1. Introduction
A pandemic is where an infectious disease spreads across whole countries, international boundaries or continents at the same time, usually driven by a novel pathogen (virus, bacteria, fungi or other organism) to which there is no population immunity.
The threat and potential impact of pandemics are such that they remain a top risk for the UK and continue to direct significant amounts of activity on a global basis.
Experts believe the most likely cause of a future pandemic will be a respiratory virus; however, the government continues to plan and prepare for a range of pandemic and emerging infectious disease scenarios, across the five different transmission routes: respiratory (droplets and aerosols), blood and body fluids, direct and indirect contact, ingestion (food and water) and by vectors such as mosquitos (see the National Risk Register 2023 for information).
Novel pathogens can present different challenges to existing circulating biological agents, even where they closely resemble them. This may include extended duration of a pandemic (many months, even years), multiple waves of infection, vaccinations or specific treatments not currently or readily available, and wider or atypical population groups being at risk and affected.
The unequal risk and impact of a future pandemic will undoubtedly exacerbate existing health inequalities and cause new disparities for communities across the country.
1.1 Planning assumptions
Equity of preparedness and response must be considered at all levels, in all responding organisations and within all communities in England, to ensure the NHS response does not create, and ideally moderates, health inequalities.
When responding to such diverse, unpredictable incidents as pandemics it is vital that plans are agile and flexible. Planning assumptions (Appendix 5) can be used as a guide to inform and develop effective response plans at all levels; however, they must not be seen as a prediction. While the profile of the next pandemic remains unknown, it is essential NHS England considers all possible impacts and is ready to lead the NHS response in conjunction with relevant partners. Lessons identified during the responses to the 2009/10 influenza pandemic caused by the A(H1N1) virus, the 2010/11 winter seasonal influenza outbreak and COVID-19 will continue to inform preparedness.
This interim document will be reviewed and updated as necessary when learning from the COVID-19 inquiry is made available and updated Government UK guidance is published.
2. Purpose of this document
This document provides a framework for NHS England when managing the response to a pandemic and should be read in conjunction with the supporting documents indicated at Appendix 6. The purpose of this document is to outline the pandemic-specific roles and responsibilities of NHS England, with a focus on the ‘command, control, coordination and communication’ (C4) and governance arrangements for the NHS.
At all times throughout a pandemic response, NHS England must fulfil the relevant responsibilities of all related legislation, including any newly issued in a pandemic. Current systems will be built upon C4 arrangements where possible rather than developing something new, and must be practical, appropriate and enhance the response.
3. Links with wider NHS emergency preparedness, resilience and response
This document supplements the strategic national framework for emergency preparedness, resilience and response (EPRR), the NHS England incident response plan national (IRP(N)) and the NHS England IRP(N) Annex A – protracted incidents. It should also be read alongside other key guidance that sets out the arrangements for NHS England in planning for and responding to pandemics and other emergencies, which can be found on the NHS England website.
As the disease spreads and the population is affected, NHS England (national) will consider the scale and the potential impacts on its own services and the arrangements required to support the wider NHS to maintain patient care. This will require national coordination. This may also be influenced at the point a pandemic is declared by the World Health Organisation (WHO).
As such, NHS England (national) will declare a Level 4 incident and will provide command and control, with NHS England (regions) co-ordinating and supporting the NHS response in collaboration with local commissioners at the tactical level. This is based on lessons identified from the response to the COVID-19 pandemic.
The IRP(N) is the overarching generic plan that details how NHS England prepares for, reviews and responds to any health-related incident at a national level. It enables NHS England to deliver corporate responsibilities in response to any incident.
Given the potential for a pandemic to last for an extended duration and be of a significant complexity, which may require enhanced resources and/or mutual aid over and above those required to respond to an isolated incident, NHS England will give early consideration to invoking the IRP(N) Annex A – protracted incidents, which describes the arrangements that may be put in place nationally following a declaration of a protracted incident.
NHS England will use established national and regional incident management structures and processes (Appendix 2), in parallel to those in place in the UK Health Security Agency (UKHSA) and the Department of Health and Social Care (DHSC), that will be used to support the response. NHS England will notify the Devolved Administrations of the arrangements established.
Following the principle of subsidiarity, decisions and actions should be taken at the lowest appropriate level, with co-ordination at the highest necessary level.
Unless explicitly stated otherwise, the term ‘NHS’ is used to refer to ‘commissioners and providers of NHS funded care.’ The term ‘testing’ is used to refer to all methods of taking specimens for the purposes of detection of active or past infection.
4. Partner and wider society response
NHS England, integrated care boards (ICBs) and UKHSA have important roles to ensure a coordinated response that provides the service needed by patients. The Office of Health Improvement and Disparities (OHID) has an essential role to play in minimising health inequalities and maximising equity of response at all levels. Local resilience fora (LRFs) will coordinate multi-agency planning and response strategies.
The wider pandemic response will require support and input from NHS England, as well as ICBs, local NHS and social care providers. Local health resilience partnerships (LHRPs) provide a strategic forum to facilitate health sector preparedness for emergencies and have a role in facilitating integrated plans across the health economy to respond to a pandemic alongside multi-agency partners.
The response to any future pandemic may require co-ordinated action across different organisations within the health and social care sector. There may also be a wider government and societal response required on a range of issues that form part of the pandemic response (including but not limited to; treatments, vaccines, personal protective equipment (PPE), procurement, borders, legislation and non-pharmaceutical interventions both in healthcare settings and across society). NHS England may need to play a supporting or coordinating role in these elements of a pandemic response. This document does not set out the detail of wider system organisations’ roles and responsibilities, which will need to be covered in their own arrangements.
5. Overseas arrivals to England
People entering the UK from overseas are likely to need support at the early stages of a future pandemic, just as they did for COVID-19. This included British nationals returning voluntarily or following the guidance of the FCDO and British nationals who had been isolating on cruise ships where there had been outbreaks or quarantine was instigated by other countries.
The UK Government instigated hotel quarantine and later home isolation requirements for these people, and this was supported by the local NHS and public health teams. Later in the response, students and health care workers returning to the UK also had to isolate for periods of time before rejoining wider society, if they entered the UK from certain ‘red listed’ countries.
NHS England (national) will set the policy and strategy around supporting these people from a healthcare perspective, and regional and local NHS teams will be required to implement this operationally.
6. NHS England aim and objectives
The aim of NHS England when responding to a pandemic is:
To coordinate the NHS response to the pandemic ensuring access to, and delivery of, safe, effective and timely care for patients, and to safeguard staff wellbeing and safety in order to mitigate identified risks and lessen potential harm.
Our objectives in response to a pandemic are to:
- support the provision of treatment and care to patients across a range of NHS settings
- provide the public with information regarding access to NHS services
- minimise the impact on NHS services
- maintain and support NHS staff health, safety and welfare at all levels throughout and after the response
- restore and recover services inclusively taking equality and health inequalities considerations into account (appendix 1);
- identify, consider and mitigate where possible health inequalities, and ensure healthcare equity for all patients and staff, throughout the pandemic
- ensure a coordinated and cohesive response across all directorates as outlined in the NHS England IRP(N)
- maintain timely and appropriate situational awareness to inform decisions
- undertake debriefs and identify lessons which can be implemented to enhance our response to future pandemics and other incidents
7. NHS England roles and responsibilities during a pandemic
NHS England is, in line with the Civil Contingencies Act (2004) as well as the EPRR Framework, responsible for the command, control, communication, coordination, and leadership of the NHS in the event of a major incident or an emergency. Furthermore, it has well-rehearsed national and regional incident management structures to support a pandemic response.
NHS England has a number of responsibilities in responding to an evolving or declared pandemic; these requirements will vary depending on which phase of the pandemic we are in. The following sections outline the responsibilities of both national and regional NHS England teams in each phase.
7.1 Preparedness before the pandemic
NHS England must take steps to be prepared to respond to a future pandemic. This includes supporting NHS and partner organisations where appropriate. This table outlines key organisation responsibilities to be undertaken before a pandemic. Pragmatic decisions should be taken to identify where, how and by whom these are delivered. This should not be seen as an exhaustive list as other requirements may be identified.
National | Regional | |
|---|---|---|
monitor the national and international situation through liaison with partners such as DHSC and UKHSA | Yes | No |
convene a planning group to maintain oversight and contribute to NHS and partnership preparedness activities | Yes | No |
act as a conduit for consistent information and advice from DHSC and UKHSA to the NHS | Yes | Yes |
monitor and evaluate risks and impacts, identifying and mitigating gaps where possible | Yes | Yes |
provide up to date operational guidance to the NHS for use in a pandemic | Yes | No |
ensure that NHS commissioned services (including nationally and directly commissioned specialist services) are included in planning arrangements | Yes | Yes |
work with the local NHS to facilitate the development of agreements with the independent and voluntary healthcare sector | No | Yes |
lead NHS pandemic preparedness, encouraging and supporting local health preparedness | No | Yes |
ensure the development, maintenance, testing and exercising of effective and integrated health response plans | Yes | Yes |
develop an understanding of local plans and arrangements to support local activities | No | Yes |
work with local NHS and partners to plan and share good practice, address specific issues and keep plans up to date | No | Yes |
as appropriate, work with relevant partners to identify operational delivery aspects (eg vaccine delivery) | Yes | Yes |
ensure staff within NHS England and the wider health economy are supported and informed in pandemic preparedness and response | Yes | Yes |
undertake appropriate assurance to ensure the NHS has adequate plans in place for a pandemic (eg the annual EPRR assurance process and regular LHRP discussions) | Yes | Yes |
ensure the LHRP and LRF is appropriately appraised of relevant NHS issues and progress regarding pandemic preparedness through locally agreed arrangements | No | Yes |
7.2 Managing the initial cases
When there are initial cases and small clusters in the country, the focus is on containment and understanding the epidemiology of the disease as well as providing patient care and support.
Different parts of the country may be differentially affected at this time, depending on where early cases occur. Therefore, not all regions or teams may be undertaking all roles and responsibilities to the same degree at the same time. The spread of the virus across the country will require localities working together to provide a coherent national pandemic response.
National | Regional | |
|---|---|---|
monitor the national and international situation through liaison with partners such as DHSC and UKHSA | Yes | No |
monitor and evaluate risks, issues and impacts, identifying and mitigating gaps where possible | Yes | Yes |
lead NHS preparedness and response, encouraging and supporting local health organisations | No | Yes |
provide up to date operational guidance to the NHS | Yes | No |
convene response groups with appropriate representation to lead, command, control, co-ordination and communication of the internal and wider NHS response | Yes | Yes |
convene a recovery team with appropriate representation to oversee a return to normal business functioning within NHS England and the NHS | Yes | Yes |
represent the NHS at LRF strategic coordination group (SCG) and LHRP meetings, and where appropriate be the lead agency/Chair where locally agreed | No | Yes |
agree the level of response for the NHS locally and ensure the NHS and relevant partners are kept appropriately appraised | No | Yes |
review any agreements with independent or voluntary health sector providers and LRF partners to support the local NHS | Yes | Yes |
provide support and guidance regarding healthcare to local NHS organisations and LRF partners as necessary | No | Yes |
facilitate the flow of information regarding the NHS response and system pressures to DHSC and others | Yes | No |
ensure staff NHS England and the wider health economy are supported and informed | Yes | Yes |
oversee national personal protective equipment (PPE) stock management and distribution to local NHS providers | Yes | Yes |
activate processes to collate information from the NHS through regular situation reports (SitReps) | Yes | Yes |
support UKHSA and the NHS to access tests and test people in line with national guidance to inform patient management, epidemiological intelligence, and the response | Yes | Yes |
support appropriate repatriation, quarantine and isolation of people as required in specialist locations or their homes | Yes | Yes |
7.3 Treating clusters and escalating to managing a national outbreak
As the number of confirmed cases rises there will be increasing demand on services. There will be patients in different parts of the country, and increasing numbers of NHS organisations will be responding. National and regional oversight will ensure the NHS functions cohesively across the country to provide the best care for all patients, as consistently as possible. One of the key aspects will be a need to understand the impact on operational capacity using existing processes across the system to manage capacity and demand during periods of increased activity. Actions from the previous stage of the response remain relevant, although they may require increased implementation across wider areas or for longer durations. Additional actions are set out below.
In addition to actions in the previous stage… | National | Regional |
|---|---|---|
consider any potential in extremis measures that might need to be enacted and ensure appropriate engagement and discussion with relevant bodies and staff | Yes | No |
facilitate decision making on the provision of NHS services and service priorities in conjunction with DHSC and commissioners | Yes | Yes |
support any changes to service or system delivery as required (eg assessment pods, community screening and isolation wards) ensuring appropriate engagement with DHSC, professional bodies and others | Yes | Yes |
enact business continuity plans and mobilise resources as required to deliver the specific response elements and support essential normal business where appropriate | Yes | Yes |
ensure the most effective use of resources through adapting the response according to capacity, including commissioning additional NHS capacity where required and possible | Yes | Yes |
appropriately enact any agreements with independent or voluntary health sector providers to support the local NHS | No | Yes |
oversee delivery of any ongoing testing in collaboration with UKHSA and local providers | Yes | Yes |
7.4 Escalation and de-escalation
Changes in incident response level can only be authorised by the NHS England Chief Executive Officer (CEO) or Accountable Emergency Officer (AEO) on the advice of the incident director (national). Within a protracted incident, the de-escalation or removal of the protracted nature of the incident will be agreed by the national incident response board (NIRB) and authorised by the CEO or AEO.
Criteria for escalation and de-escalation are at paragraph 8 of the NHS England IRP(N).
8. Command, control and co-ordination
8.1 Leadership
In a Level 4 incident NHS England will lead the overall NHS response and will coordinate the system to ensure the best possible care for all patients and impacted individuals within available resources. Leadership from the national team to regions will be essential to ensure a joined up and consistent approach.
NHS England will establish an overarching national incident response board as appropriate (NIRB, see Appendix 2) accountable to the NHS executive and NHS England boards, with membership at national executive level, to oversee the internal response co-ordination and delivery, as well as the wider NHS response.
In all response aspects, the NHS England NIRB will set strategic direction, and there will not be scope for significant regionalisation except for operational requirements or managing impacts caused by loss of supplies.
Strong clinical leadership throughout from national medical and nursing directors will be essential to support their regional counterparts and peers in provider organisations.
8.2 Staffing
The response to a pandemic is likely to be protracted over several months or even years. It will be important that the response can be maintained seven days a week, with the potential for 24-hour working, if required.
Consequently, the response must not rely solely on EPRR or active on-call staff. Sufficient staff support and resource should be identified to deliver the response and protect the EPRR function to respond to concurrent events or incidents.
Staff will be drawn from across all of NHS England’s directorates and teams (see Appendix 2). Staff with specific interest and skills to support the response should be involved where possible and appropriate at the relevant levels. The organisational ‘reservist model’, with central coordination and oversight through close working with HR, may be the most effective way to achieve this.
The roles staff are expected to carry out in response to a protracted incident should, whenever possible, be broadly comparable to (or a natural extension of) those they normally carry out. Further training will be delivered, both proactively and reactively, in line with any requirement to increase staffing.
The minimum occupational standards (MOS) for EPRR sets out the minimum national occupational standards that health commanders, managers and staff responding to incidents as part of an incident management team and other staff involved in EPRR must achieve in order to be competent and effectively undertake their roles.
Staff welfare must be considered and supported throughout. Not only is this a direct duty of care of the organisation but will also help ensure the best possible response by the system for patients and the public.
9. Recovery
In line with good practice, recovery work should be considered at all levels in NHS England, as well as across the wider system, early in the response. It is essential the recovery phase is planned and managed. This will help ensure services are restored in a timely and appropriate way to normalise the system, potentially to a new definition of what constitutes normal. Command and control processes for recovery should mirror the processes established by response teams.
The indicator for this stage is when pandemic activity is either significantly reduced compared to the peak, or when the activity is considered to be within acceptable parameters. An overview of how services’ capacities are able to meet demand will also inform this decision.
National | Regional | |
|---|---|---|
ensure readiness is maintained internally and across the NHS to manage further outbreaks or incidents | Yes | Yes |
acknowledge staff contributions and review welfare arrangements, providing support as necessary | Yes | Yes |
review staffing arrangements in conjunction with the local NHS organisations | Yes | Yes |
assess the impact through comprehensive debriefing internally, of NHS organisations, and with partners | Yes | Yes |
ensure a staged recovery of NHS England and the NHS as soon as appropriate | Yes | Yes |
review national and regional resources and capabilities | Yes | Yes |
review effectiveness of pandemic specific interventions, such as repatriation, quarantine/ home isolation, testing and PPE distribution | Yes | Yes |
oversee return of unused countermeasures as required to national stockpiles | Yes | Yes |
review and report on response arrangements and update relevant plans to reflect lessons identified | Yes | Yes |
review health inequality and equity aspects of the response to ensure any disproportionalities that emerged through the pandemic are mitigated as soon as possible | Yes | Yes |
contribute to any national inquiries as appropriate | Yes | Yes |
9.1 Recovery support
Following an extended response, irrespective of severity, recovery across the NHS will be challenging and take a significant period. Not all services which may have been suspended will be able to restart at the same time, and support will be required from teams across NHS England, to the wider NHS as well as internally. Recovery support should be governed by staff who are empowered to make decisions and allocate funds (e.g. to commission new services) if needed and in line with available legal powers.
Recovery support will need to consider ways to rebuild a healthcare infrastructure which can allow prioritisation of care to meet demand (such as psychosocial support), with a planned approach for returning to business as usual or a new way of working. Within the latter, considerations should be made around what new services, commissioned and/ or established specifically during the incident, the system will want to retain as part of business as usual.
Where a service was commissioned exceptionally by NHS England, there may need to be consideration of how that will be transitioned to more appropriate organisations where appropriate (e.g. ICBs) where any enabling legislation extending NHS England commissioning powers comes to an end. Any emergency arrangements or flexibilities in legislation established during a pandemic response may be time limited, and this will need to be considered and addressed in the recovery period.
10. Reporting and monitoring
Assurance is sought from the NHS of readiness to respond to pandemics through NHS core standards for EPRR as part of the annual assurance process. Additional assurance may be sought from organisations following the declaration of a pandemic, in relation to specific areas (e.g. testing capability, PPE etc.). It is recognised that the need to provide this assurance adds to the burden of responding to the pandemic; however, information and intelligence is a key requirement in supporting the NHS’s shared situational awareness and understanding of the risk. Information and assurance requests will be assessed by the strategic incident director as to their necessity prior to cascade and will be kept to a minimum wherever possible. Reporting requirements to the NHS England NIRB will include workstream and risk reports plus regular summary updates to the NHS executive and board.
As the outbreak reaches the UK and numbers of cases increase, there will be a regular requirement for situation reports (SitReps) to understand the local impact on the NHS using established emergency response mechanisms that may be supplemented as required to meet any additional requests specific to the pandemic. The daily schedule or ‘battle rhythm’ will be determined by the strategic incident director in line with the requirements of the incident – as such activity levels and information demands may increase or decrease accordingly.
Appendix 1: Equality and health inequalities
Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and processes cited in this document, we have given regard to the need to:
- eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it
- reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities
Consideration should be given to safeguarding of all staff, patients and the public throughout the extended response of a pandemic.
All guidance developed under this framework will have due regard to the need to reflect the impact on and from health inequalities in local populations during times of preparing for and responding to major incidents. Guidance on the NHS equality and health inequalities legal duties can be found on the NHS England website.
Health inequalities during a pandemic
Pandemics sadly present the potential for exacerbation of existing health inequalities, unequitable response to different communities, including access to specific treatment and routine services by patients, public and staff.
Reducing the actual or unintentional impact from health inequalities during a major incident is vital. The NHS will engage as much as possible with (and give consideration to) specific communities in planning for a pandemic.
National and regional incident directors, as part of their role leading the response to the pandemic, should consider the impact of their decisions on health inequalities within the existing population, wherever the population lives, and as a result of an incident. This, along with other decisions, should be appropriately recorded in incident logs along with the rationale underpinning the decision being made.
An equality and health inequalities impact assessment has been completed to support the development of this framework.
Health inequalities during COVID-19
COVID-19 is our most recent pandemic and the learnings regarding the health inequalities are a key aspect of our planning for a future pandemic. Reducing healthcare inequalities is an NHS priority. The COVID-19 pandemic highlighted stark health inequalities across England, exacerbated existing inequalities in life expectancy between the most and least deprived areas and had an unequal impact across ethnic groups. For more information see the Health Profile for England: 2021.
Further information on how health inequalities impacted on COVID-19 mortality rates is provided in Build Back Fairer: The COVID-19 Marmot Review.
Ethnicity
Significant disparities in relation to COVID-19 mortality by ethnicity have been identified. People of Bangladeshi ethnicity had around twice the risk of death than people of White British ethnicity. People of Chinese, Indian, Pakistani, other Asian, Black Caribbean and other Black ethnicity had between 10 and 50% higher risk of death when compared to White British.
Appendix 2: Response co-ordination structures
The following section outlines the response coordination structures and the anticipated pandemic response roles and responsibilities of teams in NHS England. Directorates and teams within NHS England will need to lead and support delivery of these responsibilities, as well as maintain essential business as usual functions.
The information provided below is not prescriptive or restrictive but is an indicator of how the response could be managed. It is recognised that modification will be required to ensure the response fits most effectively with existing structures and relationships.
NHS England national incident response board
Should the pandemic be declared a protracted incident, a national incident response board (NIRB) will be established. The NIRB will support NHS England’s response, including making decisions, recommendations and responding to the Government’s cross-departmental strategy and approach.
To ensure robust governance and clarity around reporting and decision-making, the NHS England NIRB will be established as a time-limited sub-committee of the NHS England board.
Key roles and responsibilities of the NHS England NIRB are as follows:
- set the strategic direction and provide oversight of the NHS England response to a pandemic
- consider and agree the approach to implementation of national NHS response measures and related key communications activity; agree any associated targets for regional and local response and monitor delivery of these
- determine the redeployment and/or reallocation of NHS England resource to support NHS operational readiness and the response to a pandemic
- provide oversight and challenge to NHS England workstreams, cells and task groups on progress and delivery, including the costs to the organisation and wider NHS and any communications and guidance associated with this work
- review key programme risks and any issues escalated to the board and, where necessary, determine appropriate action to mitigate these and resolve any barriers to progress
- ensure appropriate arrangements are established to maintain as much BAU activity as possible and at the appropriate time to manage recovery work following the pandemic incident
The NHS England NIRB will be chaired by the Chief Operating Officer (COO). Membership will consist of corporate and regional directors and representatives from the strategic incident and EPRR teams, and transformation directorate. Colleagues from DHSC, Ministry of Defence (MOD) and UKHSA are also invited to attend as key partners supporting the delivery of healthcare in a pandemic.
To support operational resilience, provision will be made for the national medical director or strategic commander to chair these meetings in the absence of the COO. Consideration will be given to deputy arrangements for all other members to support the continued operation of the NHS England NIRB.
Dedicated secretariat support will be provided to ensure appropriate governance and linkage with other key fora.
NIRB will be supported by a national incident management team (IMT(N)) that will deliver the operational and logistical aspects of the response as well as the policy, reporting, communications and briefing aspects.
Figure 2 shows the generic response structures that will be implemented in response to a pandemic.
Figure 2: NHS England typical response structure
NHS England Board
NHS England Executive
National Incident Response Board
The national incident response board is made up of senior executives across NHS England and is responsible for setting the strategic direction of the incident, making decisions and providing oversight and challenge to the incident response
PMO office
The PMO office is responsible for providing an effective programme management function across the incident response
Strategic Response Group (Transform)
Tactical Response Group (Contingency)
Operational Response Group (ICC(N)) (Co-ordinate)
Teams responsible for providing time boxed support to the incident response, supported by the cells
Cell 1
Cell 2
Cell 3
Cell 4
Cell 5
Cell 6
Cells provide specialist advice to support the forecasting, planning and delivery of the incident
The NHS England IRP(N) – Annex A protracted incidents provides further information about the constituent groups.
Incident management team (national)
The incident management team (national) (IMT(N)) will provide national operational direction, co-ordination and oversight of the NHS operational response. Key roles and responsibilities of the IMT(N) are as follows:
- act as the reporting line into the NHS England NIRB from NHS England regions including information from local commissioners and providers
- co-ordinate ad hoc and planned response arrangements such as repatriations, quarantine, community testing and home isolation
- oversee the delivery of escalation arrangements for routine and specialist resources (eg high consequence infectious diseases capacity and capability)
- provide advice and direction as necessary and make decisions in relation to risks and issues escalated by the regional IMTs
- collate and analyse information from the regions for submission to DHSC and others related to pressures and capacity within the NHS
- oversee the operational and logistical aspects of the response, eg PPE strategic reserve and stockpile management and distribution, vaccine and other clinical countermeasures delivery
- deliver the policy, reporting, communications and briefing aspects, including collation of situation reports, communications to the NHS, patients and the public, and briefings to NHS England senior management and DHSC
- work with NHS Employers towards supporting the wider NHS staffing community
- ensure prompt and timely establishment of a national Recovery Working Group (RWG) to run in parallel with the response
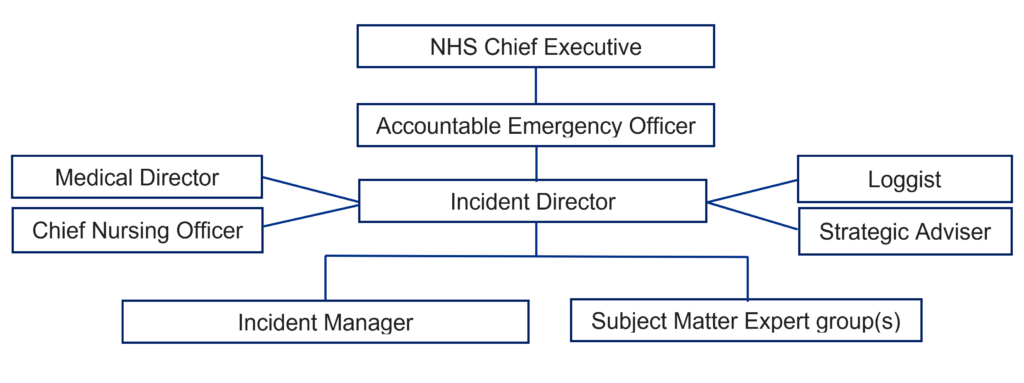
The typical structure of an IMT(N) is shown in Figure 3.
Figure 3: Typical structure of an incident management team (national)
Text description: the illustration shows a typical structure of an IMT(N).
This group will report into the NHS England NIRB and will be chaired by a senior member of NHS England, with other members drawn from across NHS England’s directorates and teams.
The IMT(N) will interact with the IMT (R)s and other partners through regular meetings and through the national operations centre.
Incident management teams (regional) (IMT(R)s)
There will be a need for more granular understanding and management of the intricacies and detail of the local response at regional level. It is suggested that each region establishes an incident management team (regional) (IMT(R)) function, with membership representing all directorates and relevant teams. This should link to the national response arrangements as well as with regional multi-agency partners involved in the response and existing regional management groups for strategic system oversight. They will lead the response within the regions, liaise with LRF and LHRP partners, and support ICBs and providers to deliver a safe and effective service by linking into the existing structures and capacity management processes.
The IMT(R)s will be responsible for several activities to oversee and deliver the NHS response. These will be flexed to meet demands and may not be required throughout the whole response. These include (but are not limited) to:
- lead the regional and local NHS response, appropriate to the current and predicted impact of the pandemic
- support the delivery of nationally directed interventions and actions such as testing, isolation and escalation
- ensure the NHS, partners, patients and the public are kept appraised of the evolving situation with particular reference to the regional response
- oversee and manage the NHS response through adapting the response according to capacity, implementing specific interventions, and commissioning additional NHS capacity where required
- ensure that regional NHS England directorates and teams enact their business continuity plans and mobilise resources appropriately as necessary
- ensure prompt and timely establishment of recovery working groups (RWG) at all appropriate levels to run in parallel with the response
- provide assurance and situation reports regarding the NHS response to the IMT(N)
- collate and analyse information for submission to the IMT(N), DHSC and others related to pressures and capacity within the NHS, alongside any directly submitted information to NHS England (national), DHSC, UKHSA or ONS
- support the local response, facilitating mutual aid (including from the military) if required
Regular discussions will be held between the IMT(N) and IMT(R)s to ensure co-ordinated response management. Regional representatives of NHS England directorates and teams will need to integrate into the IMT(R)s to ensure co-ordinated management of external and internal issues. The frequency, structure and timing of meetings to manage the response will be determined by demand.
Figure 4 shows an example of an IMT(R) with support cells, shown in Figure 3. Support cells will be determined by the nature of the response and will be adapted accordingly.
Figure 4: Example structure of an incident management team (regional)
Regional director
Regional incident response director
Cells
Critical care
Urgent and emergency care
Out of hospital
Supply chain and estates
Information
Workforce
Clinical
Communications
Patient transport
Independent sector
Nightingale hospital
Vaccination
Additional roles may be introduced as required.
All response coordination groups will have appropriate links to other organisations and responding groups. There will be regular engagement at all appropriate levels with DHSC, UKHSA, and partners to ensure the best possible response for patients. This may be through meetings/ teleconferences or embedded liaison officers to reflect pressures and escalation arrangements. Existing mechanisms and relationships will be used where possible.
Subject specific support teams
In addition to the core groups outlined above, some subject-specific workstreams and cells will be established to provide specific advice and guidance to help manage the response. The list of groups will evolve as the situation develops, and some will be more ‘task-and-finish’ in nature with a finite duration. Enabling workstreams should be established to oversee modelling, reporting, and analytics work, as well as aspects of business including workforce, finance and operationalisation of infection prevention and control (IPC) measures. The involvement and input from subject matter experts from other organisations (such as DHSC, UKHSA and other appropriate advisory groups) will be a key aspect of this, alongside NHS England staff.
Close alignment between different groups will be key due to the large number of independencies. Regional cells and workstreams are expected to be docking into national equivalents to ensure information flows adequately and effectively across the wider system.
Appendix 3: Support roles and responsibilities
Communications
Robust communications are an important part of the response. Communications colleagues are an intrinsic component of the NHS England response teams and need to function in a fully integrated manner with the wider response. Existing NHS England communications processes will ensure this is delivered.
NHS England’s communication activity with the NHS, partners, stakeholders and the public will build on existing mechanisms and good practice. Where appropriate, national messages will be developed and delivered in partnership with UKHSA and DHSC, and at regional level with LHRP and LRF partners. For pandemic response the overall health communications strategy is led by DHSC. The key communications priorities for NHS England will be to:
- support operational delivery
- keep NHS England staff and staff across the NHS well informed
- ensure that the public know how, where and when to access services
- support the public to maintain confidence in the NHS and wider health system’s ability to manage the situation
A wide range of channels will be used, as appropriate to the audience and message, including guidance for clinicians and NHS managers, print and broadcast media, as well as social media and marketing tools.
Health and Justice
NHS England has some specific responsibilities in the health and justice setting. These settings are prisons, immigration removal centres, young offender institutions and children and young people secure settings. The responsibilities are set out below:
- maintain equivalence of care for the health and justice patient group, effectively ensuring that irrespective of where the patient comes from, they will be given access to care in the same way as other patients
- work closely with the health and justice (national support teams) in NHS England, UKHSA and the His Majesty’s prison and probation service (HMPPS), Home Office (HO) and youth justice board (YJB) to ensure briefings, updates and actions are provided and addressed
- participate in and contribute to NHS England’s response arrangements to ensure critical health and justice links and partnerships are maintained
- provide leadership for the health and justice system ensuring close working with regions and lead commissioners, and through them ensure business continuity of commissioned healthcare provision within secure settings and that actions are delivered
- include health and justice representation at national and regional IMT and EPRR arrangements described in Appendix 2
- ensure close working with custodial partners to safeguard against the spread of pandemic infections for this population cohort
- ensure close synergy, collaborative working and robust communications with all relevant partners, including health and justice leads for NHS England, HMPPS, HO, YJB and UKHSA
- ensure good quality and up to date information from HMPPS, HO and YJB regarding the status of the health and justice settings
- ensure the health and justice settings are included in NHS England operational plans for accessing PPE and testing kits
Infection prevention and control (IPC)
Effective leadership and the consistent communication of evidence-based IPC guidance is key in a pandemic response. IPC specialists are an intrinsic part of all NHS England’s response teams and will be integrated within the wider response at all stages and at all levels. IPC specialists nationally and regionally will work together with key stakeholders e.g. UKHSA, devolved nations and DHSC to ensure a co-ordinated and consistent response. Key priorities for NHS England will be to:
- support national/regional IMT/co-ordination centre(s) response, ensuring IPC representation in NHS England decision-making and communication cascade
- develop and support the provision of evidence-based IPC clinical and operational guidelines for the NHS in liaison with DHSC, UKHSA and the devolved nations
- engage with key external stakeholder’s including professional bodies and infectious diseases expertise on pandemic response(s)
- agree, activate, and review relevant situation reports and data
- seek assurance from systems regarding knowledge and application of relevant operational and clinical guidelines including the national infection prevention and control manual (NIPCM)
- provide consistent IPC leadership, working closely with systems and providers to adopt, adapt and scale up implementation of national IPC guidelines
- work with UKHSA and DHSC to agree roles and responsibilities during a pandemic response, identifying any gaps in provision outside core NHS services and agreeing a national pandemic response
- provide an IMT response that includes an IPC cell, linking national and regional governance to ensure effective communication and routes of communication and escalation
Primary care
The focus of primary care planning during a pandemic will be to support public health messaging about self-care and the maintenance of essential services to prioritise patient groups deemed to be most at risk. Where sufficient warning that a pandemic is surfacing and in anticipation of its severity, primary care providers will work to ensure patients are as prepared as possible for a pandemic.
Effective communication across integrated care systems and other local resilience forums will be required to ensure GPs and other healthcare professionals are aware of local capacity in acute, primary and integrated urgent care, and social care facilities.
NHS representation at local resilience forums (LRFs) and borough resilience forums (BRF) should ensure consideration of primary care issues and that strong local communications are established and maintained. Response arrangements across England will therefore not follow a consistent model.
A change in patient health seeking behaviour during a pandemic is likely to see a change in demand for certain treatments. Some may need to be delivered differently, e.g. via telephone, email or video consultation. The range of nurse led services may need to increase or be provided through creating greater autonomy for the wider primary care clinical workforce e.g. professional support which would include ensuring appropriate professional and clinical indemnity, to support professionals working at the margins of their traditional scope of practice, will be discussed at a national level.
The nature of primary care, operating as a relatively small business and employing more part-time/locum workers than other sectors of the NHS, means that a significant outbreak may have a lasting impact on infrastructure. Secondary and community care providers may also experience a prolonged period before resuming normal business (such as fully reinstating cancelled elective programmes) while the system normalises.
The work should also consider how NHS England, as well as the wider NHS, would respond should there be further outbreaks or a subsequent major incident.
NHS 111
Use of and integration with 111/ telephony/ web-based services
Previous outbreaks have shown that NHS 111 and 999 services can be early indicators of any increase in pressure at local level. The rise in call volumes and web-traffic to 111 can correspond with the level of any emerging health alert or pandemic. During September 2012, cold and flu data from NHS111 was showing an unusual and out-of-context/ out-of-season rise in typical cold and flu symptoms for that time of the year.
Considered use of these services can support a response and help mitigate pressure on other areas of the NHS, while providing accessible support to patients and the public.
National coordination of these services should be considered early in the planning and response to any future pandemic. This must be coordinated with DHSC and UKHSA to ensure the NHS can respond.
The nature of the public messaging about a pandemic can disproportionally impact these services (e.g., leading to a high volume of contacts from ‘worried well’ people as well as those who need care) which can overwhelm these services and stop those at most need gaining access to symptomatic support and treatment.
NHS England and the UKHSA will need to prioritise how calls will be answered. It is essential the 999 and 111 services are available for business-as-usual capability as well as responding to those who are unwell as a result of a pandemic. UKHSA is responsible for ensuring call taking staff are available to manage the increased number of calls related to a pandemic to protect the business-as-usual 111/999 priority functions.
NHS England Integrated Urgent Care and Urgent & Emergency Care teams will work together to agree the level of response, in partnership with the operational delivery of this service by UKHSA. This will allow NHS 111 / 999 to manage BAU business while contacts seeking support and advice about a specific health related issue will be managed by UKHSA.
It is anticipated, however, that the public will be directed to NHS 111 as a single point of contact, and that symptomatic callers or pandemic specific enquiries would be re-routed to UKHSA-supported call taking staff. If they required further assessment, they would be routed back to the NHS 111 service.
With digital services now a critical part of a modern healthcare system, the pandemic enabled us to achieve a level of digital transformation that might have otherwise taken several years, and it is critical that we continue to build on the progress we’ve made and ensure that all health and care providers have a strong foundation in digital practice.
Increasing numbers of interactions with citizens could be delivered digitally with the NHS app being used as a simple, single digital front door (incorporating NHS, UK and NHS 111 on-line) helping to shift clinical activity away from face-to-face, except when needed.
This would help to put patients in control of their own health (through national digital channels) by leveraging the power of tailored and contextual information/ communication, improving access to in-home diagnostics (where applicable) and messaging to empower and reassure, change behaviours and potentially improve health outcomes. Self-care, self-refer and effective triage.
Adult critical care
Previous experience has proven that adult critical care services are an important ‘keystone’ service during time of pandemic. During the COVID-19 pandemic, an Adult Critical Care Planning Programme was established, with a remit to improve services and prepare for future emergencies. Support tools for adult critical care service commissioners, providers and clinical networks were developed and released as a result, alongside existing commissioning guidance. These are now embedded across the ongoing commissioning function and include the Adult Critical Care Dashboard and Adult Critical Care Surge Planning Guidance.
During times of increased demand on adult critical care services, in line with the published surge planning guidance, a formal advisory panel is established to support and coordinate local decision making on mutual aid, known as the Adult Critical Care Capacity Panel (or previously the Severe Covid Response Cell).
In addition, there is an adult critical care clinical reference group (CRG) with a National Clinical Director (NCD) situated in the national specialised commissioning team, which supports national standards and guidance on specialised critical care services.
Alongside this there are also approximately 20 adult critical care Operational Delivery Networks (ODNs), covering the geography of services in England, underpinned by a shared clinical network service specification. Upon establishment of any future pandemic emergency response governance structure, consideration should be given as to how the CRG, NCD and the ODNs should be linked in.
Ministry of Defence (MOD)
A military liaison officer (MLO) is allocated to NHS England within the EPRR team. The role of the MLO during a pandemic will be to:
- act as a conduit between the NHS and MOD
- identify the impact on MOD personnel
- ensure effective communication between the NHS and MOD
- identify what support, if any, MOD may be able to provide the NHS including through military aid to the civil authorities (MACA) if appropriate
The MLO will also be a member of the NHS England MACA panel which will be established in the event of multiple MACA requests being submitted. This panel will provide a governance and assurance function, ensuring that requests for military resources are appropriately triaged.
Appendix 4: Resources
Finance and legal
Pandemic related expenditure will be tracked across NHS England and the wider NHS, and the legal protocols underpinning the response are in line with organisational legal responsibilities and frameworks.
Antibiotics
A range of antibiotics have been stockpiled to treat the anticipated secondary complications of a pandemic. These may be useful if secondary bacterial pneumonias are a feature of a pandemic. These are largely for use in secondary care although there may well be some primary care demand. It is intended that antibiotics will be made available through the usual distribution mechanisms, (i.e. NHSSC or through the wholesaler networks). Other medications, like steroids, may become key treatments depending on the nature of the pandemic agent.
Pandemic specific vaccine (PSV)
At the earliest, it is anticipated that a pandemic specific vaccine (PSV) will be available four to six months after a pandemic agent is identified. This will be affected by the causative agent and whether there are any existing vaccines that could be used as a basis for a pandemic vaccine. There will be insufficient vaccine initially to launch a mass vaccination campaign, therefore national prioritisation will be required by DHSC with expert input. It is anticipated that vaccine will be initially offered to people identified as at increased risk through the early months of a pandemic, which will be a significant under-taking. It is anticipated that vaccine will be delivered through primary care and occupational health (for NHS workers) and may be augmented by mass vaccinations services, the stand-up of community pharmacy and vaccination services, and extraordinary arrangements in primary care. The consumables necessary to deliver the vaccine will also be provided.
Testing and sampling
Testing of people suspected of being infected with an infectious agent has been delivered through a variety of approaches in previous outbreaks and pandemics appropriate to local services and populations. These have been supported by NHS commissioners and providers at all levels, and all aim to minimise the impact of suspect patients on members of the public, primary care and emergency departments. The approach to testing will likely evolve over the pandemic as case numbers increase, and as specific test are developed.
Appendix 5: Planning assumptions
The position around planning assumptions currently remains unchanged, in that plans should follow three principles described by DHSC prior to the COVID-19 pandemic:
- precautionary: response should consider high severity risk, including the acknowledgment of the potential severe symptoms experienced
- proportionality: response should align with the known risk; a plan should be implemented for not only high impact pandemics but lower impact scenarios too
- flexibility: there should by a UK wide plan demonstrating consistency but with a degree of flexibility and agility to allow for variation within the transition from one phase to another to align with local levels of infection and pressure on the healthcare system
Although previous arrangements focused on an influenza pandemic, as highlighted in the National Risk Register 2023: “any new pathogen transmitted by the respiratory route is likely to share characteristics with influenza in that it can spread rapidly via close proximity, can travel rapidly and there are few easy immediate countermeasures. It has therefore been a planning assumption that a plan for pandemic influenza would have considerable overlap with a plan for other diseases easily transmitted by the respiratory route”. These reflect a reasonable worst-case scenario (RWCS) regarding impact to healthcare and wider services and the following generic assumptions should continue to aid planning:
- it will not be possible to halt the spread of a new pandemic virus, and it would be a waste of public health resources and capacity to attempt to do so
- the impact and nature of a virus cannot be known until it has emerged and affected a significant number of people, this means that impact predictions are an assumption as opposed to a forecast; the actual impact could be very different to that predicted
- response plans must have a degree of agility and scalability to cope with a range of possibilities and adapt to a wide range of scenarios
- despite the origin of the pandemic, it is likely to reach the UK very quickly, with sporadic cases and small clusters of the disease occurring around the country after only one or two weeks
- the degree of pressure in different areas will vary, highlighting the importance of flexibility within the plan
- while influenza treatments exist, effective vaccines (or treatments for a non-influenza pandemic) are unlikely to be available at the initial stages of response
Appendix 6: Supporting documents
Generic
- NHS Emergency Preparedness, Resilience and Response Framework
- NHS England Incident Response Plan
- NHS England Incident Response Plan Annex A – Protracted Incidents
- CCS’s National Risk Register
- National IPC Manual for England
- WHO checklist for respiratory pathogen pandemic preparedness planning
- Minimum Occupational Standards
Pandemic Influenza
- Pandemic flu – GOV.UK (www.gov.uk)
- The UK Influenza Pandemic Preparedness Strategy (2011)
- Health and Social Care Influenza Pandemic Preparedness and Response (2012)
COVID-19
High consequence infectious diseases (HCID)
Surveillance
Publication reference: PRN01206