrowings are the only materially impacted financial statement line items. See note 14.6 for more information.
The accompanying notes are an integral part of these accounts.
Amanda Pritchard, Accounting Officer, 21 January 2024.
Consolidated statement of changes in equity for the year ended 31 March 2023
* These adjustments reflect local NHS providers’ adjustments to prior year reserves. The aggregated adjustments are not considered material to the consolidated provider accounts and so prior year balances have not been restated.
** Other reserve movements includes a transfer between charitable funds and NHS provider income and expenditure reserves representing a transfer of resources eliminated from income and expenditure on consolidation.
Consolidated statement of changes in equity for the year ended 31 March 2022
* These adjustments reflect local NHS providers’ adjustments to prior year reserves. The aggregated adjustments are not considered material to the consolidated provider accounts and so prior year balances have not been restated.
** Other reserve movements includes a transfers between charitable funds and NHS provider income and expenditure reserves representing a transfer of resources eliminated from income and expenditure on consolidation.
Information on reserves
Public dividend capital
Public dividend capital (PDC) is a type of public sector equity finance based on the excess of assets over liabilities at the time of establishment of an NHS trust, or predecessor NHS trust where PDC is recognised by a foundation trust. Additional PDC may also be issued to NHS providers by the Department of Health and Social Care to fund capital investment or support operating cash flows. A charge, reflecting the cost of capital utilised by an NHS provider, is payable to the Department of Health and Social Care as the PDC dividend.
Revaluation reserve
Increases in asset values arising from revaluations are recognised in the revaluation reserve, except where, and to the extent that, they reverse impairments previously recognised in operating expenses, in which case they are reversed in operating expenses. Subsequent downward movements in asset valuations are charged to the revaluation reserve to the extent that a previous gain was recognised unless the downward movement represents a clear consumption of economic benefit or a reduction in service potential.
Other reserves
This reserve reflects balances formed on the creation of predecessor NHS bodies, and in some historic mergers before the use of transfer by absorption. Other reserves also include non-controlling interests. Non- controlling interests represent the equity in a subsidiary of an NHS provider which is not attributable, directly or indirectly, to the NHS provider.
Income and expenditure reserve
The balance of this reserve represents the accumulated surpluses and deficits of NHS providers.
NHS charitable funds reserves
This balance represents the ring-fenced funds held by the NHS charitable funds consolidated within these financial statements. These reserves are classified as restricted or unrestricted and a breakdown is provided in note 27.
Consolidated statement of cash flows for the year ended 31 March 2023
table
Total cash and cash equivalents is reconciled to the consolidated statement of financial position in note 17.1.
Cash flows from discontinued operations are not material so are not shown separately on the face of the consolidated statement of cash flows.
Notes to the financial statements
Note 1 Accounting policies and other information
Basis of preparation
Paragraph 1 of Section 65Z4 of the National Health Service Act 2006 (as inserted by Section 14 of the Health and Care Act 2022) requires NHS England to prepare a set of accounts that consolidates the annual accounts of all NHS trusts and NHS foundation trusts for each financial year. This set of accounts is termed the ‘consolidated provider accounts’ and is prepared in accordance with directions issued by the Secretary of State. In line with those directions, these accounts have been prepared in accordance with the Department of Health and Social Care (DHSC) Group Accounting Manual (GAM) 2022/23 and the HM Treasury Financial Reporting Manual (FReM) in relevant respects. ‘NHS providers’ is used as a collective term for NHS trusts and NHS foundation trusts. ‘Trusts’ when not prefixed with ‘NHS’ is also used to mean providers in general.
NHS England is responsible for issuing an accounts direction to NHS foundation trusts under the NHS Act 2006. NHS England directs that the financial statements of NHS foundation trusts shall meet the accounting requirements of the GAM. The GAM is directly applicable to NHS trusts as a result of directions issued by the Secretary of State.
The accounting policies contained within the GAM are broadly consistent with those specified in the FReM, which itself follows UK-adopted International Financial Reporting Standards (IFRS), to the extent that it is meaningful and appropriate in the public sector context. The GAM’s divergences from the FReM are designed to ensure an appropriate financial reporting framework and have been approved by HM Treasury’s Financial Reporting Advisory Board. NHS providers have confirmed their accounting policies are consistent with the GAM in all material respects.
Accounting convention
These financial statements have been prepared under the historical cost convention modified to account for the revaluation of property, plant and equipment, intangible assets and financial instruments that are measured at revalued amounts or fair values at the end of each reporting period, as explained in the accounting policies below.
Consolidated Statement of Comprehensive Income (SOCI) policy
The SOCI in these consolidated accounts is presented to separately identify the surplus or deficit before impairments of non-financial assets and absorption transfers as this is how NHS England (formerly Monitor and the NHS Trust Development Authority (NHS TDA), as part of NHS Improvement) has reported on the performance of NHS providers during the year. We consider that the notional gain/loss associated with a transfer by absorption is outside of the operational performance management of an NHS provider. Impairments and revaluations of property, plant and equipment and other non-financial assets are usually considered outside of a provider’s control. Fair value movements are not included within the ‘impairments and transfers’ column as providers are held to account for the effects of funds
being invested in this way.
Note 1.1 Consolidation and other entities
Basis of consolidation
These accounts consolidate the accounts of all NHS providers that have been in existence during 2022/23 using the principles of IFRS as adopted by the FReM. They present the consolidated results of the NHS provider sector after the elimination of inter-NHS provider balances and transactions. NHS England (and formerly NHS Improvement), is not the parent undertaking for NHS providers and their results are not incorporated within these accounts. As there is no parent entity within this consolidation, only consolidated group statements are presented.
The consolidated provider accounts are prepared based on accounts for each NHS provider which have been audited by the provider’s locally appointed auditor. For 2022/23, two providers’ audits remain incomplete at the time of finalising these disclosures on 15 January 2024. More information is provided in note 31. We are satisfied that the residual uncertainty is not material to these consolidated accounts.
Business combinations and machinery of government changes
Where an NHS provider combines with, transfers a function to, or receives a function from another entity within the Whole of Government Accounts boundary (including other NHS providers) this represents a ‘machinery of government change’ regardless of the mechanism used to effect the combination.
Where functions are transferred to NHS providers from other NHS or local government bodies (or vice versa), the transaction is accounted for as a transfer by absorption. The assets and liabilities transferred are recognised in the accounts as at the date of transfer and prior year comparatives are not restated. The assets and liabilities are not adjusted to fair value prior to recognition. The net gain/loss corresponding to the net assets/liabilities transferred is recognised within non-operating income/expenditure. Where a provider receives assets formerly held by primary care trusts from NHS Property Services or Community Health Partnerships under NHS property guidance announced in May 2019, the corresponding gain is instead recognised in other comprehensive income: this is referred to as ‘modified’ transfer by absorption.
In absorption transfers for property, plant and equipment assets and intangible assets, the cost and accumulated depreciation and amortisation balances from the transferring entity’s accounts are preserved on recognition in the NHS provider accounts. Where the transferring body recognised revaluation reserve balances attributable to the assets, the NHS provider makes a transfer from its income and expenditure reserve to its revaluation reserve. Where DHSC transfers Public Dividend Capital (PDC) from the divesting body to the receiving body as part of an absorption transaction, this is treated as a transfer from the income and expenditure reserve to the PDC reserve by the NHS provider. This ensures that the absorption gain/loss is calculated in line with the requirements of the FReM and also that the balance of PDC is preserved where this is transferred by DHSC.
Where functions are transferred to another NHS or local government body, the assets and liabilities transferred are derecognised from the accounts as at the date of transfer and prior year comparatives are not restated. The net loss / gain corresponding to the net assets / liabilities transferred is recognised within non-operating income/expenditure.
Any revaluation reserve balances attributable to assets de-recognised are transferred to the income and expenditure reserve.
More details of transfers in 2022/23 and 2021/22 are provided in note 30.
Where NHS providers acquire businesses from outside of the Whole of Government Accounts boundary, these are accounted for in accordance with IFRS 3 Business combinations.
Subsidiaries
Under IFRS 10 Consolidated financial statements , an NHS provider controls an investee when it is exposed to, or has rights to, variable returns from its involvement with the investee and has the ability to affect those returns through its power over the investee. Power over the investee occurs where the provider has existing rights that give it the current ability to direct the relevant activities. The income, expenses, assets, liabilities, equity and reserves of subsidiaries are consolidated, in full, into the appropriate financial statement lines. The capital and reserves attributable to non-
controlling interests are included within Other Reserves in the Consolidated Statement of Financial Position.
The amounts consolidated are drawn from the financial results of the subsidiaries for the year, except where a subsidiary’s financial year end is before 1 January or after 1 July. In these cases the actual amounts for each month of the year to 31 March are obtained from the subsidiary and consolidated.
Where a subsidiary’s accounting policies are not aligned with those of the NHS provider (including where they report under UK GAAP) amounts are adjusted during local consolidation where the differences are material. Inter-entity balances, transactions and gains/losses are eliminated in full on consolidation. Subsidiaries classified as ‘held for sale’ are measured at the lower of their carrying value and ‘fair value less costs to sell’.
NHS charitable funds
NHS providers are the corporate trustees to various NHS charitable funds. NHS providers have individually assessed their relationships to the respective charitable funds to determine whether they meet the definition of subsidiaries under IFRS 10. Some NHS providers consolidate their linked NHS charity as a result. Other providers may also have charities meeting the definition of local control that are not locally consolidated on the grounds of materiality. These consolidated accounts only include charities locally consolidated by providers.
The charitable fund’s statutory accounts are prepared to 31 March in accordance with the UK Charities Statement of Recommended Practice (SORP) which is based on UK Generally Accepted Accounting Principles (UK GAAP). On consolidation, necessary adjustments are made to the charity’s assets, liabilities and transactions to:
- recognise and measure them in accordance with the NHS provider’s accounting policies; and
- eliminate intra-group transactions, balances, gains and losses.
Associates
Associate entities are those over which an NHS provider has the power to exercise a significant influence. Associate entities are recognised in these financial statements using the equity method. The investment is initially recognised at cost. It is increased or decreased subsequently to reflect the NHS provider’s share of the entity’s profit or loss or other comprehensive gains and losses (e.g. revaluation gains on the entity’s property, plant and equipment) following acquisition. It is also reduced when any distribution (e.g. share dividends) are received by the NHS provider from the associate.
Associates which are classified as ‘held for sale’ are measured at the lower of their carrying value and ‘fair value less costs to sell’.
Joint ventures
Joint ventures are arrangements in which the NHS provider has joint control with one or more other parties, and where it has the rights to the net assets of the arrangement.
Joint ventures are accounted for using the equity method.
Joint operations
Joint operations are arrangements in which the NHS provider has joint control with one or more other parties and has the rights to the assets, and obligations for the liabilities, relating to the arrangement. The NHS provider includes within its financial statements its share of the assets, liabilities, income and expenses.
Note 1.2 Contract income
Where income is derived from contracts with customers, it is accounted for under IFRS 15 Revenue from contracts with customers . The GAM expands the definition of a contract to include legislation and regulations which enables an entity to receive cash or another financial asset that is not classified as a tax by the Office of National Statistics (ONS)
Revenue in respect of goods/services provided is recognised when (or as) performance obligations are satisfied by transferring promised goods/services to the customer and is measured at the amount of the transaction price allocated to those performance obligations. At the year end, each NHS provider accrues income relating to performance obligations satisfied in that year. Where the provider’s entitlement to consideration for those goods or services is unconditional a contract receivable will be recognised. Where entitlement to consideration is conditional on a further factor other than the passage of time, a contract asset will be recognised. Where consideration received or receivable relates to a performance obligation that is to be satisfied in a future period, the income is deferred and recognised as a contract liability.
Revenue from NHS contracts
The main source of income for NHS providers is contracts with commissioners for healthcare services. Funding envelopes are set at an Integrated Care System (ICS) level. The majority of NHS provider income is earned from NHS commissioners in the form of fixed payments to fund an agreed level of activity. Most contracts run to 31 March in each year.
In 2022/23 fixed payments are set at a level assuming the achievement of elective activity targets. These are termed ‘aligned payment and incentive’ contracts. For some providers, these payments are accompanied by a variable- element to adjust income for actual activity delivered on elective services and advice and guidance services. Where actual elective activity delivered differs from the agreed level set in the fixed payments, the variable element either increases or reduces the income earned by providers at a rate of 75% of the tariff price.
Elective recovery funding provides additional funding for the delivery of elective services. In 2022/23 elective recovery funding was included within the aligned payment and incentive contracts. In 2021/22 income earned by systems based on achievement of elective recovery targets was distributed between individual entities by local agreement and income earned from the fund was accounted for as variable consideration.
Providers also receive income from commissioners under Commissioning for Quality Innovation (CQUIN) and Best Practice Tariff (BPT) schemes. Delivery under these schemes is part of how care is provided to patients. As such CQUIN and BPT payments are not considered distinct performance obligations in their own right; instead they form part of the transaction price for performance obligations under the overall contract with the commissioner. In 2022/23 payment under these schemes is included in fixed payments from commissioners based on assumed achievement of criteria. Adjustments for actual performance are made through the variable element of the contract payments.
Mental health provider collaboratives
NHS led provider collaboratives for specialised mental health, learning disability and autism services involve a lead NHS provider taking responsibility for managing services, care pathways and specialised commissioning budgets for a population. Lead providers are accountable to NHS England and as such recognise the income and expenditure associated with the commissioning of services from other NHS and non NHS providers. Transactions for commissioning of services between NHS providers are eliminated within these accounts.
Revenue from research contracts
Where research contracts fall under IFRS 15, revenue is recognised as and when performance obligations are satisfied. For some contracts, NHS providers assess that the research project constitutes one performance obligation over the course of the multi-year contract. In many cases it is assessed that the provider’s interim performance does not create an asset with alternative use for the provider, and the provider has an enforceable right to payment for the performance completed to date. It is therefore considered that the performance obligation is satisfied over time, and the provider recognises revenue each year over the course of the contract. Some research income alternatively falls within the provisions of IAS 20 Accounting for Government grants.
NHS injury cost recovery scheme
NHS providers receive income under the NHS injury cost recovery scheme, designed to reclaim the cost of treating injured individuals to whom personal injury compensation has subsequently been paid, for instance by an insurer. Providers recognise the income when performance obligations are satisfied. In practical terms this means that treatment has been given, they receive notification from the Department of Work and Pensions’ Compensation Recovery Unit, have completed the NHS2 form and have confirmed there are no discrepancies with the treatment. The income is measured at the agreed tariff for the treatments provided to the injured individual, less an allowance for unsuccessful compensation claims and doubtful debts in line with IFRS 9 Financial instruments requirements of measuring expected credit losses over the lifetime of the asset.
Note 1.3 Other forms of income
Grants and donations
Government grants are grants from Government bodies other than income from commissioners for the provision of services. Where a grant is used to fund revenue expenditure it is credited to operating income to match that expenditure. Where the grant is used to fund capital expenditure, it is credited to the Consolidated Statement of Comprehensive Income once conditions attached to the grant have been met. Donations are treated in the same way as government grants.
Apprenticeship service income
The value of the benefit received when accessing funds from the Government’s apprenticeship service is recognised as income at the point of receipt of the training service. Where these funds are paid directly to an accredited training provider from the NHS provider’s Digital Apprenticeship Service (DAS) account held by the Department for Education, the corresponding notional expense is also recognised at the point of recognition for the benefit.
Note 1.4 Expenditure on employee benefits
Short-term employee benefits
Salaries, wages and employment-related payments, such as social security costs and the apprenticeship levy, are recognised in the period in which the service is received from employees. The cost of annual leave entitlement earned but not taken by employees at the end of the period is recognised in the financial statements to the extent that employees are permitted to carry-forward leave into the following period.
NHS pension scheme
Past and present employees are covered by the provisions of the two NHS Pension Schemes. Details of the benefits payable and rules of the Schemes can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions. Both schemes are unfunded, defined benefit schemes that cover NHS employers, general practices and other bodies, allowed under the direction of the Secretary of State for Health and Social Care in England and Wales. The scheme is not designed to be run in a way that would enable NHS bodies to identify their share of the underlying scheme assets and liabilities. Therefore, the scheme is accounted for as a defined contribution scheme: the cost to the NHS body is taken as equal to the employers’ pension contributions payable to the scheme for the accounting period. The contributions are charged to operating expenses as they become due.
Additional pension liabilities arising from early retirements are not funded by the scheme except where the retirement is due to ill-health. The full amount of the liability for the additional costs is charged to operating expenses at the time of committing to the retirement, regardless of the method of payment.
In order that the defined benefit obligations recognised in the financial statements of the NHS Pension Schemes do not differ materially from those that would be determined at the reporting date by a formal actuarial valuation, the FReM requires that “the period between formal valuations shall be four years, with approximate assessments in intervening years”. An outline of these follows:
a) Accounting valuation
A valuation of scheme liability is carried out annually by the scheme actuary (currently the Government Actuary’s Department) as at the end of the reporting period. This utilises an actuarial assessment for the previous accounting period in conjunction with updated membership and financial data for the current reporting period, and is accepted as providing suitably robust figures for financial reporting purposes. The valuation of scheme liability as at 31 March 2023 is based on valuation data as 31 March 2022, updated to 31 March 2023 with summary global member and accounting data. In undertaking this actuarial assessment, the methodology prescribed in IAS 19, relevant FReM interpretations, and the discount rate prescribed by HM Treasury have also been used.
The latest assessment of the liabilities of the scheme is contained in the scheme actuary report, which forms part of the annual NHS Pension Scheme (England and Wales) Accounts. These accounts can be viewed on the NHS Pensions website and are published annually. Copies can also be obtained from The Stationery Office.
b) Full actuarial (funding) valuation
The purpose of this valuation is to assess the level of liability for the benefits due under the schemes (taking into account their recent demographic experience), and to recommend contribution rates payable by employees and employers.
The latest actuarial valuation undertaken for the NHS Pension Scheme was completed as at 31 March 2016. The results of this valuation set the employer contribution rate payable from April 2019 at 20.6% of pensionable pay.
The actuarial valuation as at 31 March 2020 is currently underway and will set the new employer contribution rate due to be implemented from April 2024.
Other pension schemes
Local Government Pension Scheme
Some NHS providers employ staff who are members of the Local Government Pension Scheme (‘LGPS’) which is a defined benefit pension scheme, administered locally through local pension funds. Where an NHS provider is able to identify its share of the underlying scheme assets and liabilities these are recognised as a defined benefit pension scheme (‘on Statement of Financial Position’) by the provider and are consolidated here. As provider interests in such pension funds are not material to this consolidation, detailed disclosures on movements in scheme assets and liabilities are not disclosed in these accounts but can be found in the accounts of individual NHS providers.
The assets are measured at fair value and the liabilities at the present value of future obligations. The increase in the liability arising from pensionable service earned during the year is recognised within operating expenses. The expected gain during the year from scheme assets is recognised within finance income. The net interest cost during the year arising from the unwinding of the discount on the net scheme liabilities is recognised within finance costs.
Remeasurements of the defined benefit plan are recognised as ‘other comprehensive income’ in the Consolidated Statement of Comprehensive Income.
Where an NHS provider is unable to identify its share of the underlying scheme liabilities these are accounted for as defined contribution pension schemes (‘off Statement of Financial Position’) and employer contributions are charged to expenditure as they fall due. Seven NHS providers recognise LGPS schemes in this way.
Other pension schemes
Some NHS providers have employees who are members of defined benefit pension schemes other than the NHS Pension Scheme and the Local Government Pension Scheme. Where an NHS provider is able to identify its share of the underlying scheme liabilities these are recognised as a defined benefit pension scheme (‘on Statement of Financial Position’). Otherwise, these are recognised as defined contribution pension schemes (‘off Statement of Financial Position’).
There are currently no defined benefit pension arrangements accounted for ‘on Statement of Financial Position’ by NHS providers apart from LGPS schemes.
Defined contribution pension schemes
Some NHS providers have employees who are members of defined contribution pension schemes. In accounting for these schemes trusts recognise expenditure for employer contributions as they fall due. The National Employment Savings Trust (NEST) is a common example of such a scheme.
Note 1.5 Expenditure on other goods and services
Expenditure on goods and services is recognised when, and to the extent that they have been received and is measured at the fair value of those goods and services. Expenditure is recognised in operating expenses except where it results in the creation of a non-current asset such as property, plant and equipment.
Note 1.6 Discontinued operations
Discontinued operations occur where activities either cease without transfer to another entity, or transfer to an entity outside of the boundary of Whole of Government Accounts, such as private or voluntary sectors. Such activities are accounted for in accordance with IFRS 5 Non-current assets held for sale and discontinued operations . Activities that are transferred to other bodies within the boundary of Whole of Government Accounts are ‘machinery of government changes’ and treated as continuing operations.
Note 1.7 Property, plant and equipment
Recognition
Property, plant and equipment is capitalised where:
- it is held for use in delivering services or for administrative purposes;
- it is probable that future economic benefits will flow to, or service potential be provided to, a trust;it is expected to be used for more than one financial year;
- the cost of the item can be measured reliably; and
- the item has cost of at least £5,000; or
- collectively, a number of items have a cost of at least £5,000 and individually have cost of more than £250, where the assets are functionally interdependent, had broadly simultaneous purchase dates, are anticipated to have similar disposal dates and are under single managerial control.
Where a large asset, for example a building, includes a number of components with significantly different asset lives, eg plant and equipment, then these components are treated as separate assets and depreciated over their own useful economic lives.
Subsequent expenditure
Subsequent expenditure relating to an item of property, plant and equipment is recognised as an increase in the carrying amount of the asset when it is probable that additional future economic benefits or service potential deriving from the cost incurred to replace a component of such item will flow to a trust and the cost of the item can be determined reliably. Where a component of an asset is replaced, the cost of the replacement is capitalised if it meets the criteria for recognition above. The carrying amount of the part replaced is de-recognised. Other expenditure that does not generate additional future economic benefits or service potential, such as repairs and maintenance, is charged to the Consolidated Statement of Comprehensive Income in the period in which it is incurred.
Measurement
Valuation
All property, plant and equipment assets are measured initially at cost, representing the costs directly attributable to acquiring or constructing the asset and bringing it to the location and condition necessary for it to be capable of operating in the manner intended by management.
Assets are measured subsequently at valuation. Assets which are held for their service potential and are in use (ie operational assets used to deliver either front line services or back office functions) are measured at their current value in existing use. Assets that were most recently held for their service potential but are surplus with no plan to bring them back into use are measured at fair value where there are no restrictions on sale at the reporting date and where they do not meet the definitions of investment properties or assets held for sale.
Current values in existing use are determined as follows:
- Land and non-specialised buildings – market value in existing use
- Specialised buildings – depreciated replacement cost on a modern equivalent asset basis.
For specialised assets, current value in existing use is interpreted as the present value of the asset’s remaining service potential, which is assumed to be at least equal to the cost of replacing that service potential. In line with the GAM, specialised assets are therefore valued as their depreciated replacement cost (DRC) on a modern equivalent asset (MEA) basis. This valuation method therefore applies to the majority of NHS providers’ property asset base. The MEA method assumes that the existing asset would be replaced with a modern asset of equivalent capacity and function. This asset need not be restricted to the current location and thus, where it would meet the contractual location requirements of the service being provided, an alternative site may instead be used as the basis of valuation. It is for individual NHS providers to determine whether the alternative site approach is appropriate when undertaking an MEA based valuation.
Revaluations of property, plant and equipment are performed with sufficient regularity to ensure that carrying values are not materially different from those that would be determined at the end of the reporting period.
Note 1.25 explains some estimation uncertainties relating to property valuations and explores the impact of these on these consolidated accounts.
Valuation guidance issued by RICS states that valuations are performed net of VAT where the VAT is recoverable by the entity. This commonly applies to schemes procured under a Private Finance Initiative (PFI), where the construction is completed by a special purpose vehicle and the costs have recoverable VAT for a trust.
Properties in the course of construction for service or administration purposes are carried at cost, less any impairment loss. Cost includes professional fees and, where capitalised in accordance with IAS 23 Borrowing costs . Assets are revalued and depreciation commences when the assets are brought into use.
IT equipment, transport equipment, furniture and fittings, and plant and machinery that are held for operational use are valued at depreciated historic cost where these assets have short useful lives or low values or both, as this is not considered to be materially different from current value in existing use.
Depreciation
Items of property, plant and equipment are depreciated over their remaining useful economic lives in a manner consistent with the consumption of economic or service delivery benefits. Land is considered to have an infinite life and is not depreciated.
Property, plant and equipment which has been reclassified as ‘held for sale’ ceases to be depreciated upon the reclassification. Assets in the course of construction and residual interests in off-Statement of Financial Position Private Finance Initiative (PFI) contract assets are not depreciated until the asset is brought into use or reverts to the trust, respectively.
Revaluation gains and losses
Revaluation gains are recognised in the revaluation reserve, except where, and to the extent that, they directly relate to a revaluation decrease that has previously been recognised in operating expenses, in which case they are reversed in operating expenditure. Revaluation losses are charged to the revaluation reserve to the extent that there is an available balance for the asset concerned, and thereafter are charged to operating expenses.
Gains and losses recognised in the revaluation reserve are reported in the Consolidated Statement of Comprehensive Income as an item of ‘other comprehensive income’.
Impairments
In accordance with the GAM, impairments that arise from a clear consumption of economic benefits or of service potential in the asset are charged to operating expenses. A compensating transfer is made from the revaluation reserve to the income and expenditure reserve of an amount equal to the lower of (i) the impairment charged to operating expenses; and (ii) the balance in the revaluation reserve attributable to that asset before the impairment.
An impairment that arises from a clear consumption of economic benefit or of service potential is reversed when, and to the extent that, the circumstances that gave rise to the loss is reversed. Reversals are recognised in operating expenditure to the extent that the asset is restored to the carrying amount it would have had if the impairment had never been recognised. Any remaining reversal is recognised in the revaluation reserve. Where, at the time of the original impairment, a transfer was made from the revaluation reserve to the income and expenditure reserve, an amount is transferred back to the revaluation reserve when the impairment reversal is recognised.
Other impairments are treated as revaluation losses. Reversals of ‘other impairments’ are treated as revaluation gains.
De-recognition
Assets intended for disposal are reclassified as ‘held for sale’ once the criteria in IFRS 5 Non-current assets held for sale and discontinued operations are met. The sale must be highly probable and the asset available for immediate sale in its present condition.
Following reclassification, the assets are measured at the lower of their existing carrying amount and their ‘fair value less costs to sell’. Depreciation ceases to be charged and the assets are not revalued, except where the ‘fair value less costs to sell’ falls below the carrying amount. Assets are de-recognised when all material sale contract conditions have been met.
Property, plant and equipment which is to be scrapped or demolished does not qualify for recognition as ‘held for sale’ and instead is retained as an operational asset and the asset’s economic life is adjusted. The asset is de-recognised when scrapping or demolition occurs.
Donated, government grant and other grant funded assets
Donated and grant funded property, plant and equipment assets are capitalised at their current valuation on receipt. The donation/grant is credited to income at the same time, unless the donor has imposed a condition that the future economic benefits embodied in the grant are to be consumed in a manner specified by the donor, in which case, the donation/grant is deferred within liabilities and is carried forward to future financial years to the extent that the condition has not yet been met.
The donated and grant funded assets are subsequently accounted for in the same manner as other items of property, plant and equipment.
This includes assets donated to providers by the Department of Health and Social Care and NHS England as part of the response to the coronavirus pandemic. As defined in the GAM, providers apply the principle of donated asset accounting to assets that the providers control and are obtaining economic benefits from at the year end.
Private finance initiative (PFI) and Local Improvement Finance Trust (LIFT) transactions PFI and LIFT transactions which meet the IFRIC 12 definition of a service concession, as interpreted in HM Treasury’s FReM, are accounted for as ‘on-Statement of Financial Position’ by NHS providers. In accordance with the FReM, the underlying assets are initially recognised as property, plant and equipment, together with an equivalent liability.
Subsequently, the assets are accounted for as property, plant and equipment and/or intangible assets as appropriate.
The annual contract payments are apportioned between the repayment of the liability, a finance cost and the charges for services. The finance cost is calculated using the implicit interest rate for the scheme. The element of the annual unitary payment increase due to cumulative indexation is treated as contingent rent and is expensed as a finance cost as incurred.
The service charge is recognised in operating expenses and the finance cost is charged to finance costs in the Consolidated Statement of Comprehensive Income. Maintenance spend is charged to operating expenses or capitalised as property, plant and equipment depending upon the nature of the expenditure.
Useful lives of property, plant and equipment
Useful lives assigned to categories of property, plant and equipment vary between NHS providers according to specific local circumstances. The ranges of useful lives across the sector are:
|
Min life years | Max life years | |
|
Buildings, excluding dwellings |
1 |
169 |
|
Dwellings |
1 |
100 |
|
Plant & machinery |
1 |
35 |
|
Transport equipment |
1 |
20 |
|
Information technology |
1 |
30 |
|
Furniture and fittings |
1 |
35 |
Land is not depreciated by NHS providers and so is not included in the above table.
Useful lives reflect the total life of an asset and not the remaining life of an asset. The figures disclosed here are the minimum and maximum used across the provider sector for each category of asset.
Note 1.25 provides further information on the sensitivity of these estimated useful lives.
Note 1.8 Intangible assets
Recognition
Intangible assets are non-monetary assets without physical substance which are capable of being sold separately from the rest of a trust’s business or which arise from contractual or other legal rights. They are recognised only where it is probable that future economic benefits will flow to, or service potential be provided to, the trust and where the cost of the asset can be measured reliably.
Internally generated intangible assets
Internally generated goodwill, brands, mastheads, publishing titles, customer lists and similar items are not capitalised as intangible assets.
Expenditure on research is not capitalised. Expenditure on development is capitalised when it meets the requirements set out in IAS 38 Intangible assets .
Software
Software which is integral to the operation of hardware, eg an operating system, is capitalised as part of the relevant item of property, plant and equipment. Software which is not integral to the operation of hardware, eg application software, is capitalised as an intangible asset.
Measurement
Intangible assets are recognised initially at cost, comprising all directly attributable costs needed to create, produce and prepare the asset to the point that it is capable of operating in the manner intended by management.
Subsequently intangible assets are measured at current value in existing use. Where no active market exists, intangible assets are valued at the lower of depreciated replacement cost and the value in use where the asset is income generating. Revaluations gains and losses and impairments are treated in the same manner as for property, plant and equipment. Assets that were most recently held for their service potential but are surplus with no plan to bring them back into use are measured at fair value where there are no restrictions on sale at the reporting date and where they do not meet the definition of an asset held for sale.
Intangible assets ‘held for sale’ are measured at the lower of their carrying amount or ‘fair value less costs to sell’.
Amortisation
Intangible assets are amortised over their expected useful lives in a manner consistent with the consumption of expected economic or service delivery benefits.
Useful lives assigned to categories of intangible asset vary between NHS providers according to specific local circumstances. The range of useful lives across the sector is:
|
Min life years | Max life years | |
|
Intangible assets – internally generated |
| |
|
Information technology | 1 |
20 |
|
Development expenditure | 1 |
12 |
|
Websites | 1 |
10 |
|
Intangible assets – purchased |
| |
|
Software |
1 |
21 |
|
Licences & trademarks |
1 |
20 |
|
Goodwill |
99 |
99 |
|
Other |
1 |
21 |
Useful lives reflect the total life of an asset and not the remaining life of an asset. The figures disclosed here are the minimum and maximums used across the provider sector for each category of asset.
Note 1.9 Investment properties
Investment properties are measured at fair value. Changes in fair value are recognised as gains or losses in income/expenditure.
Only those assets which are held solely to generate a commercial return are considered to be investment properties. Where an asset is held, in part, for support service delivery objectives, then it is considered to be an item of property, plant and equipment. Properties occupied by employees, whether or not they pay rent at market rates, are not classified as investment properties.
Note 1.10 Leases
A lease is a contract or part of a contract that conveys the right to use an asset for a period of time in exchange for consideration. An adaptation of the relevant accounting standard by HM Treasury for the public sector means that for NHS bodies, this includes lease-like arrangements with other public sector entities that do not take the legal form of a contract. It also includes peppercorn leases where consideration paid is nil or nominal (significantly below market value) but in all other respects meet the definition of a lease. NHS providers do not apply lease accounting to new contracts for the use of intangible assets.
A trust determines the term of the lease term with reference to the non-cancellable period and any options to extend or terminate the lease which the trust is reasonably certain to exercise.
NHS providers as lessees
Initial recognition and measurement
At the commencement date of the lease, being when the asset is made available for use, providers recognise a right of use asset and a lease liability.
The right of use asset is recognised at cost comprising the lease liability, any lease payments made before or at commencement, any direct costs incurred by the lessee, less any cash lease incentives received. It also includes any estimate of costs to be incurred restoring the site or underlying asset on completion of the lease term.
The lease liability is initially measured at the present value of future lease payments discounted at the interest rate implicit in the lease. Lease payments includes fixed lease payments, variable lease payments dependent on an index or rate and amounts payable under residual value guarantees. It also includes amounts payable for purchase options and termination penalties where these options are reasonably certain to be exercised.
Where an implicit rate cannot be readily determined, a provider’s incremental borrowing rate is applied. This rate is determined by HM Treasury annually for each calendar year. A nominal rate of 0.95% applied to new leases commencing in 2022 and 3.51% to new leases commencing in 2023.
Providers do not apply the above recognition requirements to leases with a term of 12 months or less or to leases where the value of the underlying asset is below £5,000, excluding any irrecoverable VAT. Lease payments associated with these leases are expensed on a straight line or other systematic basis over the lease term.
Irrecoverable VAT on lease payments is expensed as it falls due.
Subsequent measurement
As required by a HM Treasury interpretation of the accounting standard for the public sector, the providers employ a revaluation model for subsequent measurement of right of use assets, unless the cost model is considered to be an appropriate proxy for current value in existing use or fair value, in line with the accounting policy for owned assets. Where consideration exchanged is identified as significantly below market value, the cost model is not considered to be an appropriate proxy for the value of the right of use asset.
Providers subsequently measure the lease liability by increasing the carrying amount for interest arising which is also charged to expenditure as a finance cost and reducing the carrying amount for lease payments made. The liability is also remeasured for changes in assessments impacting the lease term, lease modifications or to reflect actual changes in lease payments. Such remeasurements are also reflected in the cost of the right of use asset. Where there is a change in the lease term or option to purchase the underlying asset, an updated discount rate is applied to the remaining lease payments.
NHS providers as lessors
Providers assess each of their leases and classify them as either finance leases or operating leases. Leases are classified as finance leases when substantially all the risks and rewards of ownership are transferred to the lessee. All other leases are classified as operating leases.
Where a provider is an intermediate lessor, classification of the sublease is determined with reference to the right of use asset arising from the headlease.
Finance leases
Amounts due from lessees under finance leases are recorded as receivables at the amount of the provider’s net investment in the leases. Finance lease interest income is allocated to accounting periods to reflect a constant periodic rate of return on the provider’s net investment.
Operating leases
Income from operating leases is recognised on a straight-line basis or another systematic basis over the term of the lease. Initial direct costs incurred in negotiating and arranging an operating lease are added to the carrying amount of the leased asset and recognised as an expense on a straight-line basis over the lease term.
Initial application of IFRS 16
IFRS 16 Leases as adapted and interpreted for the public sector by HM Treasury has been applied to these financial statements with an initial application date of 1 April 2022. IFRS 16 replaces IAS 17 Leases, IFRIC 4 Determining whether an arrangement contains a lease and other interpretations.
The standard has been applied using a modified retrospective approach with the cumulative impact recognised in the income and expenditure reserve on 1 April 2022. Upon initial application, the provisions of IFRS 16 have only been applied to existing contracts where they were previously deemed to be a lease or contain a lease under IAS 17 and IFRIC 4. Where existing contracts were previously assessed not to be or contain a lease, these assessments have not been revisited.
NHS providers as lessees
For continuing leases previously classified as operating leases, a lease liability was established on 1 April 2022 equal to the present value of future lease payments discounted at the HM Treasury incremental borrowing rate of 0.95%. A right of use asset was created equal to the lease liability and adjusted for prepaid and accrued lease payments and deferred lease incentives recognised in the statement of financial position immediately prior to initial application.
Hindsight has been used in determining the lease term where lease arrangements contain options for extension or earlier termination.
No adjustments have been made on initial application in respect of leases with a remaining term of 12 months or less from 1 April 2022 or for leases where the underlying assets has a value below £5,000. No adjustments have been made in respect of leases previously classified as finance leases.
NHS providers as lessors
Leases of owned assets where a trust is lessor were unaffected by initial application of IFRS 16. For existing arrangements where a provider is an intermediate lessor, classification of all continuing sublease arrangements has been reassessed with reference to the right of use asset.
2021/22 comparatives
Comparatives for leasing transactions in these accounts have not been restated on an IFRS 16 basis. Under IAS 17 the classification of leases as operating or finance leases, still applicable to lessors under IFRS 16, also applied to lessees. In 2021/22 lease payments made by providers in respect of leases previously classified as operating leases were charged to expenditure on a straight line or other systematic basis.
Note 1.11 Inventories
Inventories are valued at the lower of cost and net realisable value. NHS providers measure the cost of inventories using either a first in first out (FIFO) method or the weighted average cost method.
Providers received inventories including personal protective equipment from the DHSC at nil cost. In line with the GAM and applying the principles of the IFRS Conceptual Framework, providers have accounted for the receipt of personal protective equipment at a deemed cost, reflecting the best available approximation of an imputed market value for the transaction.
The DHSC GAM determined that providers act as an agent of DHSC or the UK Health Security Agency in respect of vaccines and testing kits. Accordingly, such items are not recognised as inventory or an expense in NHS providers’ accounts.
Note 1.12 Financial assets and financial liabilities
Recognition
Financial assets and financial liabilities arise where providers are party to the contractual provisions of a financial instrument, and as a result have a legal right to receive or a legal obligation to pay cash or another financial instrument. The GAM expands the definition of a contract to include legislation and regulations which give rise to arrangements that in all other respects would be a financial instrument and do not give rise to transactions classified as a tax by ONS.
This includes the purchase or sale of non-financial items (such as goods or services), which are entered into in accordance with the provider’s normal purchase, sale or usage requirements and are recognised when, and to the extent which, performance occurs, ie, when receipt or delivery of the goods or services is made.
Classification and measurement
Financial assets and financial liabilities are initially measured at fair value plus or minus directly attributable transaction costs except where the asset or liability is measured at fair value through income and expenditure. Fair value is taken as the transaction price, or otherwise determined by reference to quoted market prices or valuation techniques.
Financial assets or financial liabilities in respect of assets acquired or disposed of through leasing arrangements are recognised and measured in accordance with the accounting policy for leases described in note 1.10.
Financial assets are subsequently measured at amortised cost, fair value through income and expenditure or fair value through other comprehensive income.
Financial liabilities are subsequently measured at amortised cost or fair value through income and expenditure.
Financial assets and financial liabilities at amortised cost
Financial assets at amortised cost are those where cash flows are solely payments of principal and interest. Financial assets and liabilities subsequently measured at amortised cost include cash equivalents, contract and other receivables, trade and other payables, rights and obligations under lease arrangements and loans receivable and payable.
After initial recognition, these financial assets and financial liabilities are measured at amortised cost using the effective interest method less any impairment (for financial assets). The effective interest rate is the rate that exactly discounts estimated future cash payments or receipts through the expected life of the financial asset or financial liability to the gross carrying amount of a financial asset or to the amortised cost of a financial liability.
Interest revenue or expense is calculated by applying the effective interest rate to the gross carrying amount of a financial asset or amortised cost of a financial liability and recognised in the Consolidated Statement of Comprehensive Income and a financing income or expense. In the case of loans held from the Department of Health and Social Care, the effective interest rate is the nominal rate of interest charged on the loan.
Financial assets measured at fair value through other comprehensive income
Financial assets that are debt instruments are measured at fair value through other comprehensive income where business model objectives are met by both collecting contractual cash flows and selling financial assets and where the cash flows are solely payments of principal and interest. Movements in the fair value of financial assets in this category are recognised as gains or losses in other comprehensive income except for impairment losses. On derecognition, cumulative gains and losses previously recognised in other comprehensive income are reclassified from equity to income and expenditure.
In some cases providers have irrevocably elected to measure some equity instruments at fair value through other comprehensive income. This is not material to these consolidated accounts.
Financial assets and financial liabilities at fair value through income and expenditure
Financial assets measured at fair value through income and expenditure are those that are not otherwise measured at amortised cost or at fair value through other comprehensive income. This category also includes financial assets and liabilities acquired principally for the purpose of selling in the short term (held for trading) and derivatives. Derivatives which are embedded in other contracts, but which are separable from the host contract are measured within this category. Movements in the fair value of financial assets and liabilities in this category are recognised as gains or losses within surplus / (deficit) for the year.
In some cases providers have irrevocably elected to measure some financial assets at fair value through income and expenditure. This is not material to these consolidated accounts.
Impairment of financial assets
For all financial assets measured at amortised cost including lease receivables, contract receivables and contract assets or assets measured at fair value through other comprehensive income, providers recognise an allowance for expected credit losses.
Providers adopt the simplified approach to impairment for contract and other receivables, contract assets and lease receivables, measuring expected losses as at an amount equal to lifetime expected losses. For other financial assets, the loss allowance is initially measured at an amount equal to 12-month expected credit losses (stage 1) and subsequently at an amount equal to lifetime expected credit losses if the credit risk assessed for the financial asset significantly increases (stage 2).
For financial assets that have become credit impaired since initial recognition (stage 3), expected credit losses at the reporting date are measured as the difference between the asset’s gross carrying amount and the present value of estimated future cash flows discounted at the financial asset’s original effective interest rate.
Expected losses are charged to operating expenditure within the Consolidated Statement of Comprehensive Income and reduce the net carrying value of the financial asset in the Consolidated Statement of Financial Position.
De-recognition
Financial assets are de-recognised when contractual cash flows have been received or the provider has transferred substantially all the risks and rewards of ownership. A financial asset may also be written off when there is deemed no realistic prospect of recovery, at which point any loss in excess of credit loss allowances already recognised will be charged to operating expenditure.
Financial liabilities are de-recognised when the obligation is discharged, cancelled or expires.
Note 1.13 Cash and cash equivalents
Cash and cash equivalents comprise cash at bank, in hand and cash equivalents. Cash equivalents are readily convertible investments of known value which are subject to an insignificant risk of change in value and usually mature within 3 months or less from the date of acquisition.
In the Statement of Cash Flows, cash and cash equivalents are shown net of bank overdrafts that are repayable on demand and that form an integral part of a trust’s cash management. Cash, bank and overdraft balances are recorded at current values.
Note 1.14 Third party assets
Assets belonging to third parties in which a NHS provider has no beneficial interest (such as money held on behalf of patients) are not recognised in the accounts since an NHS provider has no beneficial interest in them. They are disclosed in a separate note to the accounts in accordance with the requirements of the FReM (see note 17.2 to the accounts).
Note 1.15 Provisions
An NHS provider recognises a provision where it has a present legal or constructive obligation of uncertain timing or amount; for which it is probable that there will be a future outflow of cash or other resources; and a reliable estimate can be made of the amount. The amount recognised in the Consolidated Statement of Financial Position is the best estimate of the resources required to settle the obligation.
Where the effect of the time value of money is significant, the estimated risk-adjusted cash flows are discounted using the HM Treasury’s discount rates effective for 31 March 2023.
Nominal rate | Prior year rate | ||
|---|---|---|---|
| Short-term | Up to 5 years | 3.27% | 0.47% |
| Medium-term | After 5 years up to 10 years | 3.20% | 0.70% |
| Long-term | After 10 years up to 40 years | 3.51% | 0.95% |
| Very long-term | Exceeding 40 years | 3.00% | 0.66% |
HM Treasury provides discount rates for general provision on a nominal rate basis. Expected future cash flows are therefore adjusted for the impact of inflation before discounting using nominal rates. The following inflation rates are set by HM Treasury, effective 31 March 2023.
Inflation rate | Prior year rate | |
|---|---|---|
| Year 1 | 7.40% | 4.00% |
| Year 2 | 0.60% | 2.60% |
| Into perpetuity | 2.00% | 2.00% |
Early retirement provisions and injury benefit provisions both use the HM Treasury’s pension discount rate of 1.70% in real terms (minus 1.3% at 31 March 2022).
Clinical negligence costs
NHS Resolution operates a risk pooling scheme under which an NHS provider pays an annual contribution to NHS Resolution, which, in return, settles all clinical negligence claims. Although NHS Resolution is administratively responsible for all clinical negligence cases, the legal liability remains with an NHS provider. The total value of clinical negligence provisions carried by NHS Resolution on behalf of NHS providers is disclosed at note 21.3.
Non-clinical risk pooling
NHS providers can participate in the Property Expenses Scheme and the Liabilities to Third Parties Scheme. Both are risk pooling schemes under which an NHS provider pays an annual contribution to NHS Resolution and, in return, receives assistance with the costs of claims arising. The annual membership contributions, and any ‘excesses’ payable in respect of particular claims are charged to operating expenses when the liability arises.
Note 1.16 Contingencies
Contingent assets (that is, assets arising from past events whose existence will only be confirmed by one or more future events not wholly within the entity’s control) are not recognised as assets, but are disclosed in note 22 where an inflow of economic benefits is probable.
Contingent liabilities are not recognised, but are disclosed in note 22, unless the probability of a transfer of economic benefits is remote. Contingent liabilities are defined as:
- possible obligations arising from past events whose existence will be confirmed only by the occurrence of one or more uncertain future events not wholly within the entity’s control; or
- present obligations arising from past events but for which it is not probable that a transfer of economic benefits will arise or for which the amount of the obligation cannot be measured with sufficient reliability.
Note 1.17 Public dividend capital
Public dividend capital (PDC) is a type of public sector equity finance based on the excess of assets over liabilities at the time of establishment of the NHS trust or predecessor NHS trust in the case for NHS foundation trusts. The Secretary of State can issue new PDC to, and require repayments of PDC from NHS providers. HM Treasury has determined that PDC is not a financial instrument within the meaning of IAS 32 Financial instruments: presentation . PDC is recorded at the value received.
A charge, reflecting the cost of capital utilised by the trust, is payable as public dividend capital dividend. The charge is calculated at the rate set by HM Treasury (currently 3.5%) on the average relevant net assets of the trust during the financial year. Relevant net assets are calculated as the value of all assets less the value of all liabilities, with certain additions and deductions as defined in the PDC dividend policy issued by the Department of Health and Social Care.
In accordance with the requirements laid down by the Department of Health and Social Care (as the issuer of PDC), the dividend for the year is calculated on the actual average relevant net assets as set out in the “pre-audit” version of the annual accounts. The dividend thus calculated is not revised should any adjustment to net assets occur as a result the audit of the annual accounts.
Note 1.18 Value added tax
Most of the activities of NHS providers are outside the scope of VAT and, in general, output tax does not apply and input tax on purchases is not recoverable. Irrecoverable VAT is charged to the relevant expenditure category or included in the capitalised purchase cost of fixed assets. Where output tax is charged or input VAT is recoverable, the amounts are stated net of VAT. Where an NHS provider consolidates the activities of a subsidiary, these activities may be within the scope of VAT rules.
Note 1.19 Corporation tax
The Finance Act 2004 amended S519A Income and Corporation Taxes Act 1998 to provide power to HM Treasury to make certain non-core activities of NHS providers potentially subject to corporation tax. NHS providers may also incur corporation tax liabilities through subsidiaries which are consolidated into their financial statements.
Corporation tax expense recognised in these financial statements represents the sum of the tax currently payable and deferred tax.
Current tax is the expected tax payable on the taxable surpluses generated during the year, using tax rates enacted or substantively enacted at the end of the reporting period, and any adjustments to tax payable in respect of previous years.
Note 1.20 Climate change levy
Expenditure on the climate change levy is recognised in the Consolidated Statement of Comprehensive Income as incurred, based on the prevailing chargeable rates for energy consumption.
Note 1.21 Foreign exchange
The functional and presentation currency of NHS providers is sterling. A transaction which is denominated in a foreign currency is translated into the functional currency at the spot exchange rate on the date of the transaction.
Where an NHS provider has assets or liabilities denominated in a foreign currency at the reporting date:
- monetary items (other than financial instruments measured at ‘fair value through income and expenditure’) are translated at the spot exchange rate on 31 March;
- non-monetary assets and liabilities measured at historical cost are translated using the spot exchange rate at the date of the transaction; and
- non-monetary assets and liabilities measured at fair value are translated using the spot exchange rate at the date the fair value was determined.
Exchange gains or losses on monetary items (arising on settlement of the transaction or on re-translation at the reporting date) are recognised as income or expense in the period in which they arise. Exchange gains or losses on non-monetary assets and liabilities are recognised in the same manner as other gains and losses on these items.
Note 1.22 Losses and special payments
Losses and special payments are items that Parliament would not have contemplated when it agreed funds for the health service or passed legislation. By their nature they are items that ideally would not arise. They are therefore subject to special control procedures compared with the generality of payments. They are divided into different categories, which govern the way that individual cases are handled. Losses and special payments are charged to the relevant functional headings in expenditure on an accruals basis.
Losses and special payments notes within individual NHS provider financial statements are compiled directly from each trust’s losses and compensations register which reports on an accruals basis without provisions for future losses.
Note 1.23 Gifts
Gifts are items that are voluntarily donated, with no preconditions and without the expectation of any return. Gifts include all transactions economically equivalent to free and unremunerated transfers, such as the loan of an asset for its expected useful life, and the sale or lease of assets at below market value.
Note 1.24 Going concern
HM Treasury’s Financial Reporting Manual (FReM) defines that a public sector body that is not classified as a trading entity will be a going concern where there is the anticipated continuation of the provision of services in the future. The same definition is applied by NHS providers in preparing their financial statements. All NHS provider financial statements have been prepared on a going concern basis in 2022/23. NHS England has prepared these consolidated financial statements on a going concern basis which reflects the basis on which the underlying accounts have been prepared with the sector having no material uncertainty to disclose. This is consistent with the current and future
funding confirmed for the NHS by Parliament and the Government.
Note 1.25 Critical accounting judgements and key sources of estimation uncertainty
These consolidated NHS provider accounts reflect the following accounting judgements made either by NHS England or individual NHS providers:
- Intra-group transactions and balances between NHS providers are eliminated upon consolidation. Where differences are identified in the amounts recorded, adjustments are made to these amounts to ensure all intra- group balances eliminate. Any difference between these amounts and the amounts recognised as expenditure and payables are not further adjusted as these net amounts are not material.
We are satisfied that the gross mismatches which net together to this immaterial position do not constitute a material error.
- These consolidated accounts are prepared on a going concern basis as detailed within accounting policy 1.24.
- Individual NHS providers apply judgement in their application of the nationally prescribed accounting policies set out in the DHSC GAM.
The following are the key sources of estimation uncertainty:
- Measurement of specialised non-current assets: Property plant and equipment is measured using the revaluation model in IAS 16 Property, plant and equipment as set out in accounting policy 1.7. This measurement basis also applies to right of use assets unless cost is deemed to be an appropriate proxy for valuation as detailed in accounting policy 1.10. In applying RICS guidance to valuing an asset, the valuation used by the NHS provider will depend on the local assumptions and data used, including the floor area for assets. For a specialised asset valued on a depreciated replacement cost (DRC) basis as a modern equivalent asset (MEA), this includes the assumption of whether ‘alternative site’ or ‘no alternative site’ is used for the valuation. Further, RICS guidance says that valuations should be stated net of VAT where VAT would be recoverable on the cost of replacing the service potential. Whether this is applicable in each local valuation is a matter of local judgement, with guidance on the parameters for this judgement provided in the DHSC GAM. The accounting policy of DRC:MEA is applied consistently for specialised assets across NHS providers, but local valuation assumptions may have material effects on each local valuation.
- Useful lives of PPE: as shown in note 13.1, property plant and equipment (PPE) is material to these consolidated accounts. In note 1.7 we disclose, for each category of PPE, the lowest minimum and the highest maximum in the ranges of useful lives used by providers. Useful lives are the period over which assets are depreciated. We do not collect information from providers on average useful lives, but in taking the median average lowest and median average highest, and the mean average of those, an approximate average can be computed to assess the impact of the accounting estimates.
As shown in note 13.1, buildings and plant and equipment depreciation comprise 46% and 29% of total PPE depreciation charged in-year respectively. Utilising the methodology outlined above, a very approximate average useful life in these categories is 38.5 years and 10 years respectively. In average terms, making all asset lives one year shorter would increase the annual depreciation charge by approximately £34 million for buildings and
£92 million for plant and machinery. This is not material. Based on a materiality of £1.15 billion, eight times this ‘one year effect’ would be required to lead to a material error based on these approximate averages.
The depreciation charge in these accounts comprises the depreciation charges in each provider’s accounts, which in themselves relate to many assets. It is therefore not possible to thoroughly interrogate this accounting estimate upon consolidation, but given the impact locally each provider’s accounting estimates in this area are subject to review by each local external auditor.
- Measurement of lease liabilities and right of use assets for lease-like arrangements with public sector entities that do not take the legal form of a contract: In accordance with accounting policy 1.10, where formal documentation does not exist for a lease-like arrangement with a public sector body, providers must calculate lease liabilities and initial right of use asset values with reference to an expected lease term. Providers will estimate expected lease term based on the commercial reality of the arrangement and current plans for estates and service provision. This increases the estimation uncertainty in the measurement of these balances. For example, if a lease term was assessed at 25 years instead of 20 years on initial application of IFRS 16, this would result in a 22% increase in the liability recognised for that lease on 1 April 2022, but no impact on net assets on transition. The bases for such judgements are subject to review by each local external auditor.
Critical accounting estimates and judgements made in the preparation of individual NHS provider accounts are disclosed locally by each NHS provider.
Note 1.26 Early adoption of standards, amendments and interpretations
The consolidated NHS Provider financial statements have not adopted any IFRSs, amendments or interpretations early.
Note 1.27 Standards, amendments and interpretations in issue but not yet effective or adopted
IAS 8 Accounting policies, changes in accounting estimates and errors , requires disclosure in respect of new IFRSs, amendments and interpretations that are, or will be, applicable after the accounting period. There are a number of IFRSs, amendments and interpretations issued by the International Accounting Standards Board that are effective for financial statements after this accounting period.
| Standard | Description of amendment | Effective date |
|---|---|---|
| Standards, amendments or interpretations issued and effective from 2023/24: | ||
|
IFRS 16 Leases (FReM adaptation in respect of service concession arrangements) | FReM adaptation applying IFRS 16 measurement principles to liabilities held under service concession arrangements in the public sector |
Effective from 1 April 2023. |
|
IAS 1 Presentation of financial statements (amendments) and IFRS Practice Statement 2 | Amendments relating to disclosing material accounting policies instead of significant accounting policies |
Annual periods beginning on or after 1 January 2023. |
|
IAS 12 Income taxes (amendments) | Amendments to clarify how entities account for deferred tax on transactions such as leases and decommissioning obligations. |
Annual periods beginning on or after 1 January 2023. |
|
IAS 8 Accounting policies, changes in accounting estimates and errors (amendment) | Amendments relating to the definition of accounting estimates |
Annual periods beginning on or after 1 January 2023. |
| Standard | Description of amendment | Effective date |
|---|---|---|
| Standards, amendments or interpretations issued and effective for later periods: | ||
|
IAS 1 Presentation of financial statements (amendments) |
Amendments regarding the classification of liabilities |
Annual periods beginning on or after 1 January 2024. Not yet endorsed for use in the UK. |
|
IFRS 16 Leases (amendments) |
Amendments relating to the lease liability in sale and leaseback transactions |
Annual periods beginning on or after 1 January 2024. Not yet adopted by the FReM. |
|
IFRS 17 Insurance contracts |
Original issue and subsequent amendments |
The Standard applies to annual periods beginning on or after 1 January 2023. Adoption in the UK public sector is expected for the 2025/26 financial year onwards. |
|
IAS 12 Income taxes (amendments) |
Amendments relating to international tax reform |
Not yet endorsed for use in the UK |
Estimated impact of future standards
IFRS 16 Leases – application of liability measurement principles to PFI and other service concession (IFRIC 12) arrangements
From 1 April 2023, the measurement principles of IFRS 16 Leases will also be applied to NHS providers’ PFI liabilities where future payments are linked to a price index representing inflation. The PFI liability will be remeasured when a change in the index causes a change in future repayments and that change has taken effect in the cash flow. Such remeasurements will be recognised as a financing cost. Under existing accounting practices, amounts relating to changes in the price index are expensed as incurred.
Initial application of these principles will be on 1 April 2023 using a modified retrospective approach with the cumulative impact taken to reserves. This is expected to result in increased PFI liabilities on the statement of financial position. The effect of this has not yet been quantified.
Note 2 Operating segment
The NHS provider sector is formed of five types of NHS provider, supplying different services: acute, ambulance, community, mental health and specialist. This classification is based on the majority of the provider’s income: i.e. each provider is allocated to a single segment. Each NHS provider also belongs to one of seven regions.
These are two alternative segmental analyses. NHS England does not allocate resources between these segments; however this is the basis on which the performance of the NHS provider sector is reported internally. NHS England is not the parent of NHS providers and as such does not have a function that meets the definition of the chief operating decision maker in IFRS 8 Operating segments.
Net assets are not split between segments in our internal reporting and so are not split by segment here.
The figures reported below include inter-NHS provider trust income and expenditure and these are removed in reconciling to the Consolidated Statement of Comprehensive Income overleaf. The figures below exclude amounts relating to NHS charitable funds which are excluded for our regulatory analysis. The impact of consolidating charitable funds is added in to the reconciliation to the Consolidated Statement of Comprehensive Income overleaf.
Analysis by type of trust
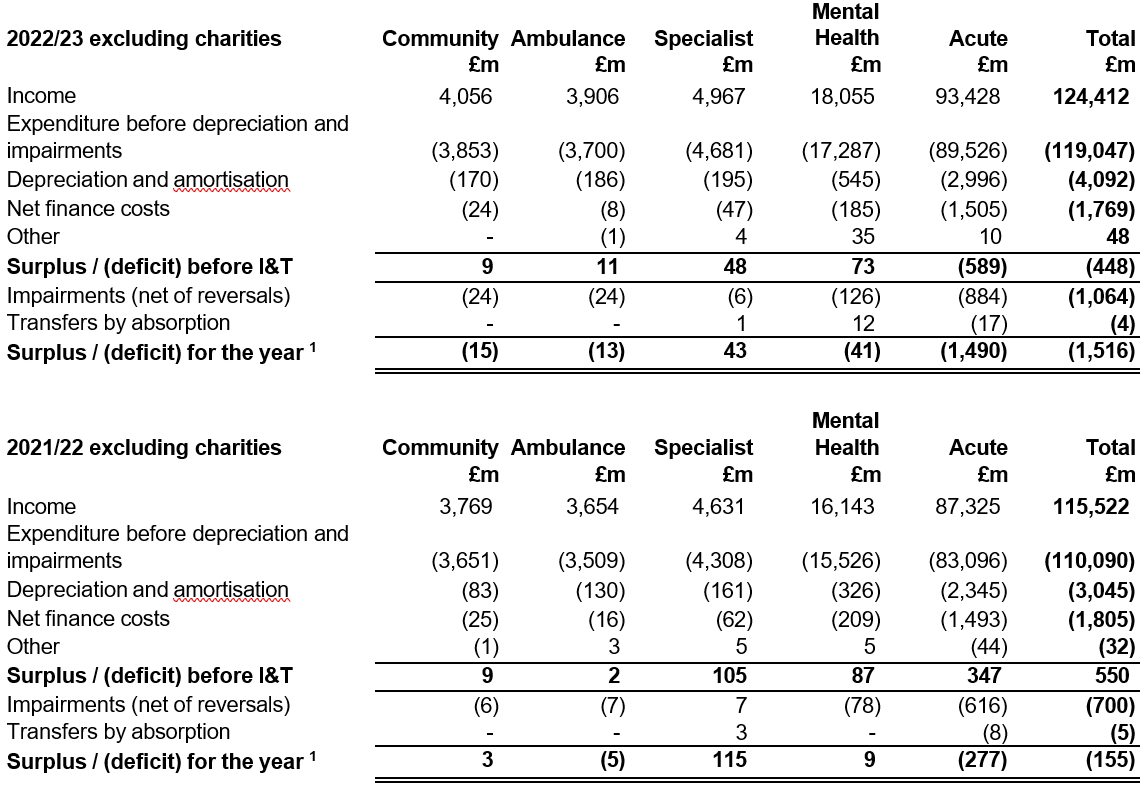
(1) These totals are after impairments and transfers but exclude consolidated charitable funds.
Analysis by region
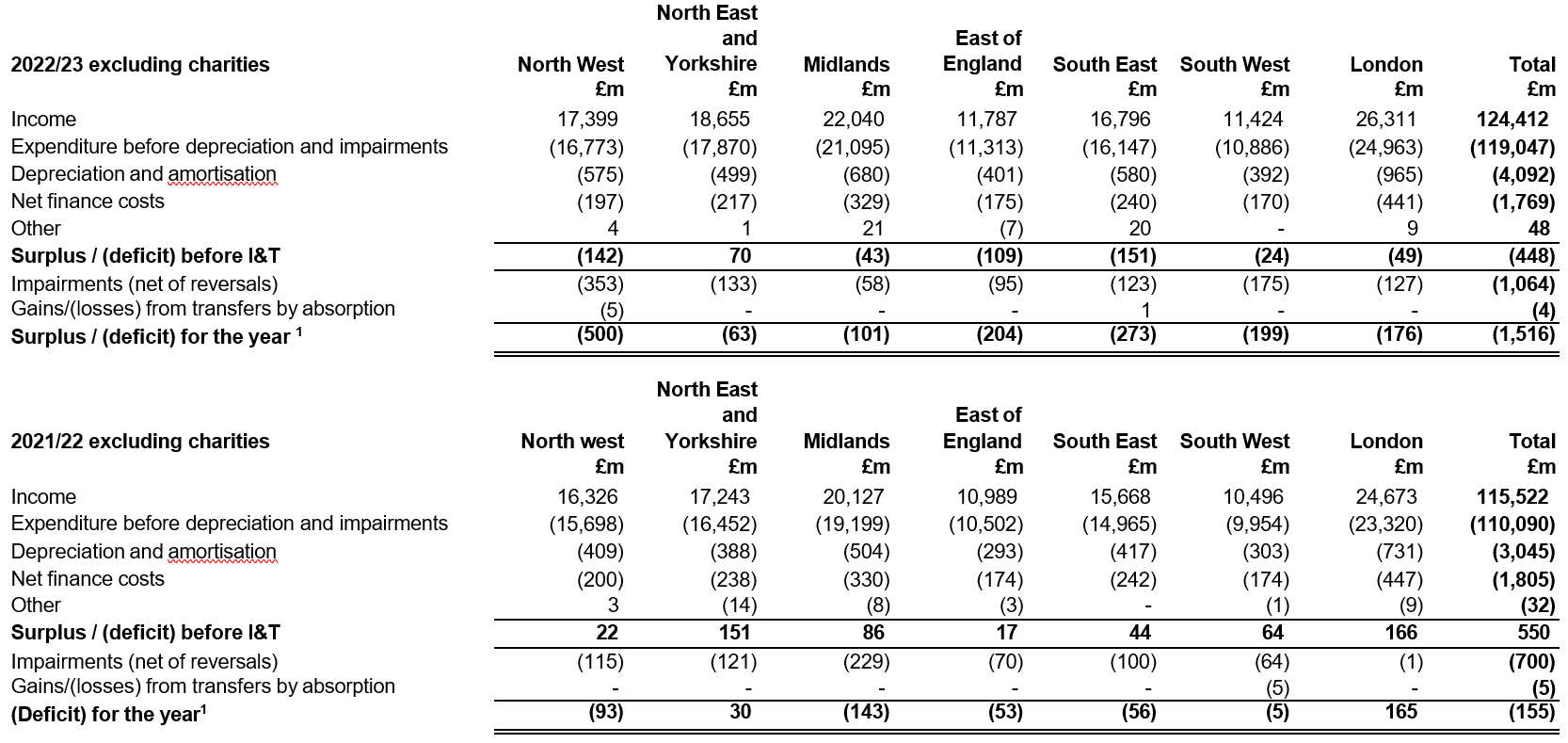
(1) These totals are after impairments and transfers but before the consolidation of charitable funds and the elimination of inter-provider leases.
Reconciliation to Consolidated Statement of Comprehensive Income
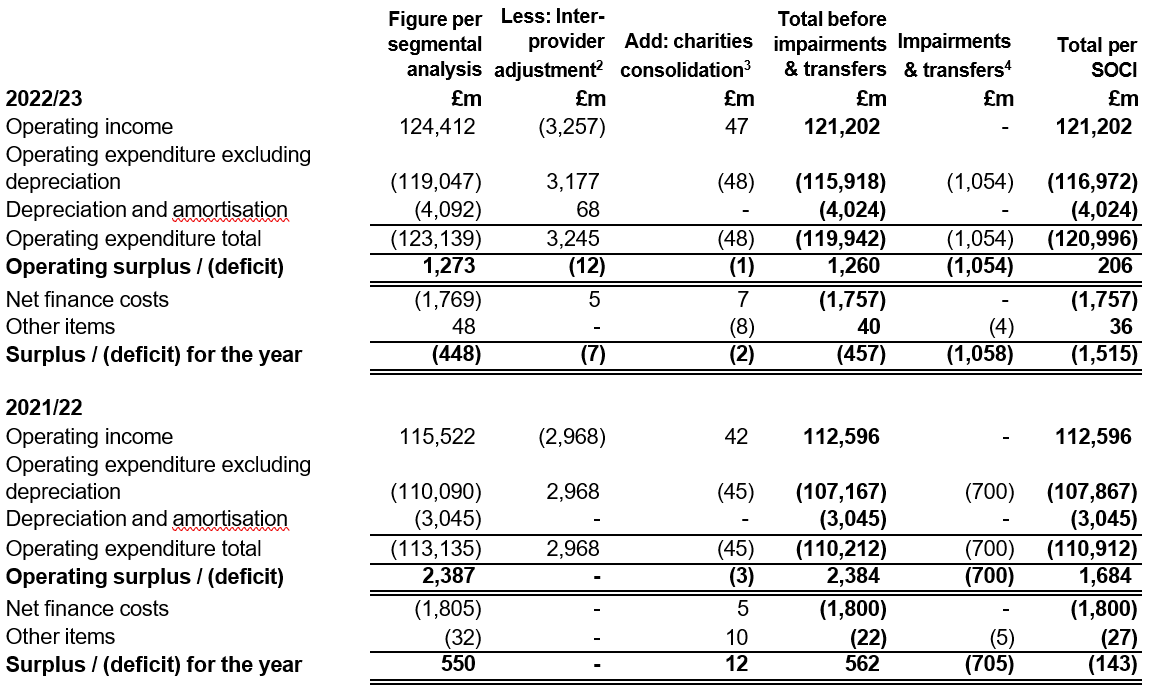
(2) These numbers represent the elimination of transactions between NHS providers. The adjustments include the alignment of accounting treatment for lease arrangements between providers which is no longer consistent between the lessee and lessor following the adoption of IFRS 16 Leases .
(3) These numbers reflect the impact of consolidating NHS charitable funds including local intra-group eliminations. These numbers do not represent total income and expenditure in NHS charitable funds.
(4) The net impairments figure in this reconciliation excludes impairments to right of use assets held under inter-provider leases eliminated on consolidation therefore does not match the impairments figure seen in the segmental reporting analysis.
Note 3 Operating income from patient care activities
All income from patient care activities relates to contract income recognised in line with accounting policy 1.2.
Note 3.1 Income from patient care activities (by nature)
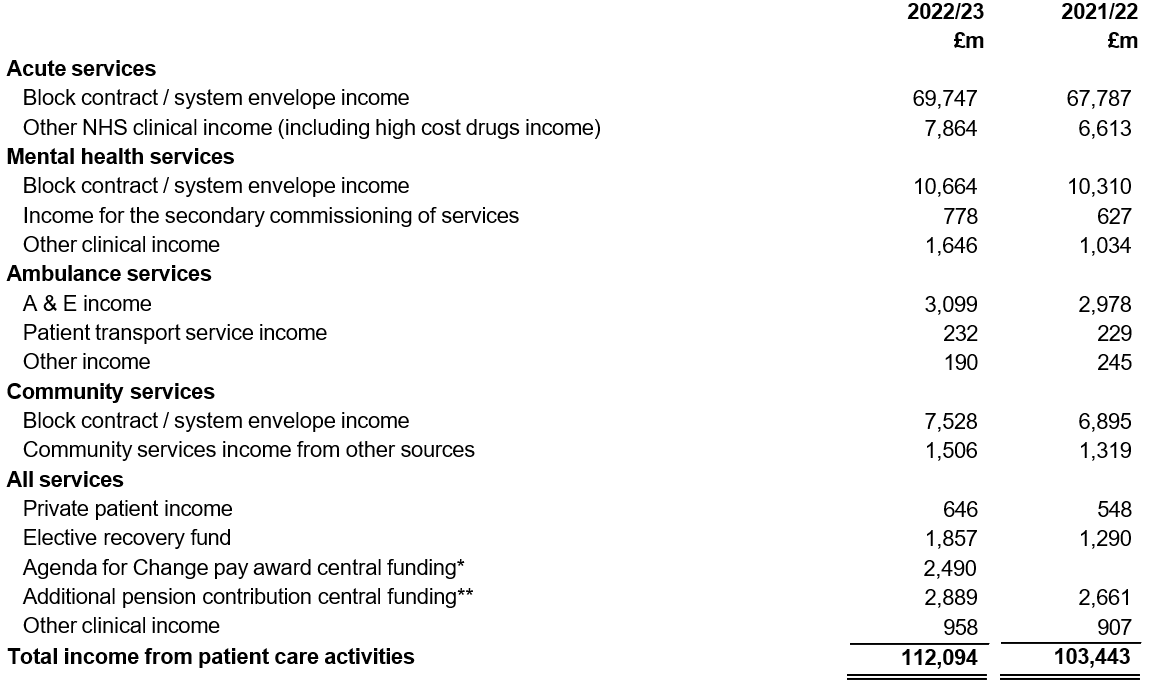
*In March 2023 the government announced an additional pay offer for 2022/23, in addition to the pay award earlier in the year. Additional funding was made available by NHS England for implementing this pay offer for 2022/23 and the income and expenditure has been included in these accounts as guided by the Department of Health and Social Care. In May 2023 the government confirmed this offer would be implemented as a further pay award in respect of 2022/23 based on individuals in employment at 31 March 2023.
** The employer contribution rate for NHS pensions increased from 14.3% to 20.6% (excluding administration charge) from 1 April 2019. NHS providers have continued to pay over contributions at the former rate with the additional amount being paid over by NHS England on providers’ behalf. The full cost and related funding have been recognised in these accounts.
Note 3.2 Income from patient care activities (by source)
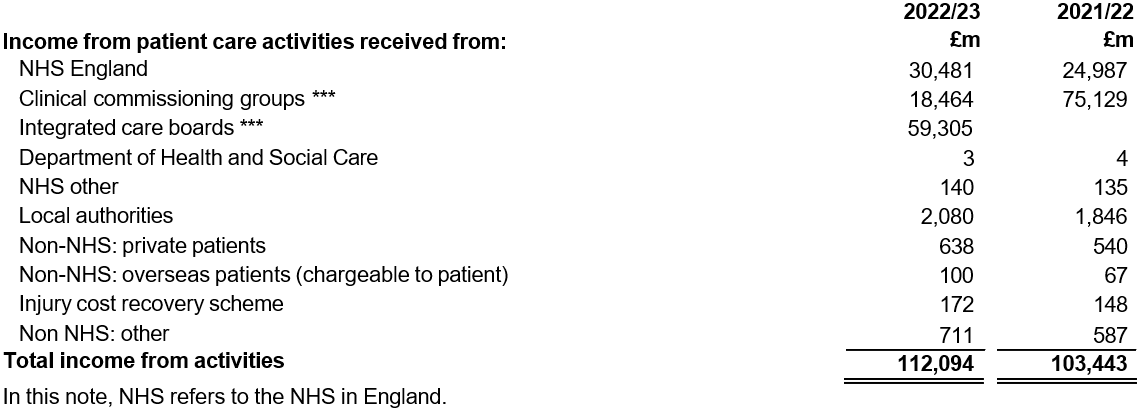
*** On 1 July 2022, 42 integrated care boards (ICBs) were established under the Health and Care Act 2022. Functions previously performed by the 106 clinical commissioning groups (CCGs) transferred and the CCGs were dissolved.
Further information on ICBs can be found at: NHS England » Integrated care in your area
Note 3.3 Overseas visitors (relating to patients charged directly by the NHS provider)
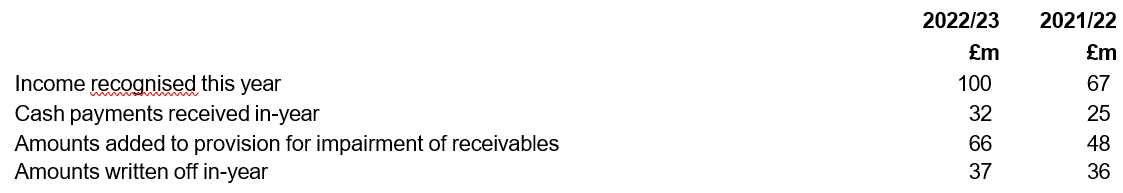
Note 4 Other operating income
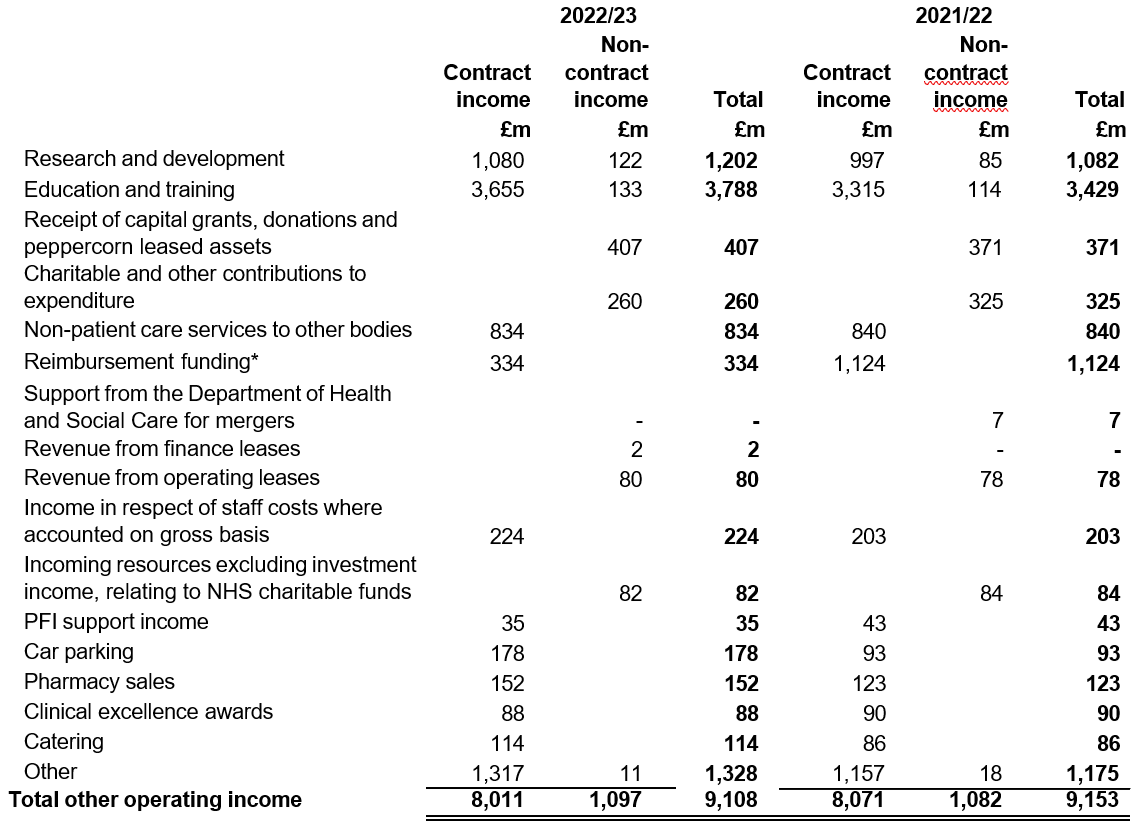
* Additional costs of delivering COVID testing laboratories and vaccinations were reimbursed to NHS providers by NHS England. From August 2022, vaccination funding was transferred into baseline contracts with integrated care boards rather than being reimbursed centrally.
Note 5 Operating leases – NHS providers as lessors
This note discloses income generated in operating lease agreements where an NHS provider is the lessor.
NHS providers applied IFRS 16 Leases to account for lease arrangements from 1 April 2022 without restatement of comparatives. Comparative disclosures in this note are presented on an IAS 17 basis. This includes a different maturity analysis of future minimum lease receipts under IAS 17 compared to IFRS 16.
Note 5.1 Operating leases income
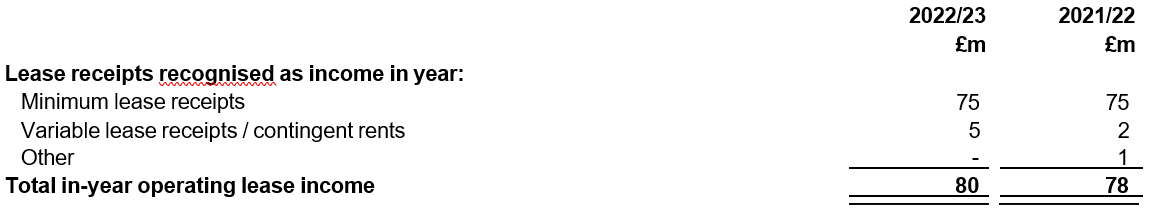
Note 5.2 Future lease receipts
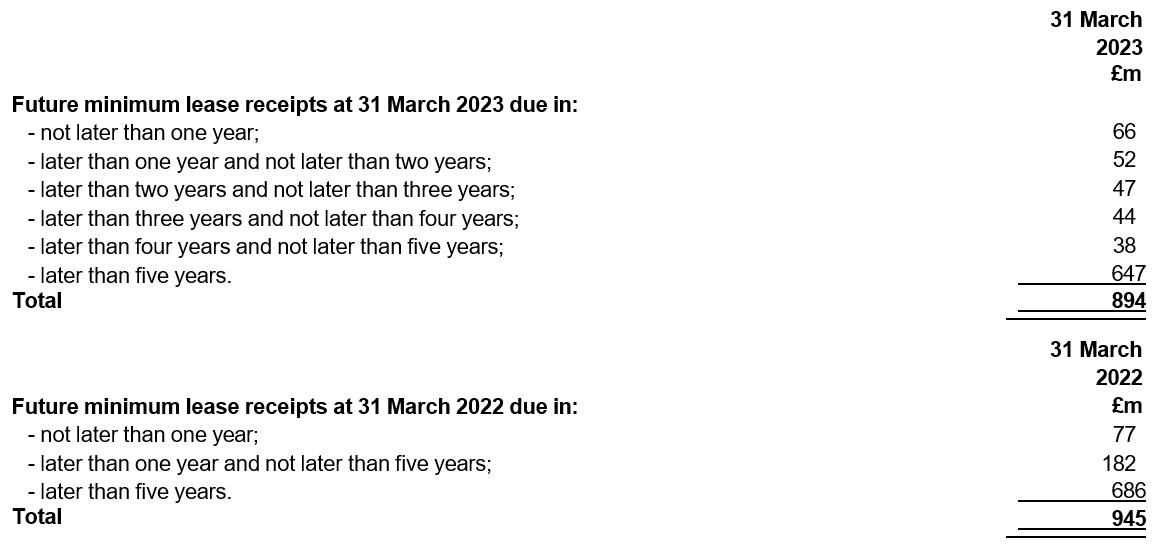
Note 6.1 Operating expenses
|
Note 6.1 Operating expenses |
| |
|
|
2022/23 |
2021/22 |
|
|
£m |
£m |
|
Purchase of healthcare from NHS and DHSC bodies |
13 |
11 |
|
Purchase of healthcare from non-NHS and non-DHSC bodies |
3,123 |
2,693 |
|
Purchase of social care |
207 |
200 |
|
Employee expenses – staff (including executive directors)* |
78,800 |
70,846 |
|
Non-executive directors |
34 |
34 |
|
Supplies and services – clinical |
8,356 |
8,164 |
|
Supplies and services – general |
1,842 |
1,709 |
|
Drug costs |
9,931 |
9,172 |
|
Inventories written down |
19 |
18 |
|
Consultancy costs |
196 |
260 |
|
Establishment |
1,243 |
1,205 |
|
Premises |
4,635 |
4,466 |
|
Transport (including patient travel) |
907 |
849 |
|
Depreciation on property, plant and equipment and right of use assets |
3,635 |
2,706 |
|
Amortisation on intangible assets |
389 |
339 |
|
Net Impairments |
1,054 |
700 |
|
Movement in credit loss allowance: contract receivables/assets |
96 |
78 |
Movement in credit loss allowance: all other receivables and financial assets |
2 |
– |
|
Increase in other provisions |
(45) |
126 |
|
Change in provisions discount rate(s) |
(86) 14 | |
|
Fees payable to the external auditor** |
| |
|
audit services- statutory audit |
32 |
26 |
|
other auditor remuneration (external auditor only) |
1 |
1 |
|
Internal audit costs, including local counter fraud services |
21 |
21 |
|
Clinical negligence |
2,435 |
2,456 |
|
Legal fees |
112 |
112 |
|
Insurance |
100 |
97 |
|
Research and development |
804 |
749 |
|
Education and training |
905 |
797 |
|
Expenditure on short term leases (current year only) |
94 | |
|
Expenditure on low value leases (current year only) |
25 | |
|
Variable lease payments not included in the liability (current year only) |
31 | |
|
Operating leases expenditure (comparative only) |
880 | |
|
Early retirements |
1 |
1 |
|
Redundancy |
17 |
15 |
|
Charges to operating expenditure for on-SoFP IFRIC 12 schemes (e.g. PFI / LIFT) *** |
1,131 |
1,059 |
|
Charges to operating expenditure for off-SoFP PFI / LIFT schemes |
1 |
4 |
Car parking and security |
78 |
82 |
|
Hospitality |
6 |
6 |
Losses, ex gratia and special payments |
19 |
32 |
|
Grossing up consortium arrangements |
17 |
13 |
|
Other services, eg external payroll |
84 |
87 |
|
Other |
678 |
840 |
|
NHS charitable funds: Other resources expended |
53 |
44 |
|
Total |
120,996 110,912 | |
* Staff costs here and in note 7.1 differ as note 7.1 also includes redundancy and early retirements costs and the costs of staff involved in research and development, education and training and internal audit services.
** These are the audit fees disclosed by NHS providers and do not include the audit fee payable to the National Audit Office in respect of these consolidated accounts. This fee is £250,000 (2021/22: £130,000).
*** This line does not contain all the charges relating to PFI and similar schemes in these accounts. An analysis of payments made to PFI operators can be found in note 24.3.
Note 6.2 Other auditors’ remuneration
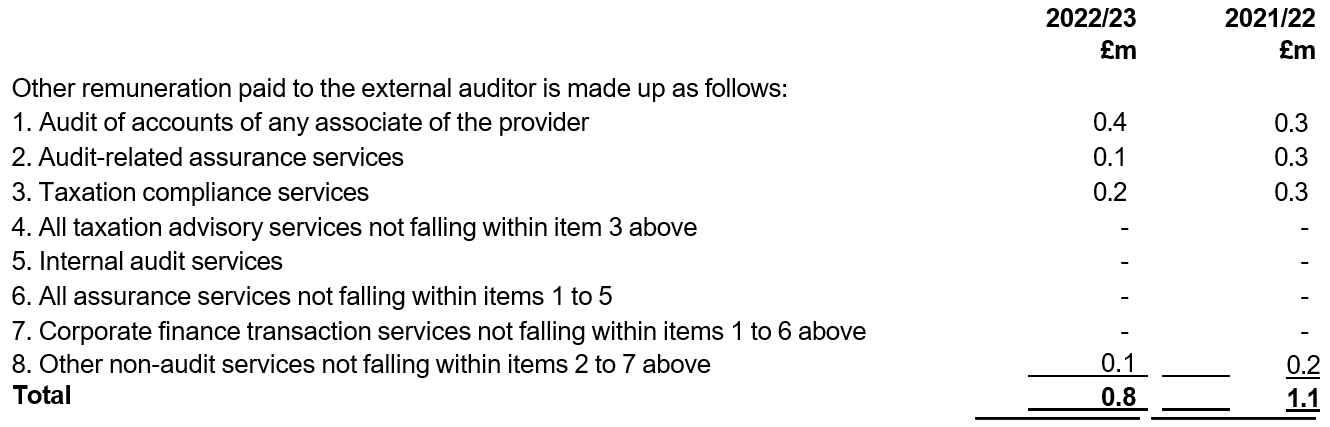
Note 7.1 Employee benefits
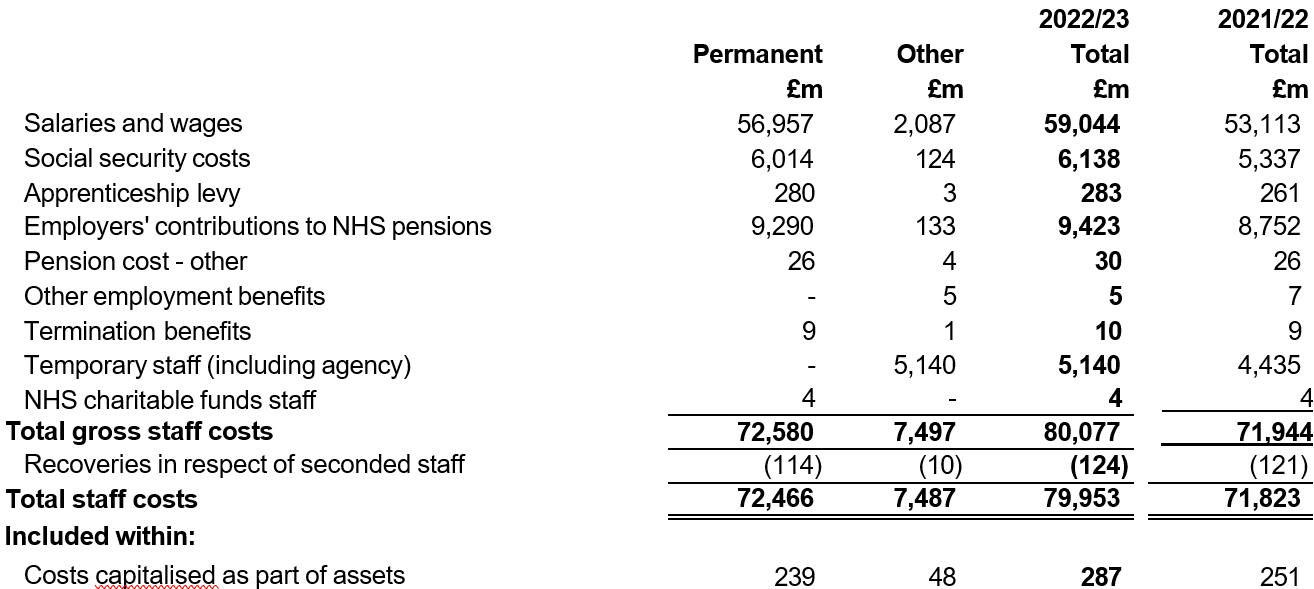
Staff costs here and in note 6.1 differ as note 7.1 also includes redundancy and early retirements costs and the costs of staff involved in research and development, education and training and internal audit services.
Individual NHS providers’ accounts and annual reports contain disclosure of senior manager remuneration, fair pay ratio information and off-payroll engagements as required by the HM Treasury FReM.
Note 7.2 Average number of employees (WTE basis)
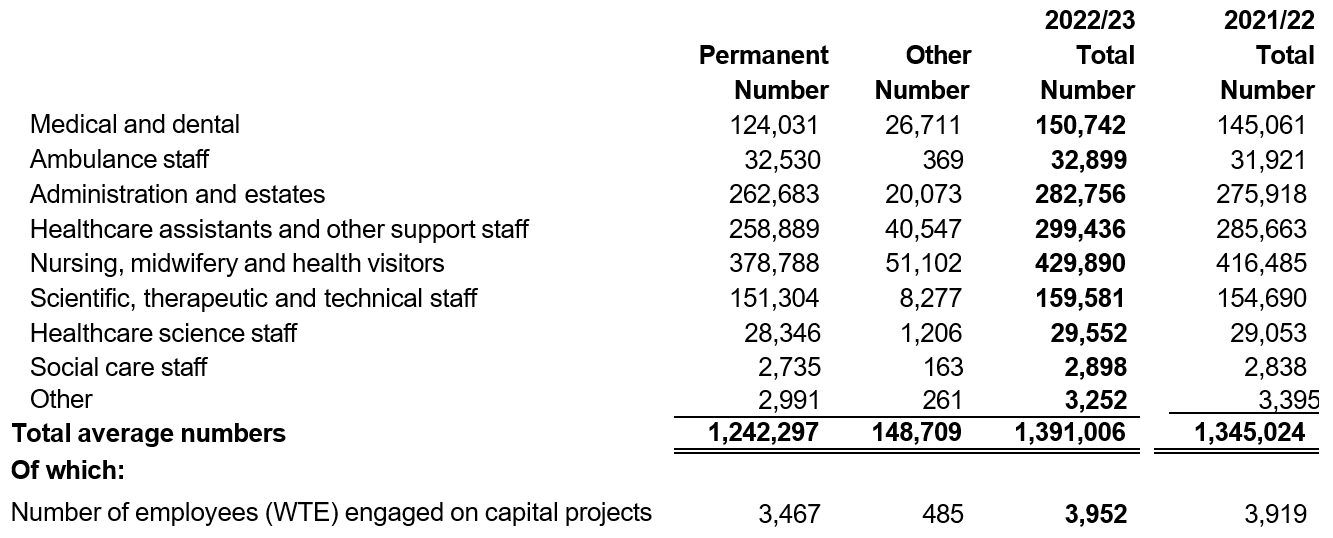
Note 7.3 Early retirements due to ill-health
During 2022/23 there were 858 early retirements on the grounds of ill-health (2021/22: 711). The estimated additional pension liability (calculated on an average basis and borne by the NHS Pension Scheme) is £61 million (2021/22: £48 million).
Note 7.4 Reporting of compensation schemes – exit packages
Redundancy and other departure costs have been paid in accordance with the provisions of the NHS terms and conditions of service. Exit costs are accounted for in full in the year of departure. Ill-health retirement costs are met by the pension scheme and are not included in the table.
Further disclosure of exit packages paid to senior managers can be found in the remuneration reports of individual NHS providers. Note 7.5 provides further analysis of the ‘other departures’ disclosed below.
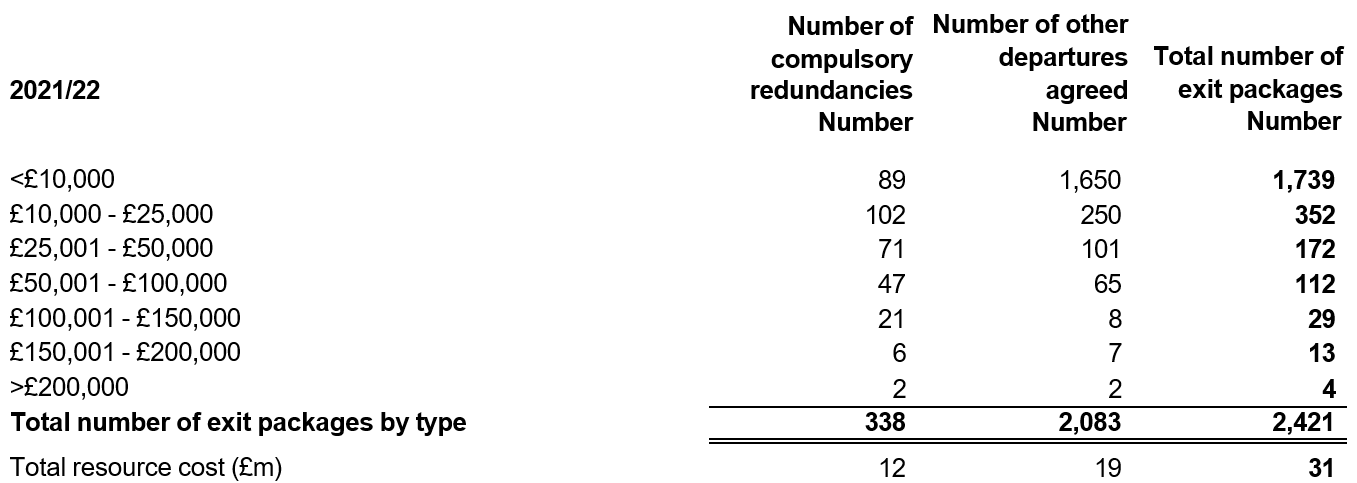
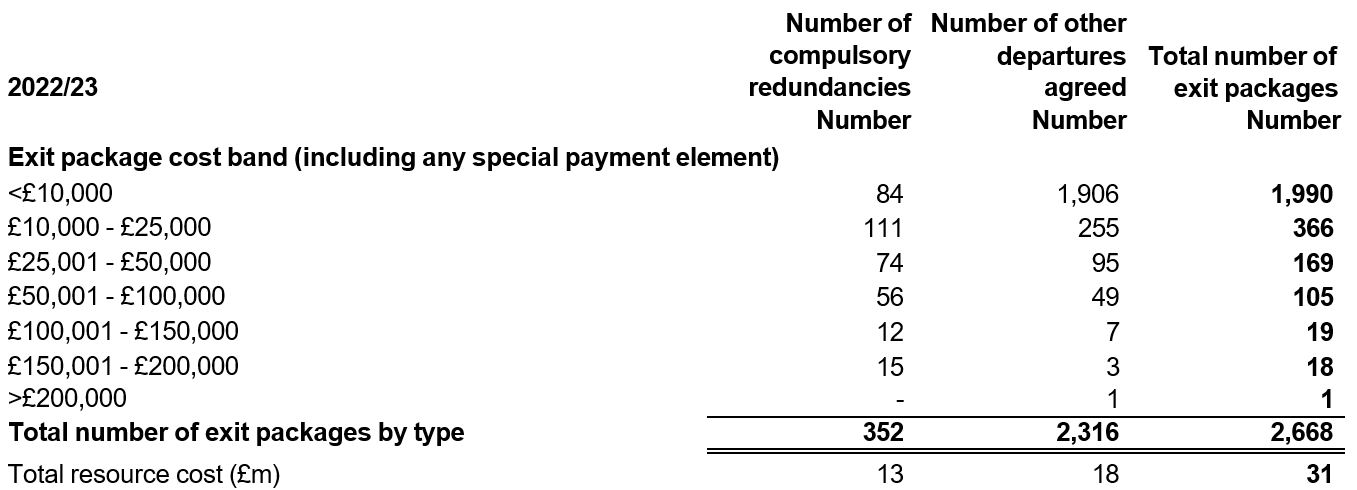
Note 7.5 Exit packages: other (non-compulsory) departure payments
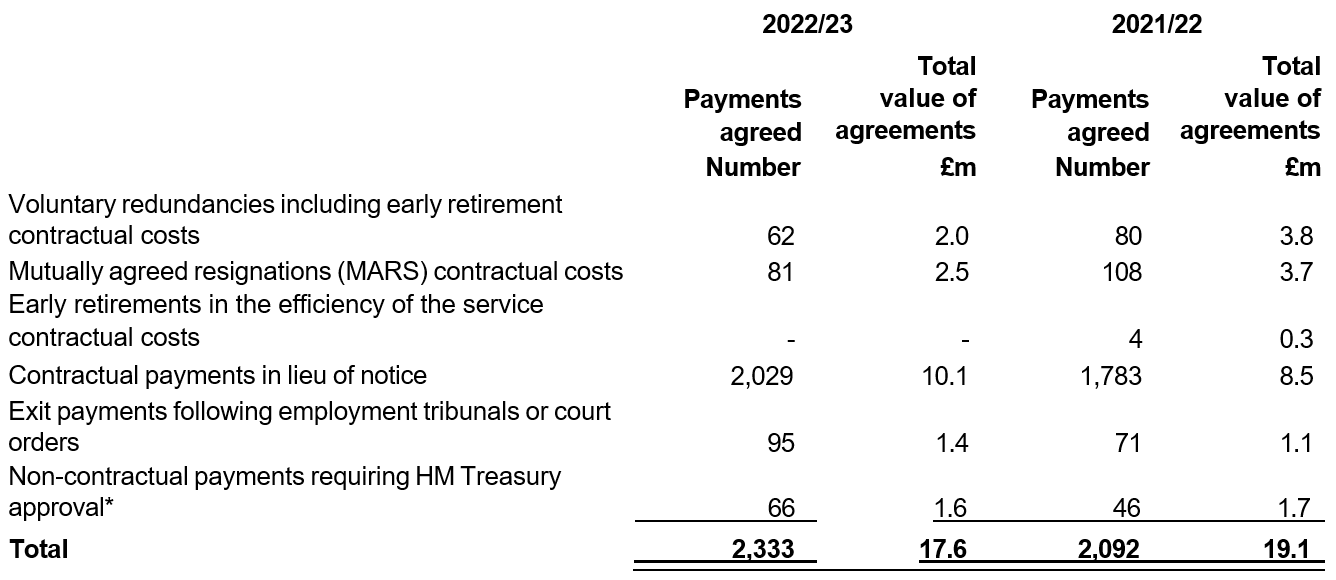
* Includes any non-contractual severance payment made following the judicial mediation, and amounts relating to non-contractual payments in lieu of notice.
In 2022/23 there were 2 non-contractual payments requiring HM Treasury approval (totalling £0.5 million) that were in excess of the individuals’ salary (2021/22: 3 payments totalling £0.4 million).
As a single exit package can be made up of several components, each of which will be counted separately in this note, the total number in note 7.5 does not match the total numbers in note 7.4 which is the number of individuals.
Exit packages disclosed in this note differ from the redundancy figure included within note 6.1. The redundancy figure in note 6.1 relates to additional costs which are not exit packages payable directly to the employee.
Note 8 Pension costs
All NHS providers participate in the NHS Pension Scheme. This is a statutory, defined benefit scheme, the regulations of which are laid down in the NHS Pension Scheme Regulations 1995 (SI 1995 No. 300). NHS providers pay contributions at rates specified from time to time by the Secretary of State, as advised by the Government Actuary and with the consent of HM Treasury.
For 2022/23, the employer contribution rate was 20.6% (2021/22: 20.6%). It is not possible for the NHS provider sector to identify its share of the underlying scheme assets and liabilities. Therefore, the scheme is accounted for as a defined contribution scheme in these accounts.
Employer pension contributions are charged to operating expenses as and when they become due.
As set out in accounting policy 1.4, some NHS providers also have employees who are members of other pension schemes. Membership of these individual schemes is not material to the consolidated NHS provider accounts.
Note 9 Impairment of non-current assets
Impairments are either charged to operating expenditure or the revaluation reserve. More detail is provided in accounting policy 1.7 and 1.8. Impairments reduce the value of assets. The note below provides detail about the reasons for impairments.
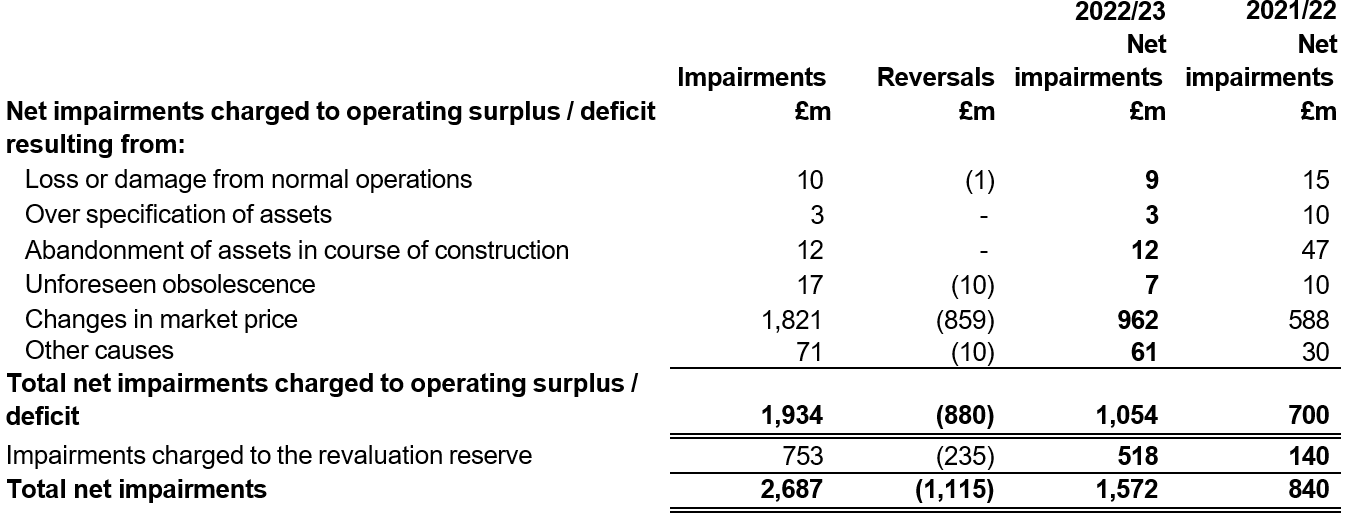
Net impairments taken to operating surplus/deficit relate to property, plant and equipment (£839 million, 2021/22: (£674 million), intangible assets (£22 million, 2021/22: £26 million), right of use assets (£192 million) and assets held for sale (£1 million, 2021/22: nil). Impairments charged to the revaluation reserve relate to property, plant and equipment (£509 million, 2021/22: £140 million) and right of use assets (£9 million).
In addition there are revaluation surpluses taken to the revaluation reserve of £2,431 million (2021/22: £1,534 million), as can be seen in the Statement of Changes in Equity.
Note 10 Finance expenditure
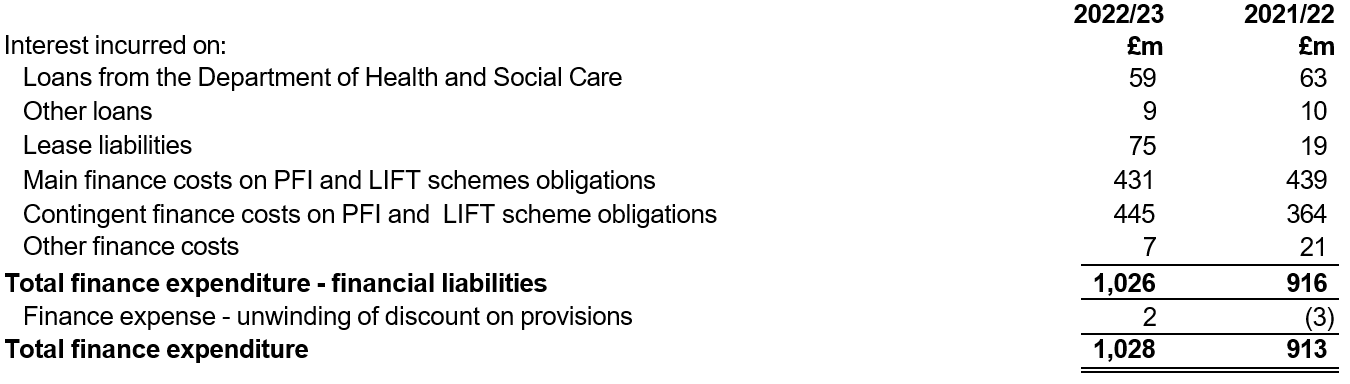
Note 11 Other gains and losses
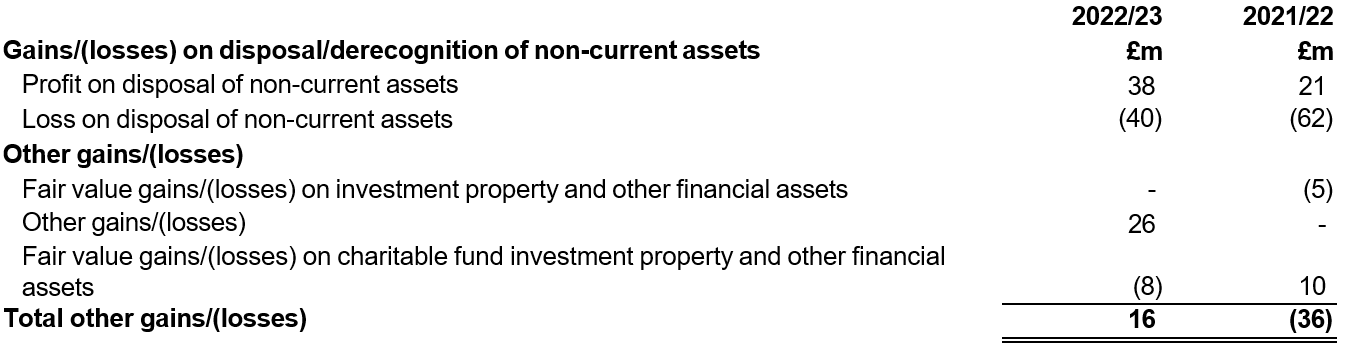
Note 12.1 Intangible assets – 2022/23
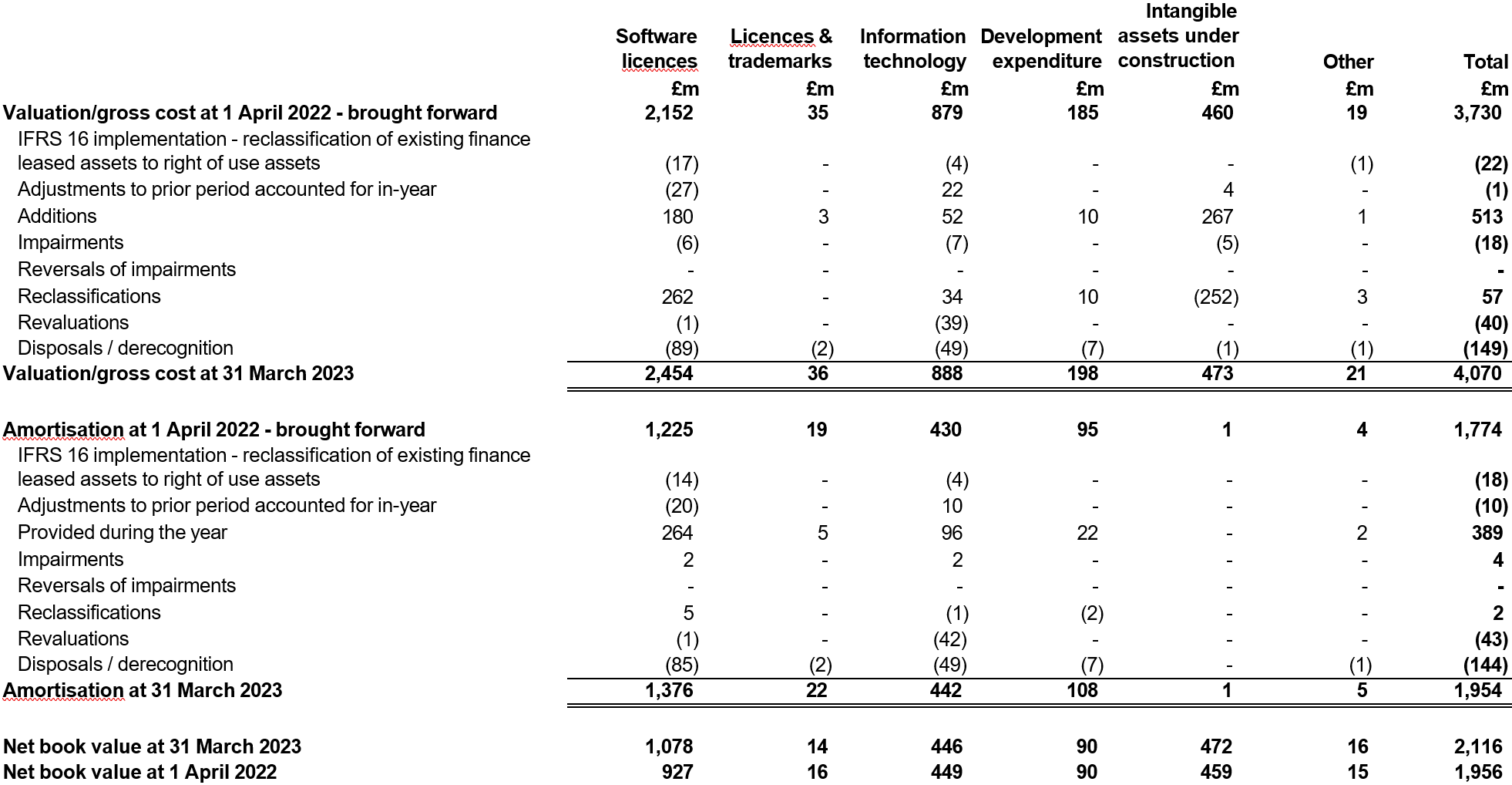
The total net impairment of £22 million shown in this note was charged to operating expenses.
Note 12.2 Intangible assets – 2021/22
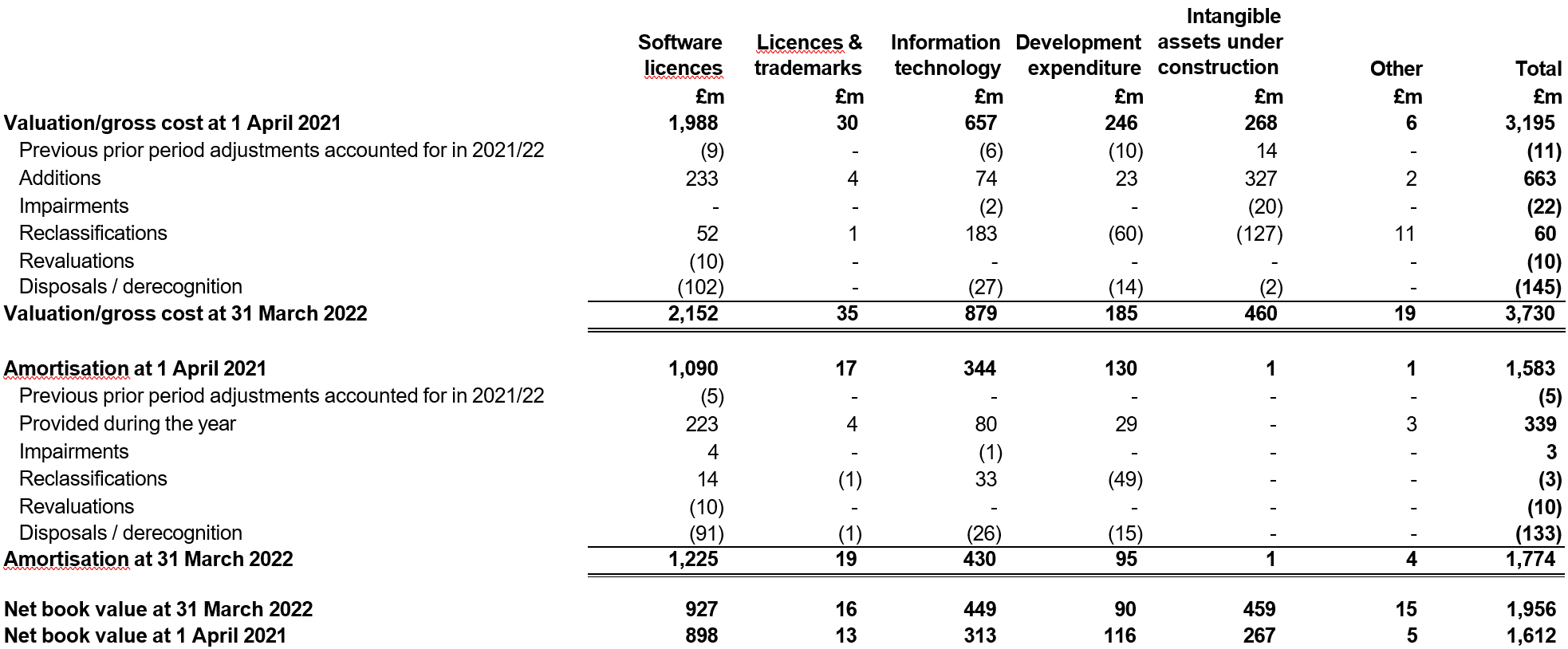
The total net impairment of £25 million shown in this note was charged to operating expenses.
Note 13.1 Property, plant and equipment – 2022/23
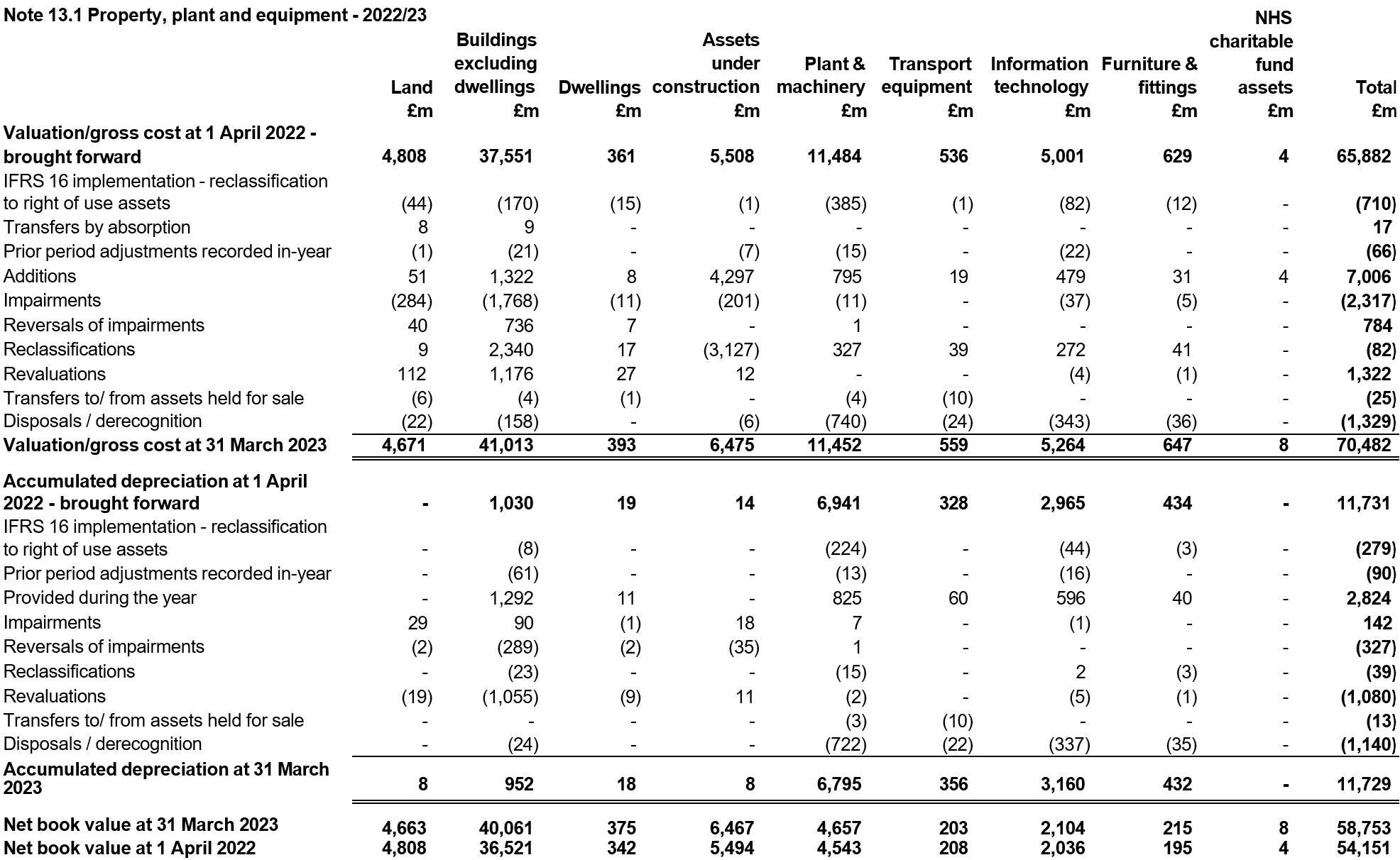
Details of donations received during the year including any restrictions or conditions imposed by the donor are disclosed in the accounts of individual NHS providers.
Of the total net impairments of £1,348 million shown in this note, £839 million was charged to operating expenses and £509 million to the revaluation reserve.
Note 1.25 explains some estimation uncertainties relating to property valuations and explores the impact of these on these consolidated accounts.
Note 13.2 Property, plant and equipment – 2021/22
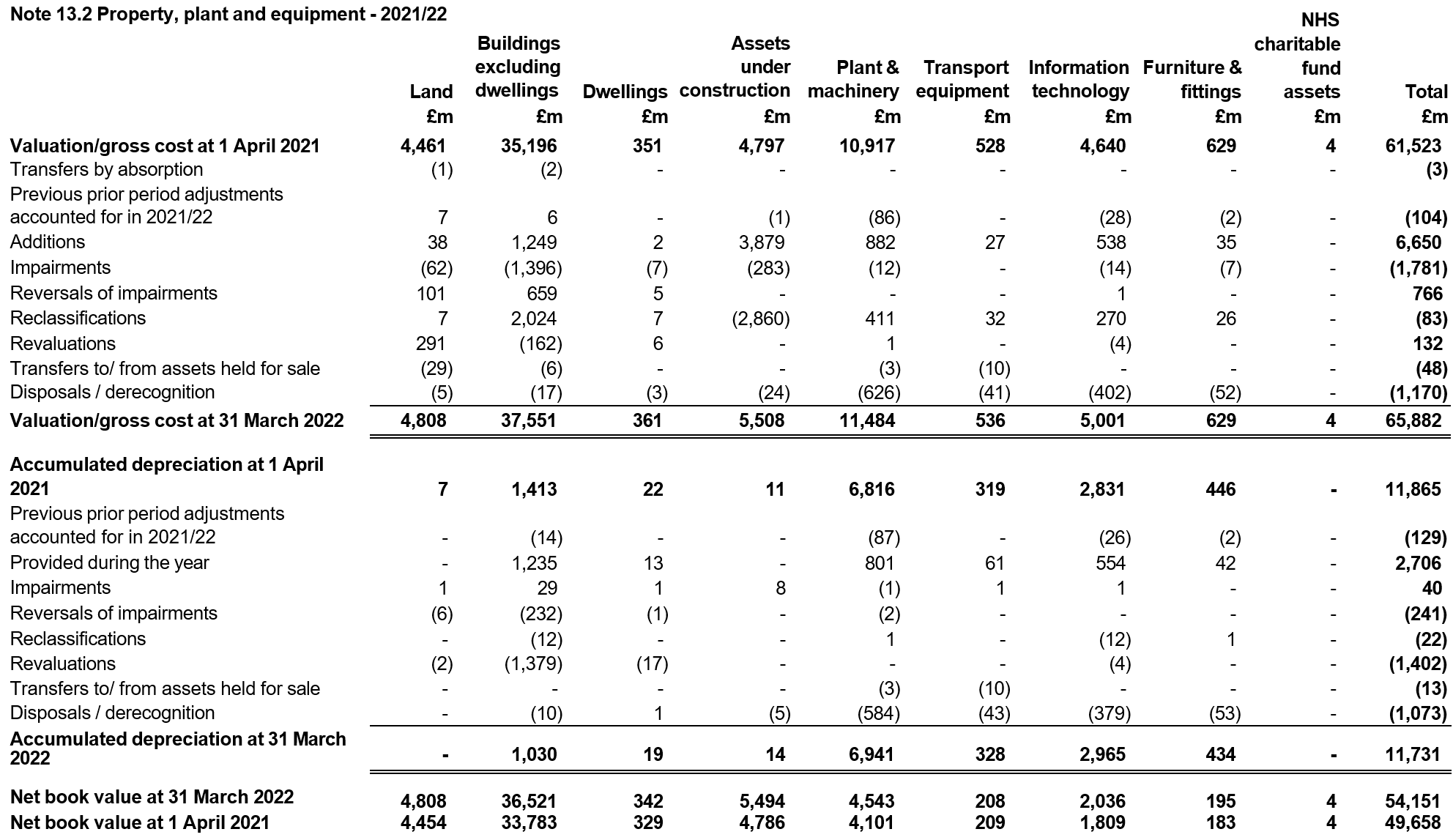
Details of donations received during the year including any restrictions or conditions imposed by the donor are disclosed in the accounts of individual NHS providers.
Of the total net impairments of £814 million shown in this note, £674 million was charged to operating expenses and £140 million to the revaluation reserve.
Note 13.3 Property, plant and equipment financing – 31 March 2023
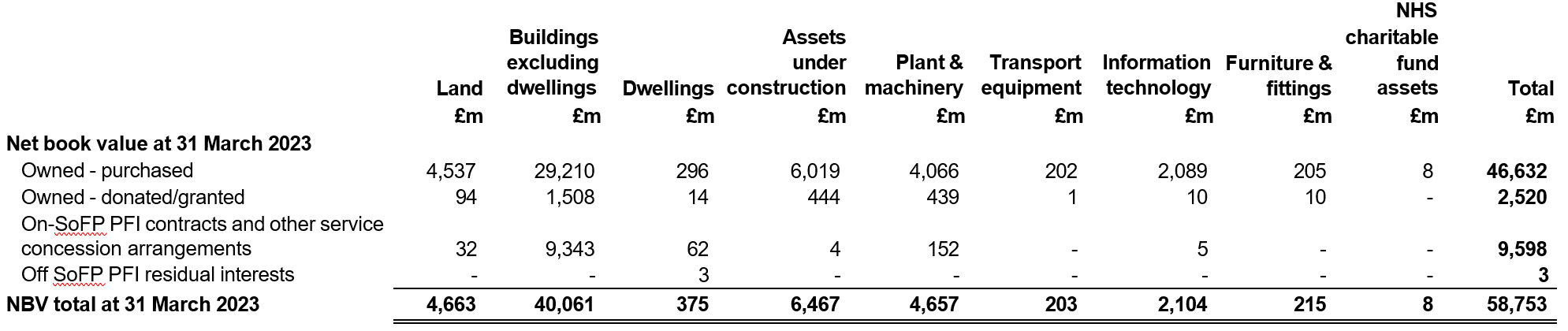
Note 13.4 Property, plant and equipment financing – 31 March 2022
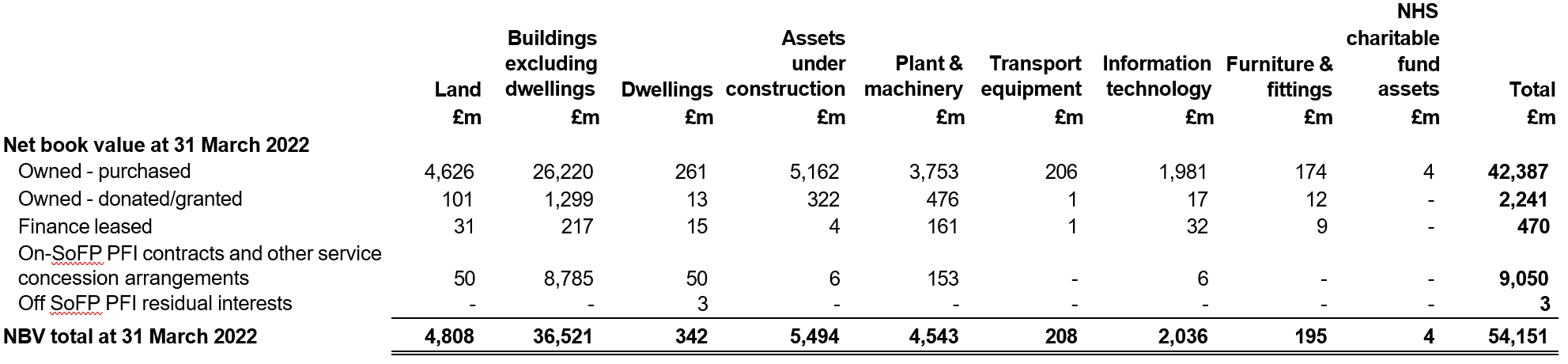
Note 13.5 Property plant and equipment assets subject to an operating lease (Trust as a lessor)
Property, plant and equipment disclosed in this note includes assets which are subject to operating leases where providers grant use of assets to third parties. It is not possible to accurately quantify the total value of such assets due to the impracticability in apportioning whole site valuations to partial assets subject to such leases. In the public sector, specialised assets are valued at the depreciated replacement cost of a modern equivalent asset required to replace the existing service potential of the trusts assets as set out in accounting policy 1.7.
Note 14 Leases – NHS providers as lessees
IFRS 16 Leases has been implemented from 1 April 2022 without restatement of comparatives. Comparative disclosures in this note are presented on an IAS 17 basis.
The majority of NHS provider lease arrangements are for the use of land and buildings ranging from integrated care units to office accommodation, and used by providers to deliver clinical and non-clinical services. Approximately 45% of lease arrangements based on the value of lease obligations at the reporting date are with NHS Property Services, a Government-owned property management company maintaining approximately 10% of the total NHS estate. The remaining leases are mainly with private landlords under commercial terms. Across providers there is a wide variety in lease terms on individual leases. More detail on the nature of lease arrangements including any restrictions or covenants imposed can be found in the accounts of individual NHS providers.
Note 14.1 Right of use assets – 2022/23 of which:
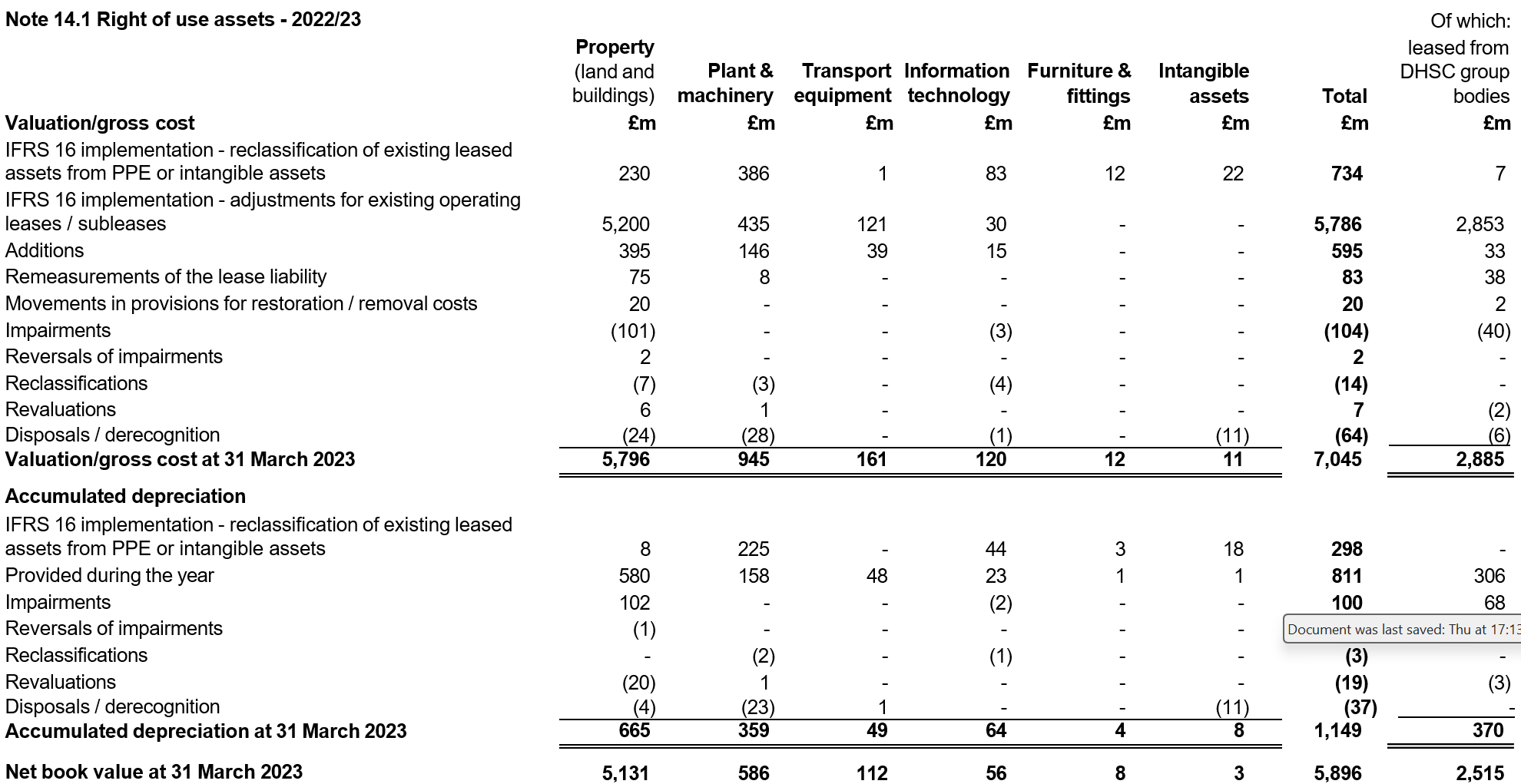
Of the total net impairments of £201 million shown in this note, £192 million was charged to operating expenses and £9 million to the revaluation reserve.
Note 14.2 Reconciliation of the carrying value of lease liabilities
Lease liabilities are included within borrowings in the statement of financial position. A breakdown of borrowings is disclosed in note 20.
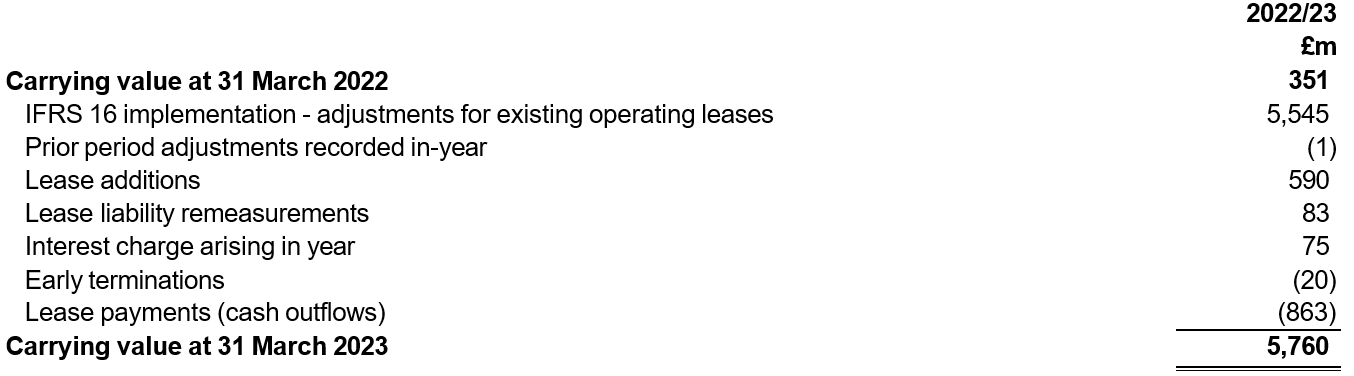
Lease payments for short term leases, leases of low value underlying assets and variable lease payments not dependent on an index or rate are recognised in operating expenditure and disclosed in Note 6.1.
Cash outflows in respect of leases recognised on-SoFP are disclosed in the reconciliation above.
Income generated from subleasing right of use assets in 2022/23 was £2 million and is included within revenue from operating leases in note 4.
Note 14.3 Maturity analysis of future lease payments at 31 March 2023
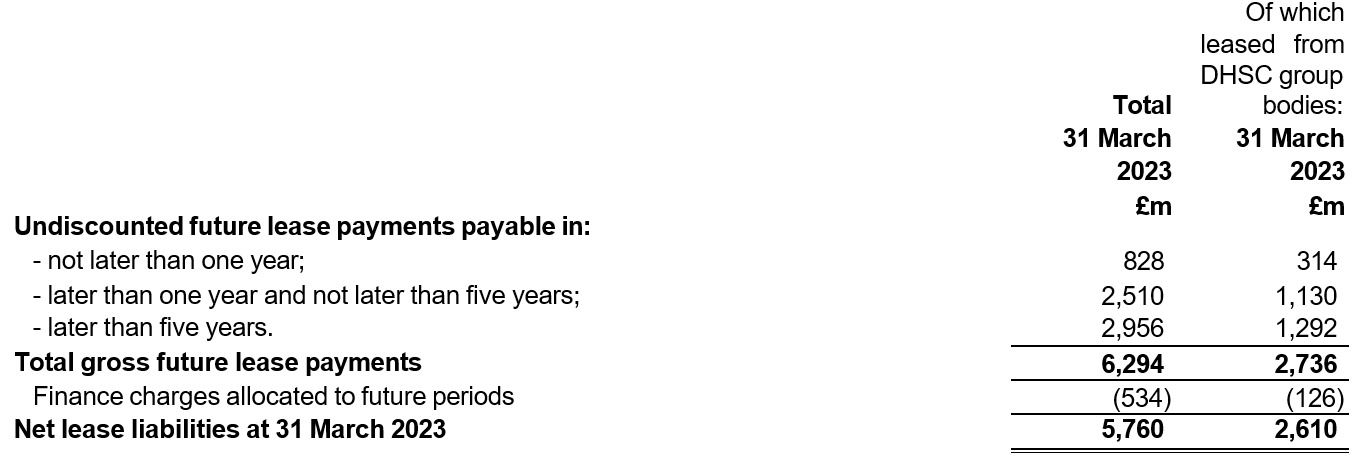
A description of how liquidity risk is managed in the provider sector to ensue these liabilities can be met as they fall due is disclosed in Note 26.6.
Note 14.4 Maturity analysis of finance lease liabilities at 31 March 2022 (IAS 17 basis)
The following table details the maturity of obligations under leases NHS providers previously determined to be finance leases under IAS 17 Leases at 31 March 2022.
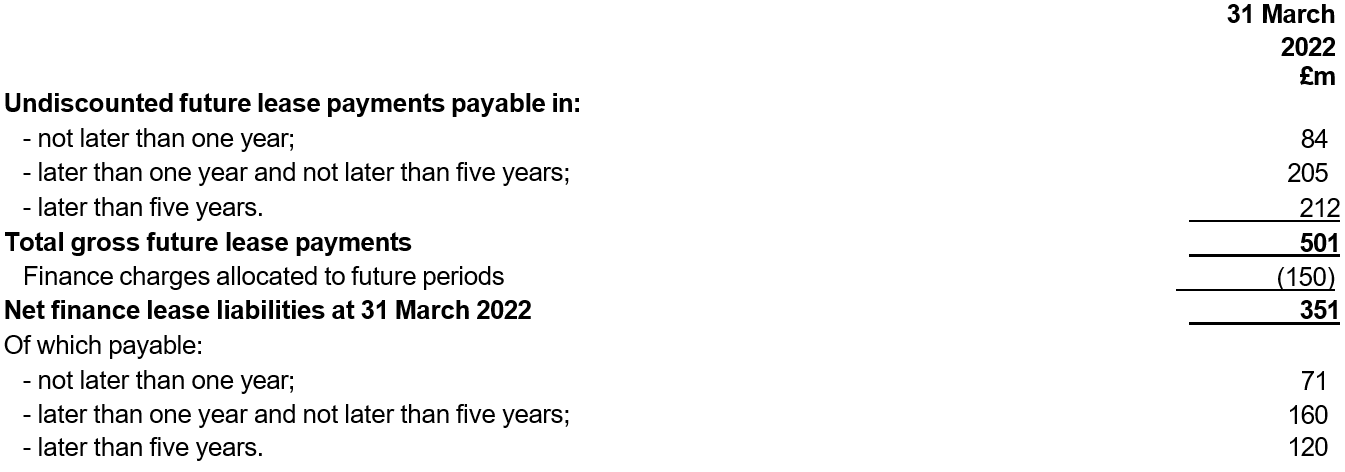
Note 14.5 Commitments in respect of operating leases at 31 March 2022 (IAS 17 basis)
This note discloses costs incurred in 2021/22 and commitments as at 31 March 2022 for leases NHS providers previously determined to be operating leases under IAS 17 Leases.
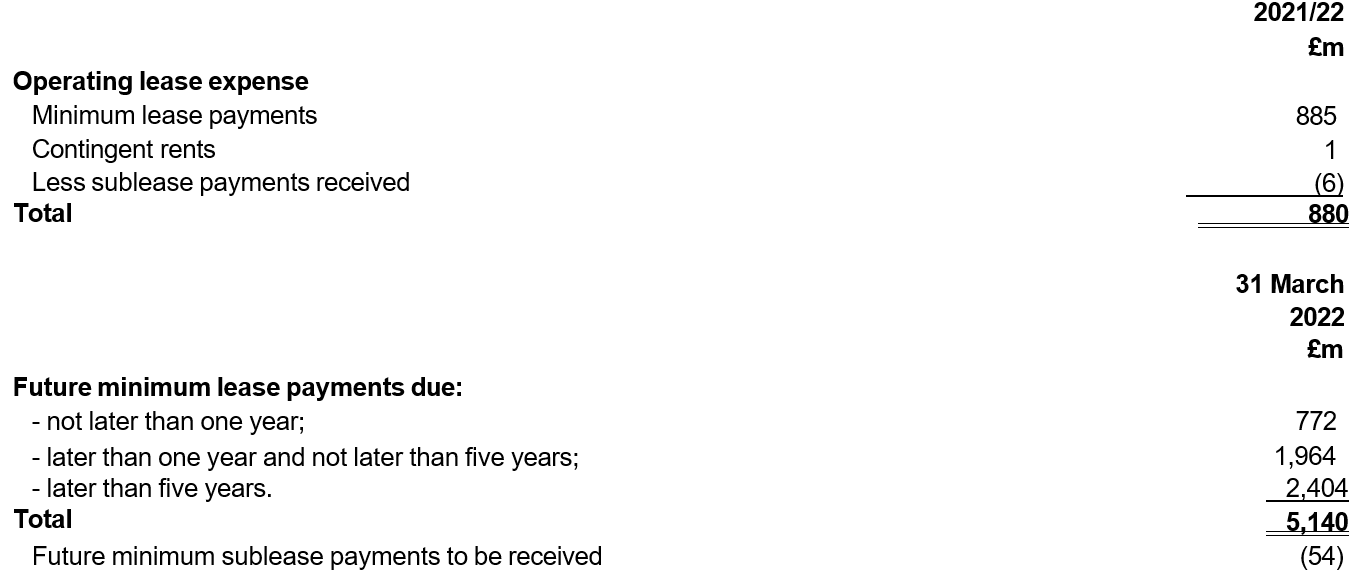
Note 14.6 Initial application of IFRS 16 on 1 April 2022
IFRS 16 Leases as adapted and interpreted for the public sector by HM Treasury has been applied to leases in these financial statements with an initial application date of 1 April 2022.
The standard has been applied using a modified retrospective approach without the restatement of comparatives. Practical expedients mandated for use by the NHS provider sector on initial application are detailed in the leases accounting policy in Note 1.10. In addition, providers may have locally elected to apply the practical expedients within paragraph C10 of IFRS 16 on a lease by lease basis.
Lease liabilities created for existing operating leases on 1 April 2022 were discounted using the weighted average incremental borrowing rate determined by HM Treasury as 0.95%.
Reconciliation of operating lease commitments as at 31 March 2022 to lease liabilities under IFRS 16 as at 1 April 2022
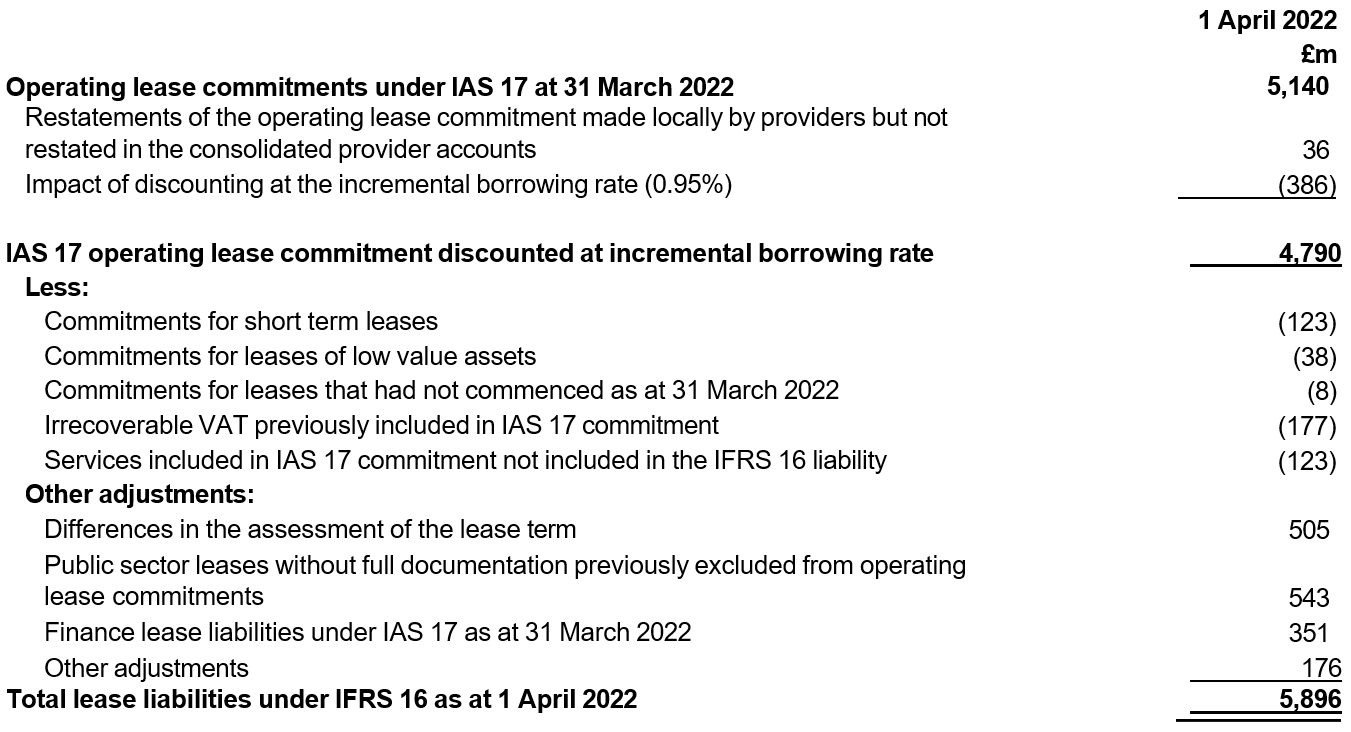
Note 15 Inventories

Inventories recognised in expenses for the year were £13,330 million (2021/22: £12,473 million). Write-downs of inventories recognised as expenses for the year were £19 million (2021/22: £18 million). These include utilisation of £194 million and write down of £3 million of personal protective equipment procured nationally by the Department of Health and Social Care and supplied free of charge to NHS providers in response to the coronavirus pandemic (2021/22: £315 million utilisation, £4 million write down).
Note 16.1 Receivables
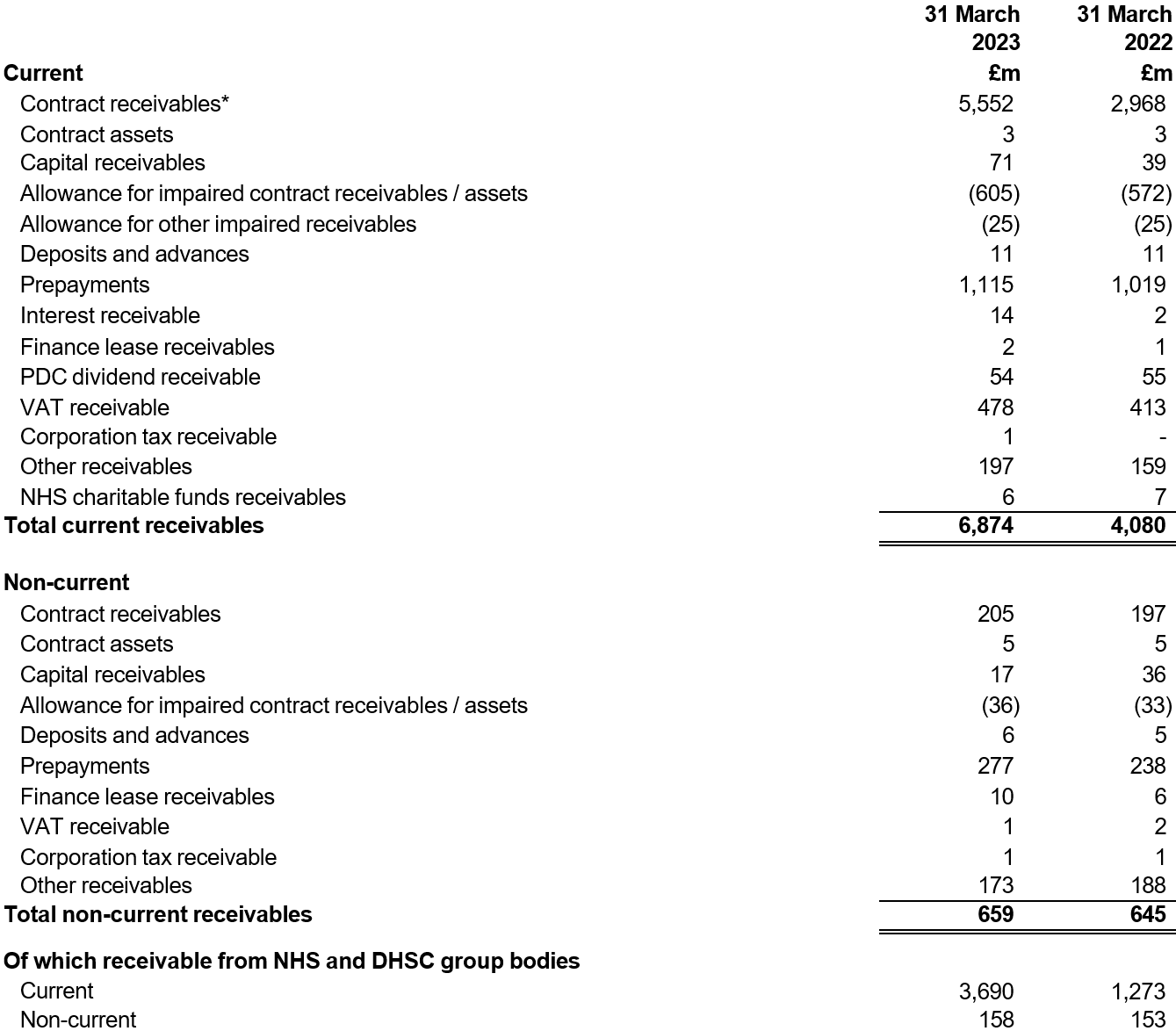
The terms ‘contract receivables’ and ‘contract assets’ are defined in accounting policy note 1.2.
*Current contract receivables at 31 March 2023 includes £2,490 million of accrued funding for the additional 2022/23 agenda for change pay award detailed in Note 3.1.
Note 16.2 Allowances for credit losses
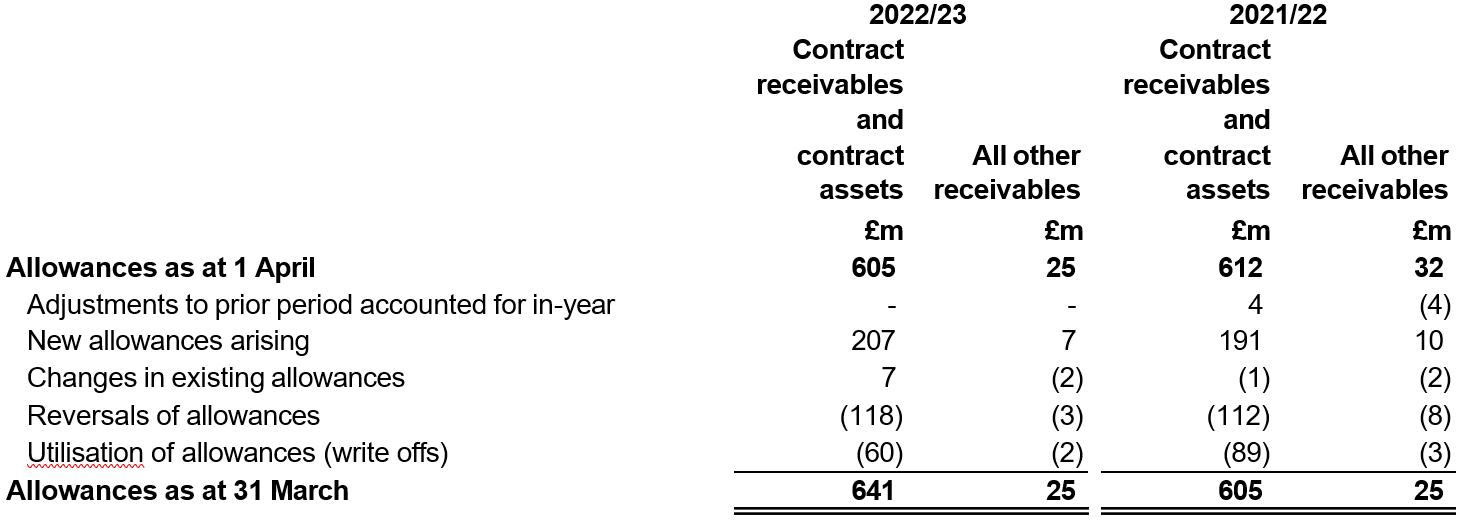
Note 17.1 Cash and cash equivalents movements
Cash and cash equivalents comprise cash at bank, in hand and cash equivalents. Cash equivalents are readily convertible investments of known value which are subject to an insignificant risk of change in value.
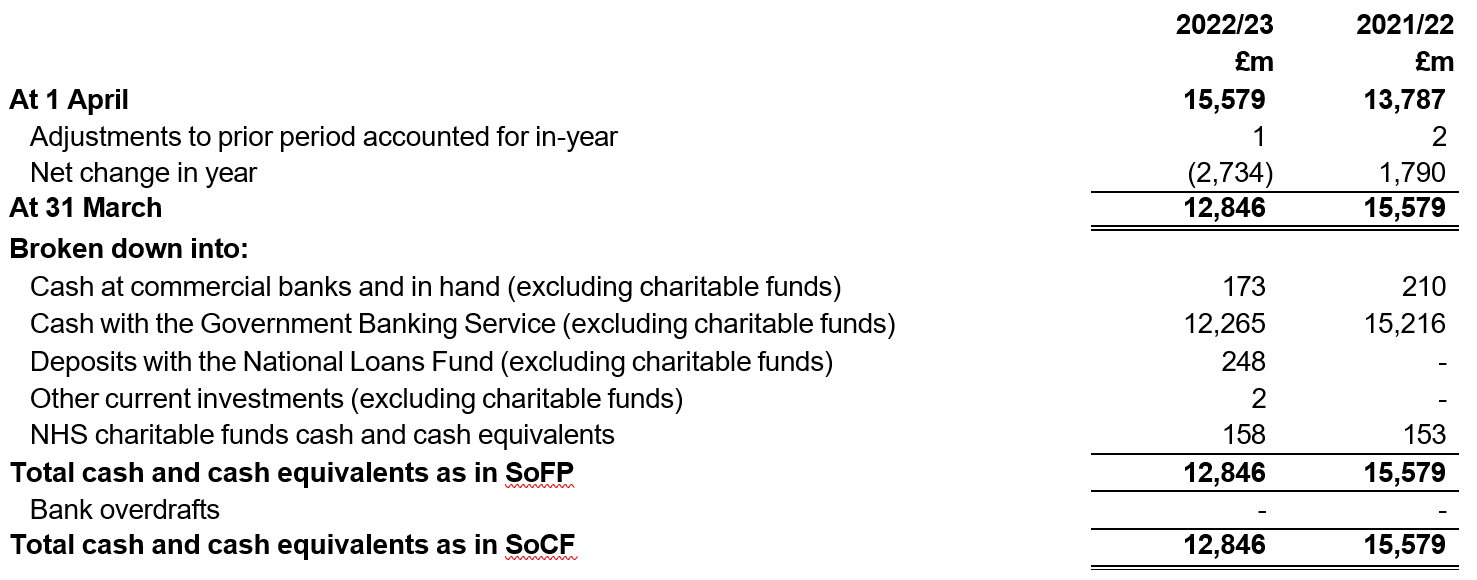
Note 17.2 Third party assets
The balance of third party assets, including patients’ money held within the NHS providers’ bank accounts at 31 March 2023 was £37 million (31 March 2022: £37 million). This has been excluded from the Consolidated Statement of Financial Position as it is not an asset of the NHS provider. Neither NHS providers nor Government more widely has a beneficial interest in these assets.
Note 18 Trade and other payables
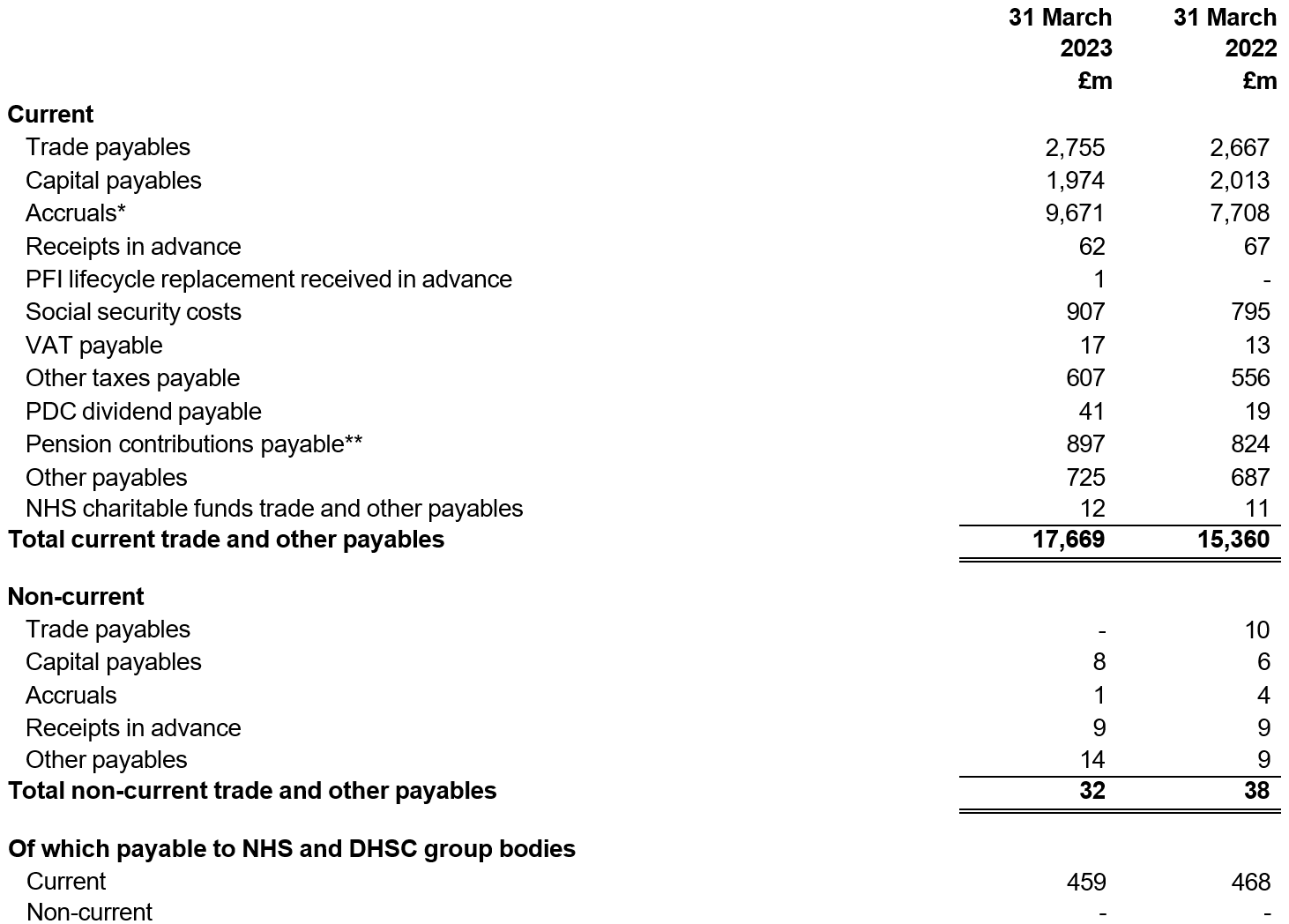
* At 31 March 2023, NHS providers accrued the costs of implementing the additional 2022/23 agenda for change pay award. As detailed in Note 3.1, providers also accrued £2,490 million of funding in respect of these costs.
** Contributions payable to the NHS pension scheme at the reporting date are now separately identified. Comparatives have been reanalysed accordingly removing the prior year contributions payable from other rows.
Note 19 Other liabilities
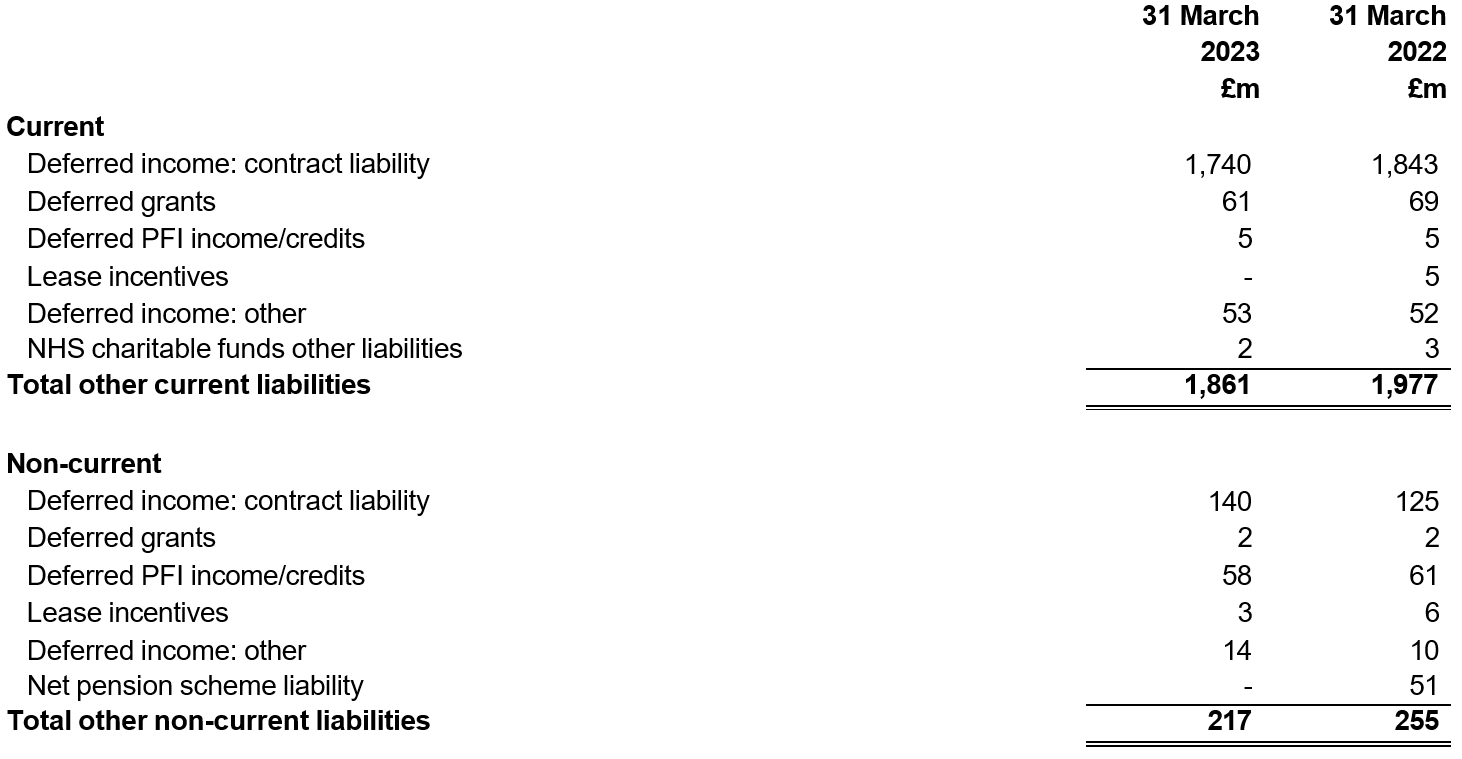
Note 20 Borrowings
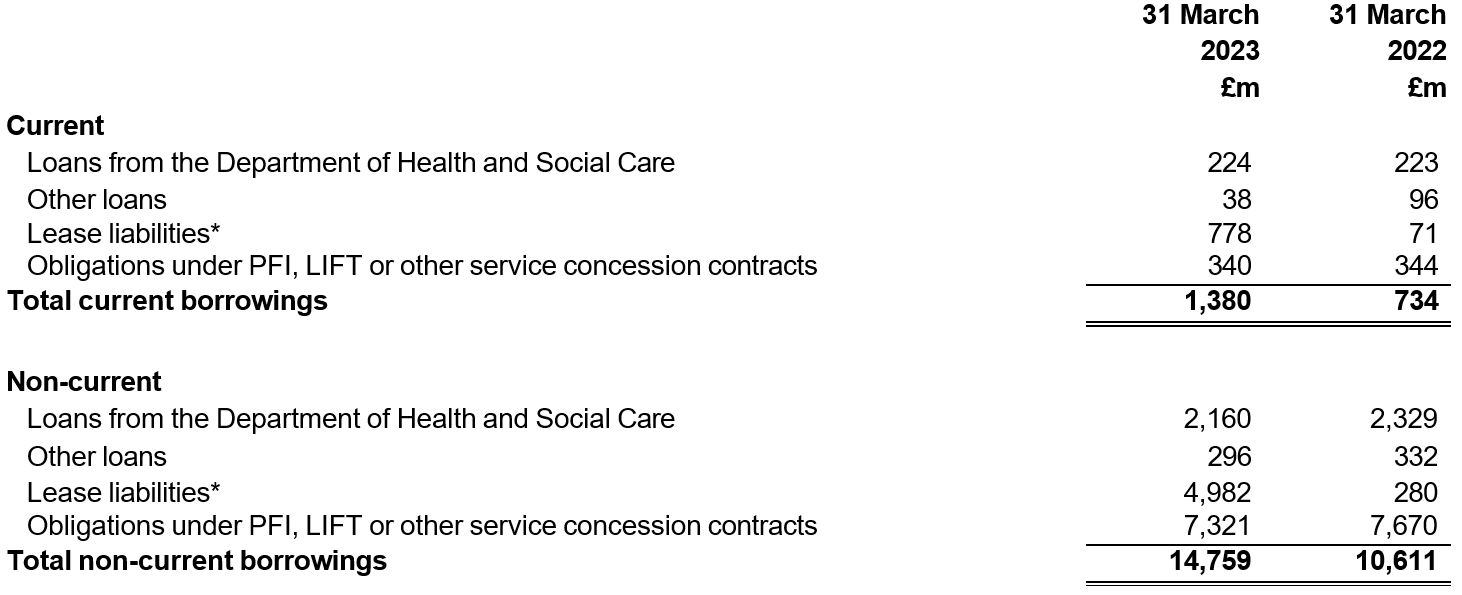
*NHS providers have applied IFRS 16 Leases to lease arrangements within these accounts from 1 April 2022 without restatement of comparatives. More information about leases and the impact of this change in accounting policy can be found in Note 14.
Note 20.1 Reconciliation of liabilities arising from financing activities – 2022/23
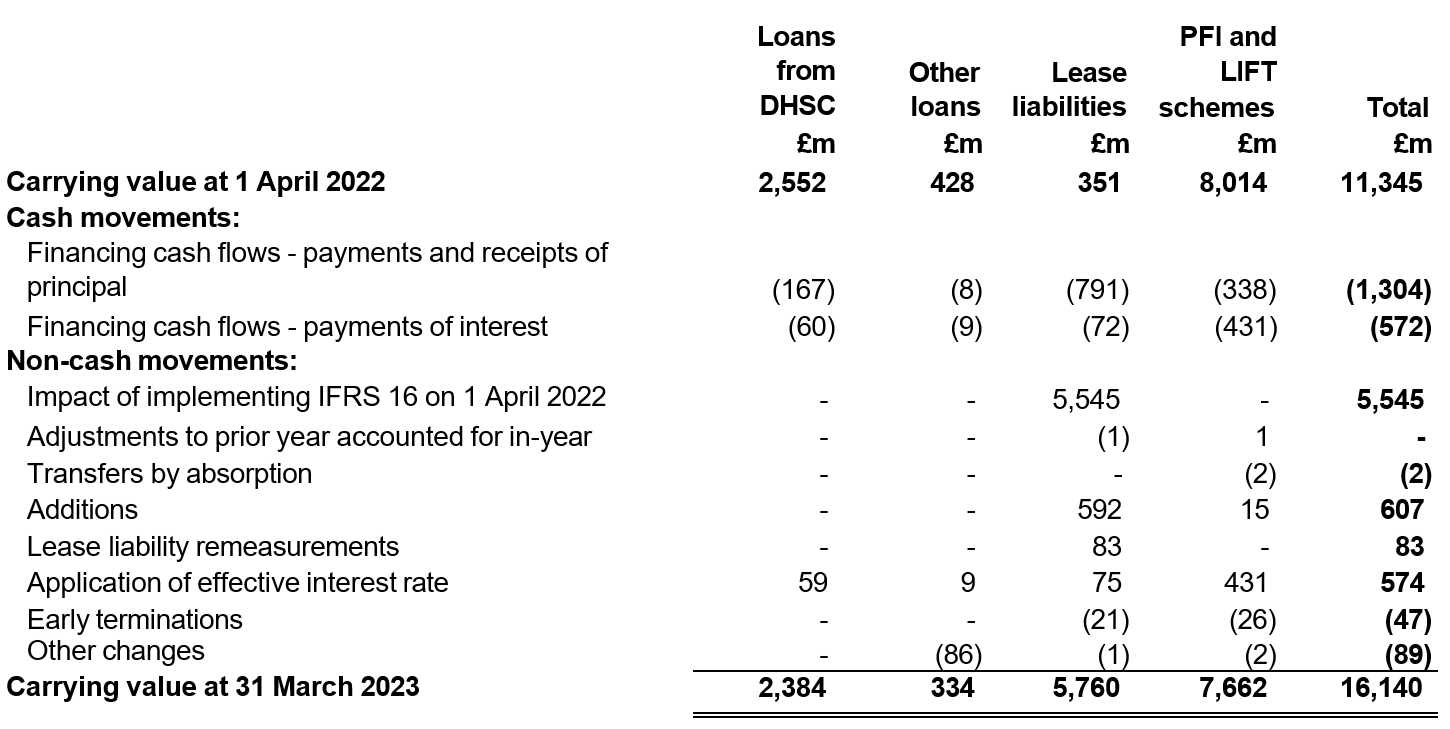
Note 20.2 Reconciliation of liabilities arising from financing activities – 2021/22
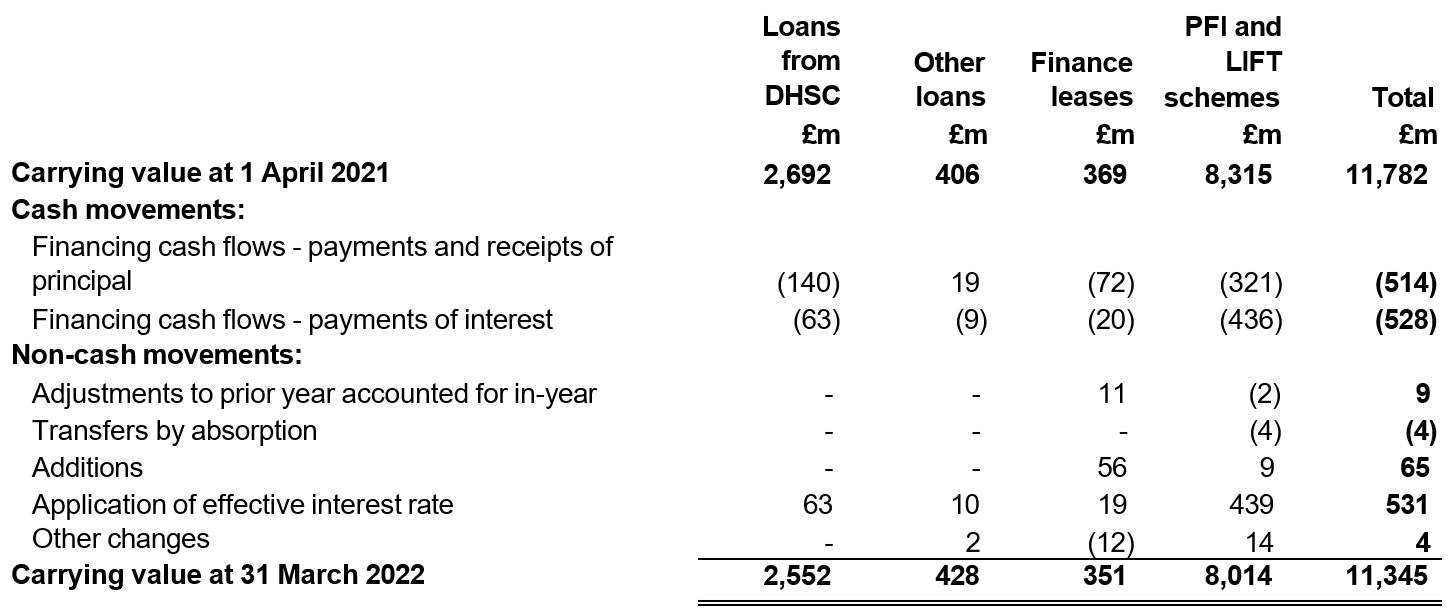
Note 21.1 Provisions for liabilities and charges
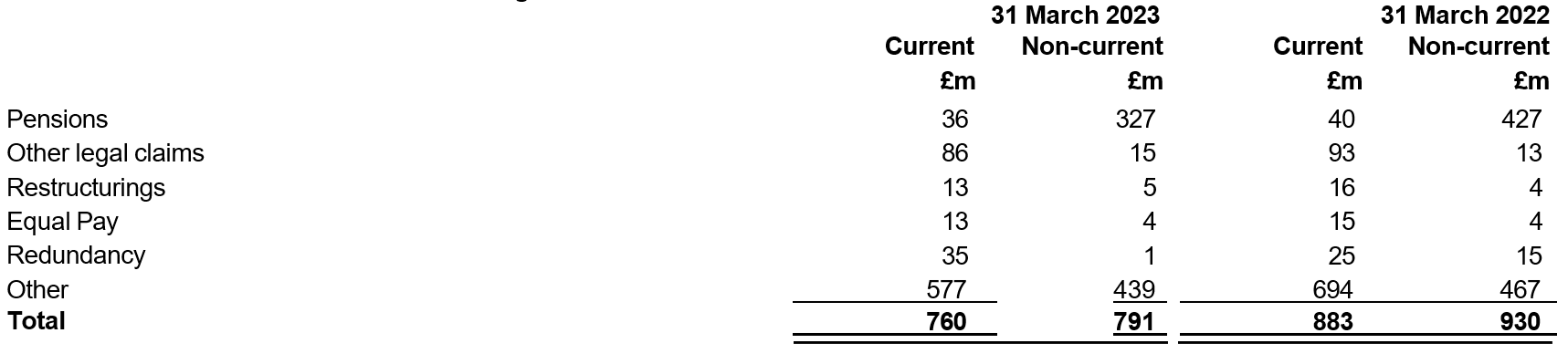
Note 21.2 Movement in provisions for liabilities and charges
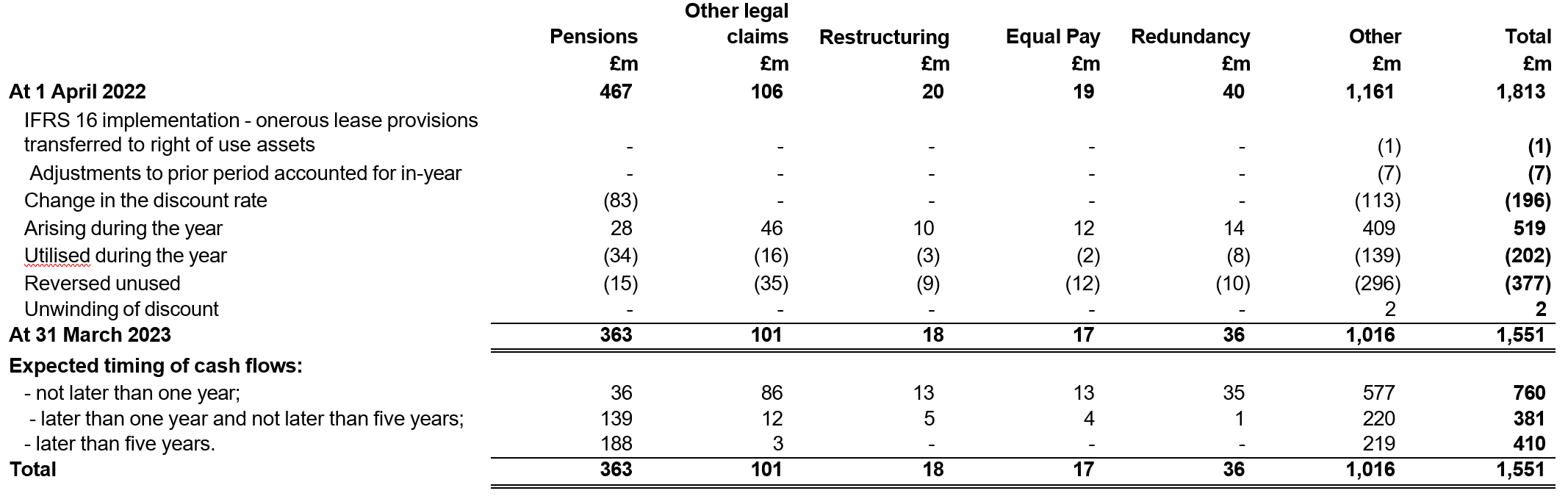
- Pension provisions relate to staff who have retired early from the NHS Pensions Scheme and are calculated in accordance with DHSC guidance.
- Other legal claims include personal legal claims that have been lodged against NHS providers with NHS Resolution but not yet agreed and therefore not included in provisions held by NHS Resolution.
- Equal pay provisions include provisions for unresolved claims relating to employment contracts.
- Redundancy and restructuring provisions are included by trusts who are undergoing change in their organisational structures.
- Included within other provisions are charges arising from the provision of services, the cost of PFI terminations, dilapidations associated with leases and other contract challenges.
Note 21.3 Clinical negligence liabilities
NHS Resolution manages clinical and some non-clinical claims on behalf of NHS providers. For this to occur, providers pay an annual premium to NHS Resolution, who then assumes responsibility for settling claims on providers’ behalf. This is called the Clinical Negligence Scheme for Trusts (CNST) which covers clinical negligence claims for incidents occurring on or after 1 April 1995. The Existing Liabilities Scheme (ELS) is centrally funded by DHSC and covers clinical negligence claims against NHS organisations for incidents occurring before 1 April 1995.
Under these schemes, most liabilities for clinical negligence are not included in providers’ statements of financial position. Instead they separately disclose the amounts relating to clinical negligence cases for their trust which are included in the provisions of NHS Resolution.
As at 31 March 2023, NHS Resolution held provisions for clinical negligence liabilities totalling £37,155 million for CNST (2021/22: £53,622 million) and £801 million for ELS (2021/22: £1,366 million) on behalf of NHS providers. NHS Resolution’s annual report and accounts provides more information on overall liabilities and explanations for movements between years: https://resolution.nhs.uk/corporate-reports/
Note 22 Contingent assets and liabilities
Contingent assets and liabilities are potential assets and liabilities arising from past events, whose existence will only be confirmed by the occurrence of future events that are not entirely within the entity’s control.
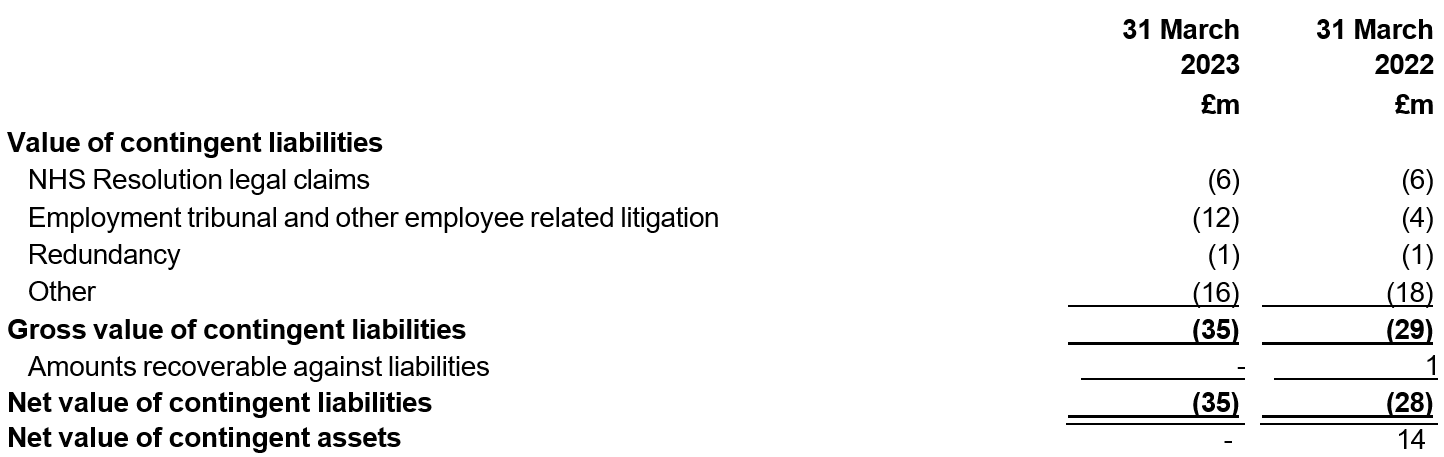
Note 23.1 Contractual capital commitments
At 31 March, contractual capital commitments not otherwise included in these financial statements were:

Note 23.2 Other financial commitments
NHS providers are committed to making the following payments under non-cancellable contracts (which are not leases, PFI contracts or other service concession arrangements):

Note 24 On-SoFP PFI, LIFT and other service concession arrangements
Note 24.1 On-SoFP PFI, LIFT and other service concession obligations
NHS providers recognise the following obligations in respect of assets included in the on-Statement of Financial Position PFI and LIFT schemes:
|
| 31 March 2023£m | 31 March 2022 £m |
|
Gross PFI, LIFT or other service concession liabilities |
13,457 |
14,559 |
|
Of which liabilities are due |
|
|
|
– not later than one year; |
828 |
866 |
|
– later than one year and not later than five years; |
3,170 |
3,244 |
|
– later than five years. |
9,459 |
10,449 |
|
Finance charges allocated to future periods |
(5,795) |
(6,545) |
|
Net PFI, LIFT or other service concession arrangement obligation |
7,662 |
8,014 |
|
– not later than one year; |
340 |
344 |
|
– later than one year and not later than five years; |
1,371 |
1,341 |
|
– later than five years. |
5,950 |
6,329 |
Note 24.2 Total service concession arrangement commitments
NHS providers are committed to making the following total payments in respect of on-Statement of Financial Position PFI, LIFT and other service concession arrangements:
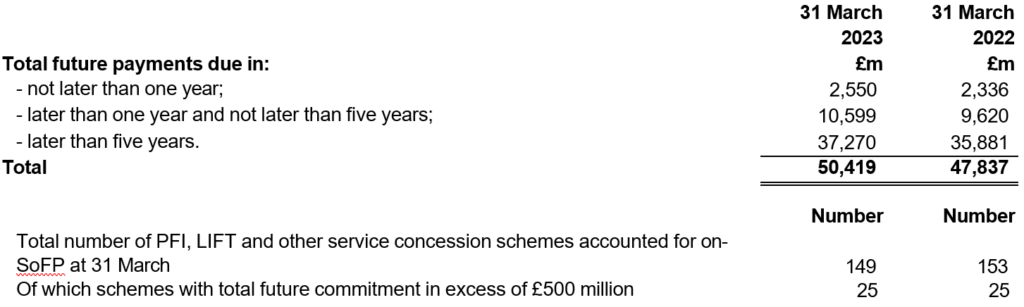
Note 24.3 Analysis of amounts paid to service concession operators
This note shows the total amount paid to the service concession operator in the year, on an accruals basis. The constituent parts of the unitary payment are taken to the Consolidated Statement of Comprehensive Income or Consolidated Statement of Financial Position as appropriate.
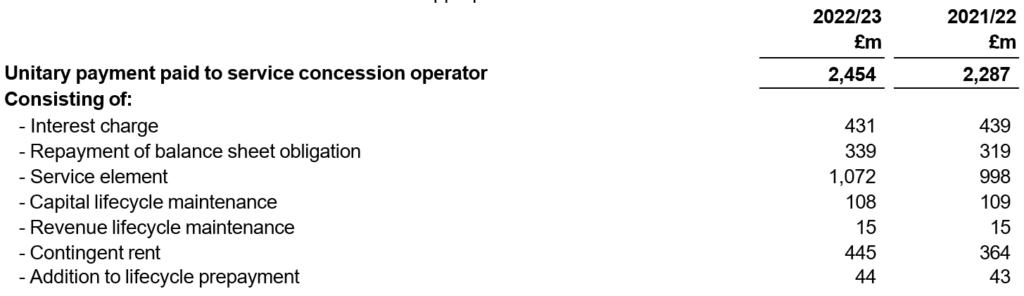
Note 25 Off-SoFP PFI, LIFT and other service concession arrangements
NHS providers incurred the following charges in respect of off-Statement of Financial Position PFI and LIFT schemes:
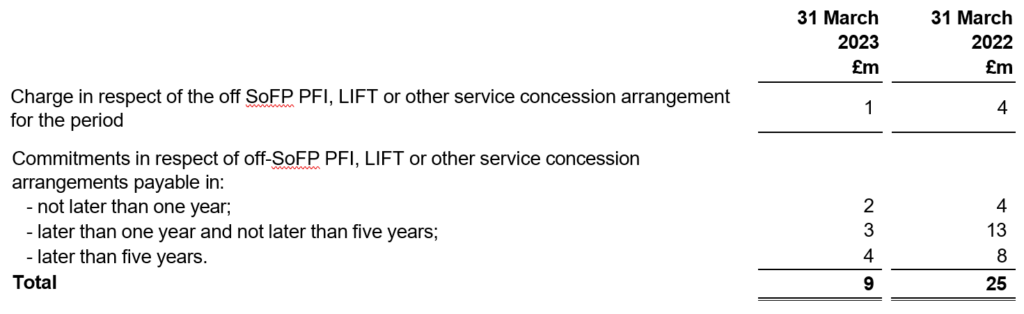
Note 26 Financial instruments
Note 26.1 Financial assets as at 31 March 2023
| Financial assets at amortised cost | Financial assets at fair value through I&E | Financial assets at fair value through OCI | Total | |
|---|---|---|---|---|
|
Carrying values of financial assets as at 31 March 2023 |
£m |
£m |
£m |
£m |
|
Receivables excluding non-financial assets |
5,484 |
– |
– |
5,484 |
|
Financial assets / investments |
89 |
1 |
4 |
94 |
|
Cash and cash equivalents at bank and in hand* |
12,688 |
– |
– |
12,688 |
|
NHS charitable funds financial assets |
182 |
128 |
44 |
354 |
|
Total at 31 March 2023 |
18,443 |
129 |
48 |
18,620 |
* Cash and cash equivalents excludes cash held by NHS charitable funds, which is shown within the final row above.
Note 26.2 Financial assets as at 31 March 2022
| Financial assets at amortised cost | Financial assets at fair value through I&E | Financial assets at fair value through OCI | Total | |
|---|---|---|---|---|
|
Carrying values of financial assets as at 31 March 2022 |
£m |
£m |
£m |
£m |
|
Receivables excluding non-financial assets |
2,883 |
– |
– |
2,883 |
|
Financial assets / investments |
82 |
1 |
5 |
88 |
|
Cash and cash equivalents at bank and in hand* |
15,426 |
– |
– |
15,426 |
|
NHS charitable funds financial assets |
186 |
120 |
61 |
367 |
|
Total at 31 March 2022 |
18,577 |
121 |
66 |
18,764 |
* Cash and cash equivalents excludes cash held by NHS charitable funds, which is shown within the final row above.
Note 26.3 Financial liabilities
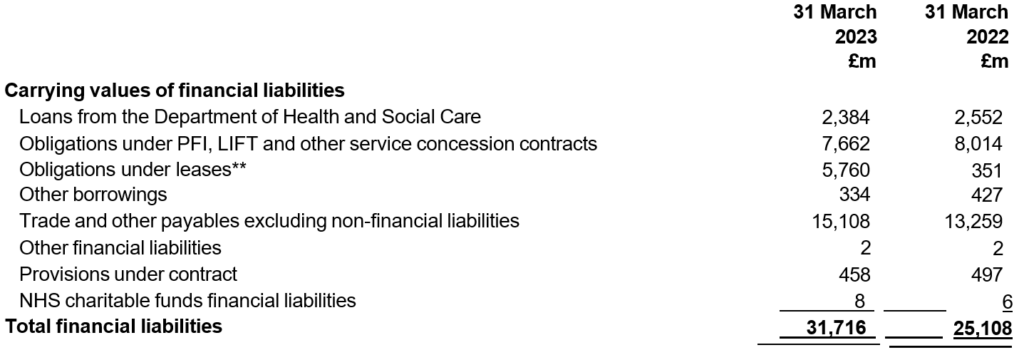
All financial liabilities are held at amortised cost.
**NHS providers have applied IFRS 16 Leases to lease arrangements within these accounts from 1 April 2022 without restatement of comparatives. More information about leases and the impact of this change in accounting policy can be found in Note 14.
Note 26.4 Maturity of financial liabilities
The following maturity profile of financial liabilities is based on the contractual undiscounted future cash flows. This differs to the amounts recognised in the statement of financial position which are discounted to present value.
| 31 March 2023 £m | 31 March 2022 £m | |
|---|---|---|
| Financial liabilities fall due in: |
|
|
| one year or less; | 17,313 | 14,876 |
| more than one year but not more than five years; | 6,905 | 4,701 |
| more than five years. | 14,182 | 12,634 |
| Total financial liabilities | 38,400 | 32,211 |
Note 26.5 Fair values of financial instruments
At a consolidated level, the fair values of financial instruments disclosed by individual providers do not differ materially from the book values disclosed above.
Note 26.6 Financial risk management
The risks arising from financial instruments and the NHS providers’ policies and processes in response to these risks are described below. Individual NHS providers may have their own bespoke policies and processes in place to deal with the risks they face as an entity.
Liquidity risk
The level of income generated by NHS providers is dependent on the contractual arrangements they have with their commissioners, whose resources are voted on annually by Parliament. In the majority of cases, these contractual arrangements are either based on a tariff for services performed or on a contract based on assumptions for the amount of work to be carried out by the NHS provider. Under current contracting arrangements, the majority of providers’ income from commissioners is under largely fixed payment arrangements which include minimal variability. More information is provided in the accounting policies.
NHS providers are required by legislation to carry out their functions effectively, efficiently and economically and under their licence conditions they are required to have systems and processes in place to ensure they comply with that duty and to ensure they are able to continue as a going concern as defined by generally accepted accounting practice.
NHS England supervises the risk of individual NHS providers breaching these and other licence conditions relating to finance by reviewing a range of financial information and categorising each trust according to our NHS Oversight Framework. It may provide mandated support to providers where required.
Details of the NHS System Framework used by NHS England for 2022/23 to monitor these risks can be accessed on the NHS England website.
As disclosed within the accounting policies at Note 1.24, these consolidated accounts are prepared on a going concern basis and we do not consider there to be a material uncertainty over going concern. It is deemed that there is not a risk that the consolidated provider sector would fail to meet its liabilities as they fall due.
Credit risk
The vast majority of the NHS provider sector’s income is generated from public sector bodies and as such is exposed to low credit risk as these bodies are financed through taxation.
NHS providers are permitted to generate income derived from private patients and overseas visitors without reciprocal arrangements, however this income contributes only 0.66% of total income from patient care activities generated in 2022/23 (2021/22: 0.53%). Other sources of income from non-public sector bodies amount to a small proportion of total provider income. Accordingly, the effective credit risk posed by income derived from private and overseas patients or non-public sector entities to the sector is low. Within cash and cash equivalents, £12.5 billion is held with the Government Banking Service and National Loans Fund. Individual providers have confirmed that they do not consider these deposits to be exposed to significant credit risk. The maximum exposures as at 31 March 2023 are in receivables, as disclosed in the receivables note.
Currency risk
The NHS provider sector operates principally within England and as such has only negligible amounts of transactions, assets and liabilities which are not in Sterling. Therefore the NHS provider sector has low exposure to currency risk.
Interest rate risk
NHS providers have the power to enter into loans and working capital facilities with commercial lenders. NHS providers are also able to borrow from DHSC. The term of DHSC loans can range up to 25 years but individual DHSC loan products may be shorter, with the potential for replacement DHSC loans to be at a different interest rate.
However given the total interest paid to DHSC by NHS providers (see note 10) this is not a material risk to the consolidated NHS provider accounts.
Note 27 Analysis of NHS charitable funds reserves

NHS charitable funds are consolidated by 44 NHS providers where the trust determines they have control (2021/22: 43) as outlined in accounting policy 1.1. Other providers may also have charities meeting the definition of local control that are not locally consolidated on the grounds of materiality.
Restricted funds are funds that are to be used in accordance with specific restrictions imposed by the donor, for example where the donor has specified that their donation should be spent on a specified ward, patients, nurses or project fund. Endowment funds are funds which the trustees are required to invest or to keep and use for the charity’s purposes.
Unrestricted income funds comprise those funds that the trustees are free to use for any purpose in furtherance of the charitable objects. Unrestricted funds include general funds, where the donor has not specified or restricted the use the charity may make of their donation. General funds additionally generate income from Gift Aid, investment income, interest and donations given specifically to cover running costs.
Note 28.1 Losses and special payments
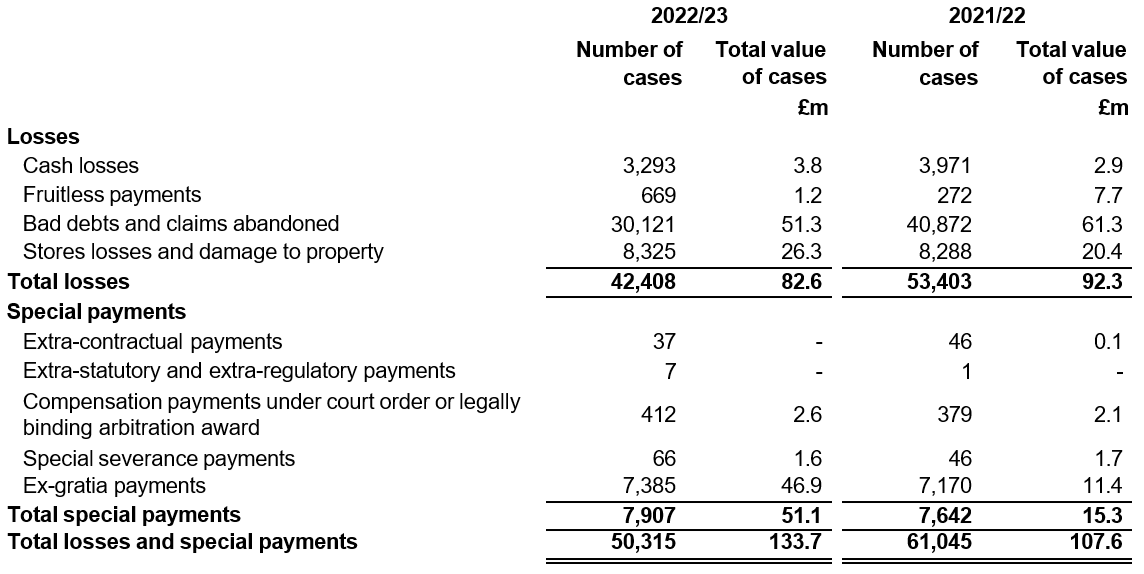
The total losses disclosed here are higher than the amounts included in the line ‘Losses, ex gratia and special payments’ in note 6.1 as NHS providers include some losses in other lines within that note.
Note 28.2 Losses and special payments in excess of £300,000
HM Treasury requires additional disclosure of losses or special payments individually in excess of £0.3 million.
In 2022/23 33 trusts reported 35 individual losses or special payments in excess of £0.3 million, totalling £38.3 million:
- Nottingham University Hospitals NHS Trust recorded a loss of £0.8 million relating to a fine for failings in maternity care.
- South Warwickshire University NHS Foundation Trust recorded a special severance payment of £0.5 million.• The Roya
- Marsden NHS Fondation Trust recorded a fraud case of £0.4 million.
- Imperial College Healthcare NHS Trust wrote off £0.3 million of outstanding invoices due from an overseas visitor.
- Sandwell And West Birmingham Hospitals NHS Trust wrote off £1.5 million of outstanding invoices due from a local authority in relation to delayed transfers of care.
- The following 9 trusts have recorded £5.1 million of pharmacy losses and osolete stock write-offs:
- Buckinghamshire Healthcare NHS Trust (£0.5 million)
- London North West University Healthcare NHS Trust (£0.3 million)
- North Middlesex University Hospital NHS Trust (£0.4 million)
- Northern Care Alliance NHS Foundation Trust (£0.5 million)
- Royal National Orthopaedic Hospital NHS Trust (£1.2 million)
- Royal Papworth Hospital NHS Foundation Trust (£0.4 million)
- Royal Surrey NHS Foundation Trust (£0.6 million)
- South Warwickshire University NHS Foundation Trust (£0.4 million)
- The Hillingdon Hospitals NHS Foundation Trust (£0.8 million)
- 19 trusts made ex gratia payments to staff members relating to VAT refunds in lease car schemes totalling £14.9 million. Each trust decision (covering all applicable staff) is counted as a single case in the table in note 28.1.
- In addition, the following 2 trusts made ex gratia payments to their related charities from funds generated by the provider. Prospective approval was not sought by the trusts for these payments and the application for retrospective approval has been declined by HM Treasury. These payments are therefore irregular.
- The Christie NHS Foundation Trust (£5.8 million)
- The Royal Marsden NHS Foundation Trust (£9 million)
In 2021/22 6 trusts reported 7 individual losses or special payments in excess of £0.3 million, totalling £8.2 million:
- East Suffolk and North Essex NHS Foundation Trust (£0.8 million)
- Manchester University NHS Foundation Trust (£0.3 million)
- Mid and South Essex NHS Foundation Trust (£0.5 million)
- Northern Care Alliance NHS Foundation Trust (£0.4 million)
- Royal Surrey NHS Foundation Trust (£0.6 million)
- University Hospitals Plymouth NHS Trust (two cases totalling £5.6 million)
Note 29 Related parties
DHSC is regarded as a related party of NHS trusts and NHS foundation trusts. Per paragraph 25 of IAS 24 Related party disclosures , government-related entities are not required to disclose balances and transactions with entities that have the same government control. The information below was collected from NHS trusts and NHS foundation trusts, who were advised to exclude from the data collection balances and transactions with entities within the whole of government accounts boundary.
Information on related party balances and transactions with charitable funds and group entities below only relates to where the entity has not been consolidated within the local accounts, and thus not consolidated within these consolidated provider accounts.
Details of NHS providers’ material related party transactions are shown in the accounts of the individual NHS providers.
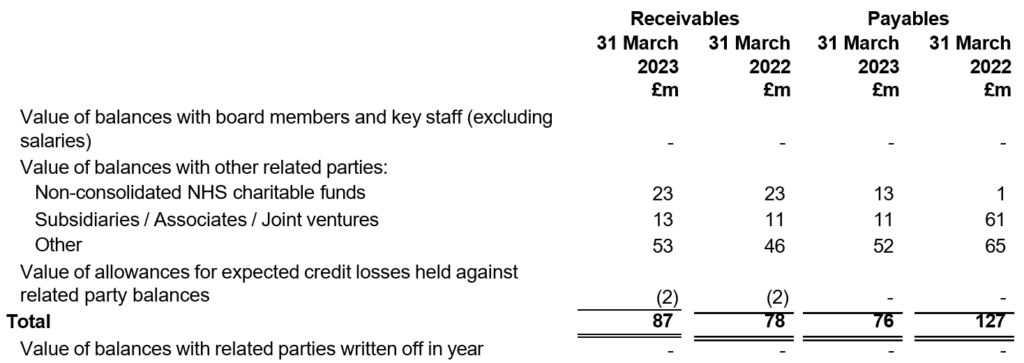
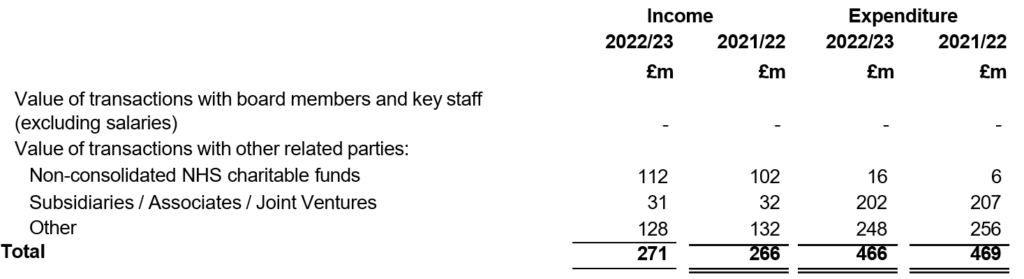
Note 30 Transfers by absorption
Most business combinations within the public sector are accounted for using absorption accounting principles. Under this approach, balances are written out by the divesting organisation and recorded by the receiving organisation at their book values at the point in transfer. A gain or loss corresponding to the value of net assets is recognised within income and expenditure. More details are provided in accounting policy 1.1.
Transactions accounted for under absorption accounting: 2022/23
Absorption transfers occurring between NHS providers are eliminated within these accounts. The following provider acquisition was eliminated in 2022/23:
| Receiving body | Divesting body | Date of transfer |
|---|---|---|
| Royal Devon University Healthcare NHS Foundation Trust | Northern Devon Healthcare NHS Trust | 1 April 2022 |
The following absorption transfers occurred between NHS providers and other government bodies during 2022/23 and so reflect absorption movements in or out of the consolidated NHS provider accounts:
| Details | Non- current assets £m | Current assets £m | Current liabilities £m | Non- current liabilities £m | Total net assets £m |
|---|---|---|---|---|---|
| Transfers from NHS Property Services (modified absorption) | 23.4 | – | – | – | 23.4 |
| Transfers to NHS Property Services | (5.6) | (0.2) | – | 1.8 | (4.0) |
| Transfer to Greater Manchester Integrated Care Board | – | (6.1) | 6.1 | – | – |
| Totals | 17.8 | (6.3) | 6.1 | 1.8 | 19.4 |
Transfers from NHS Property Services under modified absorption accounting related to assets formerly held by primary care trusts received by Kent Community Health NHS Foundation Trust and East Suffolk and North Essex NHS Foundation Trust. See accounting policy 1.1 for details of the ‘modified’ treatment that applies to gains recognised on these transfers.
The transfers to NHS Property Services under ordinary absorption accounting relate to the transfer of the Richard Hotham Unit from Sussex Partnership NHS Foundation Trust and community services properties from Pennine Care NHS Foundation Trust.
Northern Care Alliance NHS Foundation Trust transferred the Greater Manchester Shared Service to NHS Greater Manchester Integrated Care Board under ordinary absorption accounting.
The sum of the absorption gains and losses rows in the other notes to the accounts do not equal the balances presented in this note, as not all notes (for example payables and receivables) contain details of the movements in the year.
Transactions accounted for under absorption accounting: 2021/22
Absorption transfers occurring between NHS providers are eliminated within these accounts. The transfers eliminated in 2021/22 include the following provider transactions:
| Receiving body | Divesting body | Date of transfer |
|---|---|---|
| University Hospitals Sussex NHS Foundation Trust | Brighton and Sussex University Hospitals NHS Trust | 1 April 2021 |
| Greater Manchester Mental Health NHS Foundation Trust | North West Boroughs Healthcare NHS Foundation Trust | 1 April 2021 |
| Mersey Care NHS Foundation Trust | 1 June 2021 | |
| Manchester University Hospitals NHS Foundation Trust Foundation Trust | Pennine Acute Hospital NHS Trust | 1 April 2021 |
| Northern Care Alliance NHS Foundation Trust | 1 October 2021 |
The following transfers by absorption occurred between NHS providers and other government bodies during 2021/22 and so reflect absorption movements in or out of the consolidated NHS provider accounts:
Details | Non- current assets £m | Current assets £m | Current liabilities £m | Non- current liabilities £m | Total net assets £m |
|---|---|---|---|---|---|
| Transfers from NHS Property Services (modified absorption) | 5.5 | – | – | – | 5.5 |
| Transfer to NHS Property Services | (8.8) | – | 3.6 | – | (5.2) |
| Totals | (3.3) | – | 3.6 | – | 0.3 |
Note 31 Consolidation of unaudited local provider accounts
As explained in accounting policy note 1.1, these accounts are prepared based on locally audited provider accounts. To expedite national financial reporting, the disclosures in these consolidated accounts were finalised on 15 January 2024 using unaudited financial information for two providers:
- Buckinghamshire Healthcare NHS Trust – dispensation was given by NHS England for the Trust and its auditor to plan the audit of these accounts to take place outside of the normal accounts timetable. This followed the Trust having difficulty appointing an auditor due to the wider capacity constraints in the local audit market. No significant issues relating to the audit have been reported to us. More information on local audit is provided in the annual governance statement accompanying these consolidated accounts.
- East Suffolk and North Essex NHS Foundation Trust – the auditor, BDO LLP, has not been able to complete its audit prior to these accounts disclosures being prepared. No significant issues relating to the audit have been reported to us.
A summary of the financial statements of these two providers is presented below:
| NHS provider | Operating income | Operating expenses | Property, plant and equipment | All other assets | Liabilities | Reserves | |
| Buckinghamshire Healthcare NHS Trust | 603 | (595) | 351 | 85 | (124) | 312 | |
| East Suffolk and North Essex NHS Foundation Trust | 1,020 | (1,011) | 431 | 209 | (233) | 407 | |
| Total in providers (before considering additional national procedures) | 1,623 | (1,606) | 782 | 294 | (357) | 719 | |
With reference to materiality for these consolidated accounts of £1.15 billion, operating income and operating expenditure for these two trusts are material so we have performed additional assurance procedures on these balances plus public dividend capital within reserves:
- operating income: amounts from NHS England group entities have been validated to NHS England’s financial ledger
- operating expenses: within these figures, some amounts have been validated to source evidence for payroll expenditure
- public dividend capital reserve: balances validated against central records from the Department of Health and Social Care
Following these procedures we are satisfied that the residual balances over which uncertainty remains are not material to these consolidated accounts.
The consolidated provider accounts for 2021/22 were finalised using unaudited information for three NHS providers. These three providers have now published audited accounts for 2021/22. Any changes in their financial information was not material and such amendments have been presented as 2022/23 items in these consolidated accounts. More information can be found in the annual governance statement accompanying these consolidated accounts.
Note 32 Providers with modified audit opinions
The external auditor at University Hospitals of Leicester NHS Trust has qualified the Trust’s audit opinion in two respects: insufficient audit evidence over existence of plant and equipment assets with a total net book value of £110.8 million, and the impact of additional qualifications in previous years’ financial statements affecting comparative figures for 2021/22. The effects of these matters are not numerically material to these consolidated accounts but we do consider this modified audit opinion to be material by nature. More information is provided as part of the annual governance statement presented alongside these accounts.
Note 33 Prior period adjustments
Sector-wide changes in accounting policy
In 2022/23, there have been no changes in accounting policy requiring sector-wide restatement of comparatives.
IFRS 16 Leases has been applied retrospectively without restatement as described in our accounting policy in Note 1.10
Other prior period adjustments applied by NHS providers
Local prior period adjustments in individual NHS providers are not material to the consolidated accounts, and so their effects are instead disclosed in the current year.
Note 34 Events after the reporting date
As at 31 March 2023 there were 212 NHS providers.
On 1 April 2023, all services previously provided by Yeovil District Hospital NHS Foundation Trust transferred to Somerset NHS Foundation Trust and Yeovil District Hospital NHS Foundation Trust was dissolved.
On 1 July 2023, all services previously provided by Southport and Ormskirk Hospital NHS Trust transferred to St. Helens and Knowsley Hospital Services NHS Trust and Southport and Ormskirk Hospital NHS Trust was dissolved. Following the acquisition, the acquiring trust changed its name to Mersey and West Lancashire Teaching Hospitals NHS Trust.
These transactions will eliminate and will therefore have no impact on the 2023/24 consolidated NHS provider accounts. As at the date of authorisation of these accounts, there are 210 NHS providers.
In accordance with the requirements of IAS 10 Events after the reporting period , events are considered up to the date on which the accounts are authorised for issue. This is interpreted as the date of the Certificate and Report of the Comptroller and Auditor General.

