This guidance has been produced with:
- The British Association for the Study of the Liver
- The British Society of Gastrointestinal and Abdominal Radiology
- The British Society of Gastroenterology
- The British Liver Nurses’ Association
- Hepatocellular Carcinoma UK
- The British Medical Ultrasound Society
- The British Liver Trust
Purpose
This guidance sets out the minimum requirements to deliver quality surveillance for patients at risk of hepatocellular carcinoma (HCC). It supports hepatology, gastroenterology, and radiology services in tailoring pathways for HCC surveillance, based on their patient populations.
These minimum standards are intended (primarily) for senior staff at NHS providers and clinical teams who have responsibility for setting up and optimising these pathways locally.
For guidance on delivering quality ultrasound for HCC surveillance, please refer to the guidance published on the NHS England website.
Introduction
Liver cancer is the fastest-rising cause of cancer related deaths in the UK. The most common form of primary liver cancer is hepatocellular carcinoma (HCC), which makes up 85% of all liver cancers.
According to Cancer Research UK, around 6,200 people are diagnosed with liver cancer each year. Incidence of HCC has increased by 50% over the past decade and is expected to continue to rise. Existing evidence suggests that only around 20% of HCCs are currently diagnosed at an early stage (stages 1 or 2).
Research by the British Liver Trust suggests only 13% of people will survive 5 years or more following a liver cancer diagnosis, and only 40% will survive for 1 year or more.
Survival and patient outcomes from HCC are significantly improved when the cancer is diagnosed earlier. The biggest risk factor for HCC is pre-existing liver disease, with liver cirrhosis being present in 80-90% of people with HCC.
National Institute for Health and Care Excellence (NICE) guidance recommends that people at high risk of HCC (those with hepatitis B and/or cirrhosis) receive 6-monthly liver surveillance (NG50, CG165, CG115). And while guidelines from NICE and the European Association for the Study of the Liver recommend HCC surveillance, fewer than half of patients who should receive surveillance actually do.
On average, patients in regular ultrasound surveillance have their cancers detected earlier and receive more curative intent treatment.
However, implementation needs to be improved. To this end, this guidance sets out the basic requirements to deliver quality surveillance programmes to support earlier detection of HCC.
What is hepatocellular carcinoma surveillance?
Hepatocellular carcinoma (HCC) may be asymptomatic until it has reached an advanced stage.
Regular 6-monthly surveillance of adults with cirrhosis or advanced fibrosis and conditions including hepatitis B and hepatitis C (as set out in the eligibility criteria below) increases the chance of detecting HCC early so that patients can benefit from potentially curative treatment, and improved chances of survival.
Principles of hepatocellular carcinoma surveillance
- Patients suitable for hepatocellular carcinoma (HCC) surveillance should be invited to 6-monthly ultrasound scans.
- Ultrasound scans should be performed by an appropriately trained sonographer or radiologist.
- Alpha-fetoprotein (AFP) can be considered as part of HCC surveillance, unless there are patients not suitable for blood testing.
- Surveillance leads should regularly audit their service and compare outcomes with comparable services. This will also include:
- establishing targets for performance, compliance and clinical outcomes (for example, invites sent, attendance to ultrasound appointments, HCC diagnoses and stage of diagnosis)
- appropriately coding patients as under HCC surveillance.
- Services should be established in a way to maximise compliance. This should include:
- a digital system to track and call-recall patients for ultrasound appointments
- (where appropriate) coinciding surveillance scans and appointments with other liver disease assessments and appointments
- attempting at least 2 different forms of communication to invite patients to ultrasound surveillance appointments
- the use of pathway navigators and peer support workers
- Information on the purpose, benefits and limitations of surveillance should be provided to all patients.
- Patients should promptly receive and be provided with an explanation of their ultrasound results.
Eligibility criteria
With a growing array of effective treatments, all patients with early-stage cirrhosis who would be fit for and benefit from treatment should be offered enrolment into liver surveillance.
The following patients should be offered enrolment in hepatocellular carcinoma (HCC) surveillance:
- Child–Pugh stage A
- Child-Pugh stage B patients based on an individual assessment (for example, controlled ascites)
- Child–Pugh stage C patients with cirrhosis, awaiting liver transplantation
- patients with hepatitis B and significant fibrosis or cirrhosis (≥F2-4)
- patients with hepatitis B without significant fibrosis or cirrhosis with a family history of HCC
- patients with hepatitis B and hepatitis D coinfection
- patients with hepatitis C and advanced fibrosis (≥F3)
- patients with haemochromatosis and advanced fibrosis (≥F3)
- patients with other liver diseases where the individual has a high risk of HCC.
The above criteria set a minimum standard for patients who should be offered HCC surveillance. Providers may choose to offer HCC surveillance to additional patients in line with local protocols, but these protocols should be published and implemented consistently.
Exclusion criteria for hepatocellular carcinoma surveillance
Surveillance is not recommended in patients who are not fit for cancer specific therapy.
Examples include:
- those with decompensated cirrhosis who would not be candidates for liver transplant if hepatocellular carcinoma was diagnosed (Child-Pugh B8 or worse)
- those with very impaired performance status (Eastern Co-operative Oncology Group [ECOG] category 2 or World Health Organization Performance Status [WHO PS] or worse).
Patient tracking
Data capture
A local secure database or tracking system should be in place to hold a list of patients requiring hepatocellular carcinoma (HCC) surveillance.
These patients should be assigned a locally agreed code such as ‘USS (ultrasound scan) HCC surveillance’ or the appropriate labelling in their medical records.
This will enable services to track the number of patients actively receiving surveillance and support requests for ultrasound that are specific to surveillance.
Services should agree what data will need to be collected, but as a minimum the tracking system should support services to:
- capture all patients suitable for surveillance into a single list
- understand who is due their 6-monthly ultrasound scan and highlight who has/has not been invited
- capture who has attended/not attended their 6-monthly ultrasound scans
- capture patients who have declined surveillance and the reasons for this
- referral timelines, for example to HCC multidisciplinary team
- HCC diagnoses
- stage of HCC diagnoses (Barcelona Clinic Liver Cancer [BCLC] staging system)
- treatment outcomes.
Ultrasound imaging should be requested with the appropriate codes:
- NICIP USRLV
- SCT-ID 990271000000107
Call/recall systems
Services need a digital (ideally automated) system in place to call/recall patients for surveillance appointments and scans.
Services should move away from Excel spreadsheets to a secure database to hold patient lists as stated above. This includes having a way to assess and monitor patients referred for hepatocellular carcinoma surveillance.
Where standard digital systems are used (no automation function) – for example, PACS or other radiology systems – the appropriate admin support should be in place to call/recall patients.
Patient information
Patients enrolled into a surveillance programme should have information on the purpose of surveillance, its aims, and its limitations.
This can be supported by the hepatocellular carcinoma (HCC) surveillance animation and postcard, developed in partnership between NHS England and the British Liver Trust. Free copies of the HCC surveillance postcard can be ordered on the British Liver Trust website.
Further support will be provided by other resources developed by HCC surveillance providers.
All patient information should be available in easy read versions and in different languages tailored to your local populations.
Services should ensure patients are aware that they can opt out of surveillance; and should have a way to record this within the system being used to track patients.
It should also be possible for patients to change their mind. Systems will need to be updated to reflect this.
Supporting attendance
Significant challenges remain in identifying patients at risk of hepatocellular carcinoma and maintaining them in surveillance programmes, particularly those with a history of frequent drug or alcohol use, or who are experiencing homelessness.
Services should consider setting targets for attendance that are realistic but aspirational.
The NHS Cancer Programme’s Early Diagnosis of Liver Cancer Programme is aiming to support liver services invite >80% of patients with cirrhosis or advanced fibrosis (and meet the eligibility criteria, above) to 6-monthly ultrasound surveillance and support >60% of those invited to attend.
To support attendance, services should:
- understand the barriers to engagement from patients and take appropriate action to counter these (for example, changing location or timing of scans)
- provide all patients with full information on the purpose, benefits and limitations of surveillance – in clinical appointments and then followed up by written communication, to allow patients to make an informed choice about whether to attend
- invite patients to ultrasound using at least 2 different forms of communication
- the second should involve personal contact, for example a phone call
- writing to patients alone is not enough due to the different communities being contacted, many of whom will not have fixed addresses
- provide patients with their ultrasound and blood tests results promptly; and where possible, give/show their results so patients are actively able to lead their care
- (where appropriate) coincide surveillance scans and appointments with other liver disease assessments and appointments to prevent multiple hospital appointments/trips
- organise nurse-led surveillance with consultants seeing more complex patients
- use trained peer support workers and/or pathway navigators to support clinical teams
Pathway navigators and peer support workers can provide additional support to clinical teams by contacting patients frequently, providing information about their appointments in a way they are likely to engage with, and even providing transportation services to patients.
The job descriptions for these roles can be viewed on the NHS England website.
Diagnosing hepatocellular carcinoma
Ultrasound can detect large hepatocellular carcinomas (HCCs) with high sensitivity and specificity. However, detection of lesions below 2cm by ultrasound is more difficult. Combining alpha-fetoprotein (AFP) with ultrasound improves detection rates, therefore services should consider AFP.
Ultrasound can detect abnormalities that may require further investigation with cross sectional imaging.
Detailed guidance is available on the NHS England website on delivering quality ultrasound surveillance for patients undergoing HCC surveillance.
A dedicated hepatology/gastroenterology and cancer multidisciplinary team should be in place to discuss patients who may need to be referred via the faster diagnostic standard, once all necessary imaging has been completed.
Figure 1: patient pathway
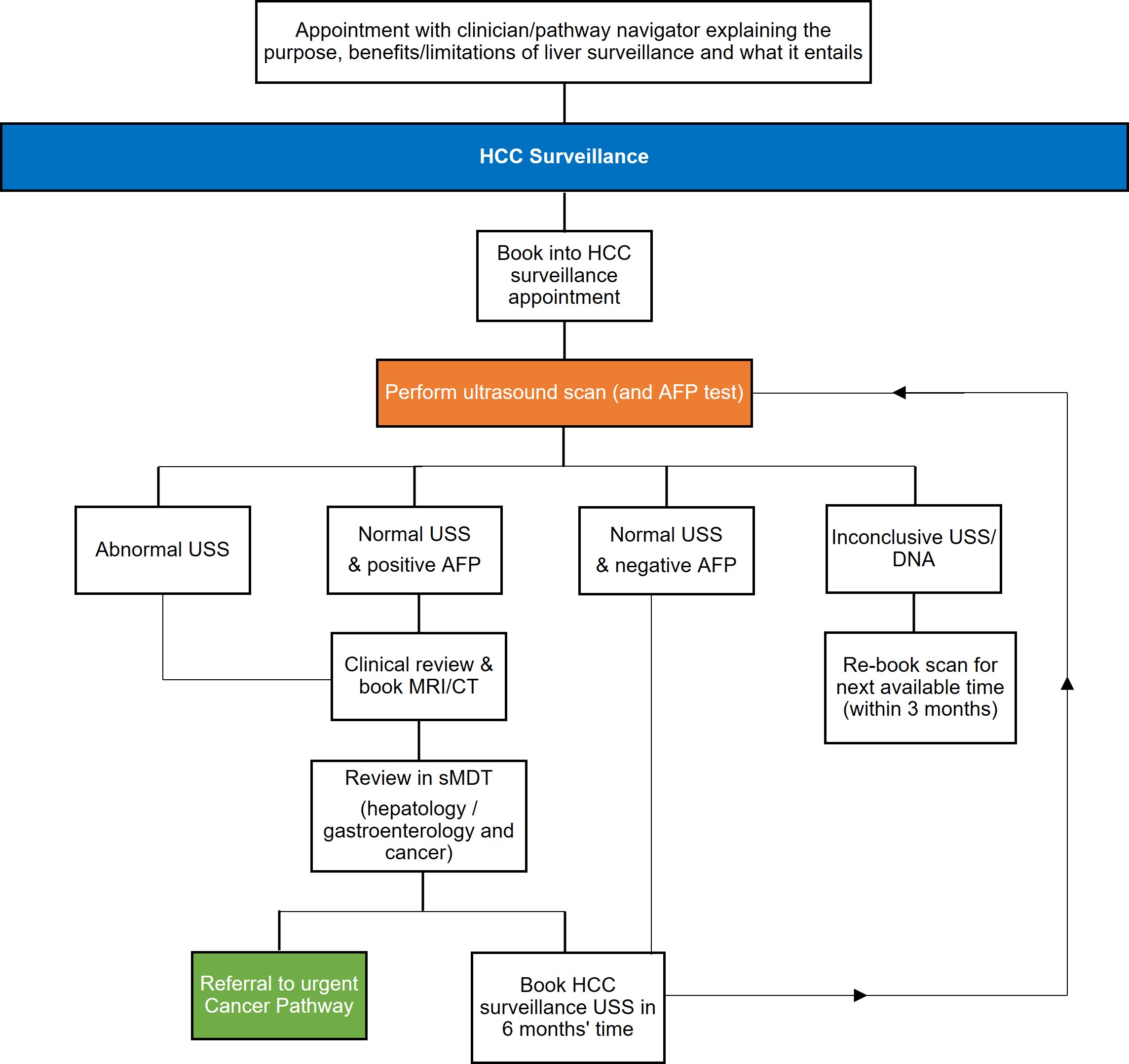
Figure 1 above is the patient pathway for hepatocellular carcinoma (HCC) surveillance. The sequence follows a pathway from enrolment in HCC surveillance and the onward journey once ultrasound has taken place.
Initially, a patient is booked into an HCC surveillance appointment. At that appointment the patient receives an ultrasound scan (and an alpha-fetoprotein [AFP] test) and the result of this determines the next step in the pathway. If an abnormal ultrasound (US) result is found, or a normal US result and positive AFP result, the patient is booked into a further clinical review and MRI/CT appointment and the results are reviewed in sMDT. Based on this the patient is either referred onto an urgent cancer pathway, or booked into another HCC surveillance US in 6 months’ time.
If a normal US result is found and a negative AFP, the patient is booked into an HCC surveillance US in 6 months’ time.
If an inconclusive result is found or the patient DNAs then the scan is rebooked for the next available time (within 3 months).
Acknowledgements
- Clinical representatives: Aloysious Aravinthan, Benjamin Stenberg, Aileen Marshall, Coral Hollywood, Douglas McDonald, Graham Foster, Ian Rowe, James Franklin, Janisha Patel, Katharine Caddick, Rebecca Jones, Rohini Sharma, Stuart McPherson, Vanessa Hebditch and Tim Cross.
- Operational representatives: Joanna Strickland.
- Patient and charity representatives: Monica Walsh, Vanessa Hebditch and the NHS Cancer Programme.
Publication reference: PRN01248

