Introduction
Modern general practice and improving care related processes
The pressures on general practice teams remain high. NHS England has committed to reducing practice administrative burdens, in part through encouraging self-service and self-referral where appropriate by patients and through integration and automation of some practice processes.
This guidance offers information on three important care-related activities (workload that pertains to a patient but does not directly involve them):
- prescription management
- long-term condition recalls
- new patient registration.
In addition, it also offers improvement approaches which can be applied to a wider range of tasks and processes.
Improving key care-related activities can deliver multiple benefits:
- safer higher quality care
- improved patient experience
- time saved, freeing up headspace for other activities and considerations
- cost savings
- increased staff satisfaction
- evidence for regulatory activities e.g. Care Quality Commission (CQC)
- achievement of certain Quality of Outcomes (QoF) indicators
Section 1: using a quality improvement approach
Any improvement or change activities need to be underpinned by a robust structure and framework for implementation, including:
- having a clear aim or vision for what you are trying to accomplish
- undertaking process mapping
- taking and understanding baseline measurement
- continually testing and measuring improvements to know when a change has led to an improvement
- sharing outcomes and learning
There are several quality improvement approaches that are used across health and care settings:
- The Model for Improvement: How to Improve: Model for Improvement | Institute for Healthcare Improvement. A summary of the model is shown in section 5.
- The Change Model for Health and Care: Change Model | NHS England. A summary of the model is show in section 5
- A four-step approach to care-related activities: a summary of this approach is described in section 5.
These methodologies can be used when looking at three specific care-related activities:
- repeat prescriptions management
- recalls for long-term condition management
- new patient registration
However, they are applicable to any improvement you make within a care-related setting or any other change project within healthcare.
Section 2: improving prescriptions management
Patients are now able to order repeat prescriptions digitally (via the NHS App and other patient facing service apps).
This repeat prescription request can be passed to the core practice system digitally and be reviewed and approved and sent to pharmacy digitally.
Moving patients where possible and appropriate away from requesting their repeat prescription via paper slips, telephone ordering and online forms brings considerable benefits to patients and general practice.
Benefits for patients
Ordering through the NHS App or another equivalent app means they:
- can order when it is convenient
- only have to tick the box to indicate the medications they require.
- reduce the risk of errors from entering complicated names and dosages or unclear ticks on paper slips
- are kept informed of the progress of their prescription
- have greater flexibility and ability to change (temporarily) their nominated pharmacy – e.g. if away on holiday
Benefits for practices
Encouraging patients to order repeat prescriptions through the NHS App or another equivalent app means:
- administrative staff do not need to enter the information manually, releasing administrative time
- the prescription request is linked to the electronic prescribing system to help clinicians to complete/manage the request more easily
- improved prescription accuracy reduces the chances of patients receiving the wrong medication
- a full audit trail is created so prescriber and dispenser can track where prescriptions are
- patients are kept informed of the progress of their prescription, reducing calls to the practice
- gives practice teams greater control over prescription and medicines management
Encouraging patients to order repeat prescriptions via the NHS App
When devising a plan to encourage patients to consider and to try ordering repeat prescriptions via the NHS app or other equivalent apps it can be helpful to use one of the quality improvement approaches described in section 1.
For example, using a plan-do-study-act (PDSA) cycle can help plan how to achieve this goal and how to keep improving the process to further increase the benefits to patients and staff in general practice.
The PDSA cycle starts with creating a plan.
The first part of planning is agreeing the objective. Start by identifying all the different ways patients can currently order repeat prescriptions, they might include:
- using the NHS App or other apps
- walking in and completing a repeat prescriptions form in reception
- dropping in or posting a paper prescriptions slip
- calling the practice and ordering over the phone
- completing a repeat prescriptions form on the practice website
Decide which you want to encourage, which you want to discourage or stop (and when you will stop them by).
Once you have agreed your objectives you can create a plan for achieving this. This will include:
- creating the right messages and communications: update messaging on the phone system and website and prepare posters and text messages to patients to raise awareness, communicate benefits and explain how to order via NHS App (and what to do if a patient needs help).
- how we will offer and provide help to patients to switch to the NHS app using patient liaison or social prescribing link workers
- briefing the practice team on the plan and with conversation points which explain the benefits to patients and to the practice of ordering prescriptions via NHS App.
- how to use your practice system to segment your patients into different groups who might need different messages. Who currently orders repeat prescriptions on channels other than via the NHS App or other apps.
- how and when we will communicate with patients regularly emphasising the key messages and benefits to them (and thank patients for helping the practice too)
- how and when we will encourage patients to nominate their local pharmacy
- how we will regularly measure the number of patients using the NHS App (or other equivalent apps) to order repeat prescriptions compared to other ways and what percentage of overall prescriptions are ordered via the NHS App (or other equivalent apps).
Once you have finalised your plan, you can set a date for when you want to start (the ‘do’ part of the PDSA cycle).
Make sure you set a regular point (for example monthly) to ‘study’ the data about the percentage of patients using the NHS App to order repeat prescriptions and the percentage of repeat prescriptions being ordered via NHS App. This allows you consider any changes or improvements you might want to make to your approach.
Smoothing back-office prescription processes
As well as encouraging patients to order repeat prescriptions via the NHS App or equivalent app, practices can also use the same quality improvement approaches to smooth back-office processes to help release staff time and reduce practice burden.
Areas practices might consider include:
- using a skills matrix an example of which can be found on the General Practice Improvement Programme website, to help understand who in the team is trained to manage prescription requests and identify where further training is required
- aligning patient medication review dates
- introduce repeat dispensing where this is clinically appropriate. Benefits are particularly seen for those patients with stable conditions and medications e.g. Levothyroxine, and align their medication review to long term condition checks
- work closely with local pharmacies around changes being undertaken (reducing unnecessary calls, emails etc)
- for patients who choose not to use the NHS App to manage their medications, look to optimise other digital channels (e.g. practice websites) to improve their ordering experience and streamline their requests to an appropriate workflow
Primary Care Networks and prescriptions working at scale
Primary Care Networks (PCNs) provide an opportunity for practices to collaborate in a wide variety of ways including:
- using a prescription hub across the PCN as a single point of service for prescription requests. This can help to simplify and streamline services. Using pharmacists and pharmacy technicians to run the hub can allow medication reviews to be undertaken and improve safety
- sharing protocols and processes for management of repeat prescriptions to develop consistency of approach
- using a Primary Care Network clinical pharmacist to work across practices to share learning and gain consistency of approach.
Section 3: improving recalls for long-term condition reviews
Long-term condition (LTC) reviews are a key element in supporting patients with long term conditions.
The volume of administrative tasks related to long-term condition management can be significant for many practices.
Practices can use the quality improvement approaches listed in Section 1, for example the plan-do-study-act (PDSA) cycles to improve recalls for long-term condition reviews.
Recalls for LTC reviews can be further enhanced using existing digital tools to reduce practice workload and improve the efficiency of long-term condition management.
Designing a reliable process for long term condition management
A reliable process for long-term condition review should include the following elements:
- reliable recall process (including management of non-response – minimum of 2 calls for care within 12 months using the patient’s preferred contact method)
- standardised care process for both patient and practice, involving minimal practice visits/contacts in the correct order to optimise care without creating failure demand
- unification of medication review and LTC review processes
- equitable spread of activity across the year e.g. using birthday month recall (avoiding Q4 panic to achieve QOF or generate high levels of personalised care adjustments)
- making full use of multi-disciplinary team and involve all staff and patients in the design of new processes
- encouraging patient responsibility for health and well-being/management of their LTCs
- consider a personalised care approach to LTC management with use of shared medical appointments, social prescribing and digitally enabled self-management depending on patient choice and need.
Use of technology to support modern long-term condition management
The management of these tasks can be supported by good process and effective use of modern messaging, appointment tools and a wide range of medically approved digital health questionnaires via online consultation tools.
These enable administrative teams to:
- gather information asynchronously to navigate and risk stratify patients based on urgency of review and continuity needs, identify need for tests prior to review, identify specific requirements for the appointment e.g. booking an interpreter or reminding the patient to bring a urine sample to their diabetes review
- request more detailed information from patients prior to review
- invite patients to self-book an appropriate appointment
- send appointment reminders
- record responses and health questionnaires directly into the patient record
- record responses to meet QOF requirements
The use of well-integrated modern messaging and booking tools and digital health questionnaires can reduce administrative time, increase response rates and reduce errors. Some of these tools can also support self-booking of appointments and fully integrate into the clinical system.
The Digital Care Services integrated framework will make available assured online consultation, messaging and appointment booking tools to practices from autumn 2023. If you would like more information or support about online consultation, messaging and booking tools please contact us at england.pctgpip@nhs.net.
Measuring and continuing to improve long-term condition management
As part of the improvement process it is important to continually test and measure that the process is safe and reliable, that patients are not missing reviews and there are no unforeseen errors.
Also look at patient and staff satisfaction metrics alongside measuring progress with your recall system within your long- term conditions pathway management.
Continual improvement of these pathways could involve looking at where at scale delivery may support management of these conditions for example at a Primary Care Network or neighbourhood footprint, or further develop the digital self-management model described above.
Section 4: improving new patient registration
For some practices new patient registration can be a time-consuming task especially for practices receiving high volumes of new patient registrations.
These high volumes can be across the year or concentrated into short time periods, for example at practices serving universities and colleges at the start of the academic year.
Practice admin teams in research told us that registrations can take between 5 and 15 minutes to process, however in some circumstances could take up to 30 minutes. This time is particularly dependent on whether they are entering paper forms, whether there’s a requirement to check catchment eligibility and whether the patient is easily matched to a record on the spine.
In recent years the NHS has invested in a national Find a GP service and national How to register with a GP surgery patient registration service to make it easier for patients to register online.
In addition, a variety of technology suppliers also provide tools to automate most new patient registrations, some of which are participating in the national registration scheme.
If you would like more information about automating new patient registration, please contact us at england.pctgpip@nhs.net.
Benefits of online patient registration
For patients:
- easy to find practices open to registering new patients
- easy to find practices open to registering new patients outside their catchment area
- no need to visit the practice to collect paper forms or download/print at home
- can be completed at a time of the patients choosing
For practices:
- (using national pilot) when the registration form is received digitally it reduces transcription errors compared to when handwritten paper forms are entered into the practice system
- (using national pilot) when the registration form is received digitally it reduces unmatched patients / spine matching errors as the patient is checked against the spine as part of the process
- (if using additional automation) can be directly ingested into the practice system, no need to rekey patient information
- (if using additional automation) can be automatically matched to the spine, no need to manually search
- (if using additional automation) can be automatically registered and patient notified, no need for manual review and notification to patient
All these benefits combined can release significant amounts of administrative time especially for practices receiving high volumes of new patient registrations.
Increasing online new patient registrations
When devising a plan to increase the percentage of new patients who register online (and potentially automate some or all the back-office registration tasks) it can be helpful to use one of the quality improvement approaches described in section 1.
For example, using a PDSA cycle can help plan how to achieve this goal and how to keep improving the process to further increase the benefits to patients and staff in general practice.
The PDSA cycle starts with the objective and creating a plan to achieve this.
To create a plan for increasing online new patient registrations you will need to:
- map the existing process
- review the new patient registration journey on your practice website
- consider if using an automation tool for back-office registration processes would be helpful
- review pre-prepared (canned) messages sent to patients about registration
- brief practice staff
- consider how collect data on the percentage of new patient registrations received online compared to paper and what changes you might need to make to your plan.
Map the existing process
- map out the ways in which a patient can find information about how they can register as a new patient
- map out the steps a new patient needs to take to apply for registration
- map out the steps practice administration staff must take to review, query, clarify, match and register a new patient
- map out how a new patient will know they have been accepted (and provided with information about the practice and how to use the service)
- consider how many patients the practice registers in a year. Does the volume of new patient registrations at the practice warrant the set-up effort and ongoing cost of using the national registration pilot and/or using a tool to automate some or all the back-office processes
New patient registration journey on the GP practice website
A good patient experience on the GP practice website is critical. It should help the patient find the relevant page easily:
- set a homepage call out ‘new patient registration’ that links to a page with information about how to register with the practice
- check the website search box. Does it link to the right page when you enter ‘join the practice’ ‘new patient’ ‘registration’ and other similar terms
When the patient is on the correct webpage, that should provide information about options to register, how to check eligibility and the option to apply online.
You can use ‘Register with the practice’ written content. This has been tested with patients in user testing for ease of use and clarity. It also meets the NHS recommended reading age.
Creating pre-prepared responses about new patient registration
Prepare canned messages (pre-written responses) that can be texted or emailed to patients enquiring about new patient registrations.
This should include links to the new patient registration pages (where patients can register online).
Automation tools for new patient registration back-office tasks
If a practice processes higher volumes of new patient registrations a tool that partially or fully automates the back-office processes may offer significant staff time savings and other benefits.
There are multiple tools offering full or partial automation of patient registrations and which use different approaches to achieve automation.
If you need help identifying options to explore, please contact us at england.pctgpip@nhs.net.
Questions a practice should ask of a supplier include asking if the tool:
- offers the ability for adults, child and proxy registrations
- provides patients with a highly usable and accessible user journey which aligns with NHS design standards. Does written content in the journey meet NHS Content Style Guide requirements and has it been tested to meet the NHS recommended reading age of 9-11 years old?
- enables the Practice to customise the question set to ask for additional information beyond the GMS1 requirements
- automatically ingests the registration document directly into the core practice system (i.e not into the NHS mail inbox where it must be re-entered by practice administrative team)
- automatically matches the patient details to the spine or offers relevant matching suggestions
- enables the practice to choose to switch the system to semi or fully automated mode, where registrations can be received, matched and registered end-to-end
- enables the practice to set ‘rules’ about which registrations they wish to manually review.
- enables the practice to automatically notify the patient they have been successfully registered with the practice
- how much does the service cost and is there a minimum contract term or minimum usage fee (so the practice can consider value for money against the potential time savings)
Staff training
Once you have developed a plan and reviewed the new patient registration journey on your practice website it’s important to engage and brief the whole practice team.
It is important that all staff understand the new patient registration process and it’s benefits for patients and practice staff so that they can answer questions and direct patients to the online registration process.
It is important to explain what support or alternative options are available for patients who are unconfident or unable to use online registration.
Therefore, it is crucial to:
- brief the reception/first contact team
- have the prepared messages to hand
- develop a frequently asked questions document for reference
Measure and improve
Record each month the total number of new patient registrations and the channel by which they arrived (and the % arriving by each channel), either:
- on paper forms
- forms attached to email or messaging
- received digitally
- received digitally and processed automatically
Review progress monthly and consider whether any further changes are required.
Section 5: improvement approaches for care-related activity
The preceding sections looked at specific care related activities and offered, within an overall approach, a set of structured activities that you could undertake to utilise technology to support patients to self-serve, therefore improving processes and reducing elements of practice workload.
The methodology could be used across any activity within the practice and could equally be applied to any care-related activity.
Care-related activity is workload that pertains to a patient but does not directly involve them, for example:
- document management
- test results
- prescription requests and queries
- LTC management (risk stratification and continuing care recalls)
- high risk drug monitoring and recalls
- referrals (including Advice and Guidance requests)
- medication reviews/optimisation
- tasks
- insurance reports
- fit notes
- patient registrations and deductions
- liaison with other organisations regarding patient care, e.g. interpreters, secondary care, community services
Principles of improving care-related activity
It is neither advisable nor practical to work on improving all these processes at once. Start with the processes that take the most time, feel the least stable, or create the most disgruntlement for staff and/or patients.
To achieve transformational, sustainable change in care-related activity, or when undertaking any quality improvement endeavour, we recommend several complimentary approaches.
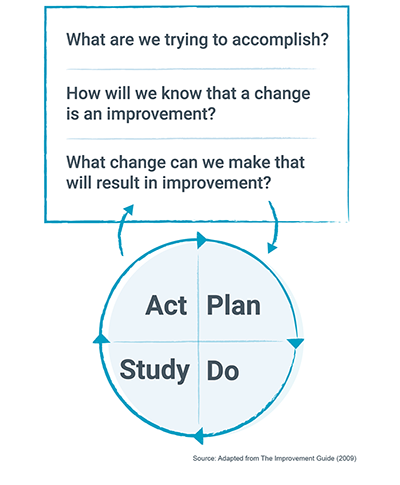
Model for improvement
Figure 1: Model for improvement. Source: How to Improve: Model for Improvement | Institute for Healthcare Improvement
Setting aims: the aim should be time-specific and measurable; it should also define the specific population of patients or other system that will be affected.
Establishing measure: teams use quantitative measures to determine if a specific change actually leads to an improvement.
Selecting changes: ideas for change may come from those who work in the system or from the experience of others who have successfully improved.
Testing changes: the PDSA cycle is a shorthand for testing a change in the real work setting – by planning it, trying it, observing the results and acting on what is learned. This sis the scientific method adapted for action-orientated learning.
Change model for health and care
Figure 2: The change model for health and care
The change model consists of eight components:
- Our shared purpose: Create a sense of shared understanding by involving all stakeholders in a conversation around the improvement you are hoping to make. Do this before anything else. Involve staff and patients wherever possible.
- Leadership by all: Quality Improvement is a team activity, not a solitary endeavour. Best progress will be made when all involved have a sense of ownership and are encouraged to lead, be it in small ways (articulation of the vision, demonstrating positive behaviours, supporting others) or larger ways (organisation, finance, transformation).
- Motivate and mobilise: In order to engage the wider practice team with changes to processes.
- System drivers: It is important to think through what problem that you are trying to fix, what are the reasons for changing and the incentives supporting delivering the outcome.
- Measurement: You need to focus on measurement it is important to know whether progress is being made on the processes we follow and the impact that is expected.
- Project and performance management: To ensure that the changes planned get delivered it is important to have ways of making sure that the change is happening and early warning systems for any problems.
- Improvement tools: Evidence suggests that using evidence-based improvement tools improves the likelihood that a change programme will be successful.
- Spread and adoption: It is important to look at good practice from elsewhere and to share what is going well for us, this builds momentum locally as well as sharing what works well with others.
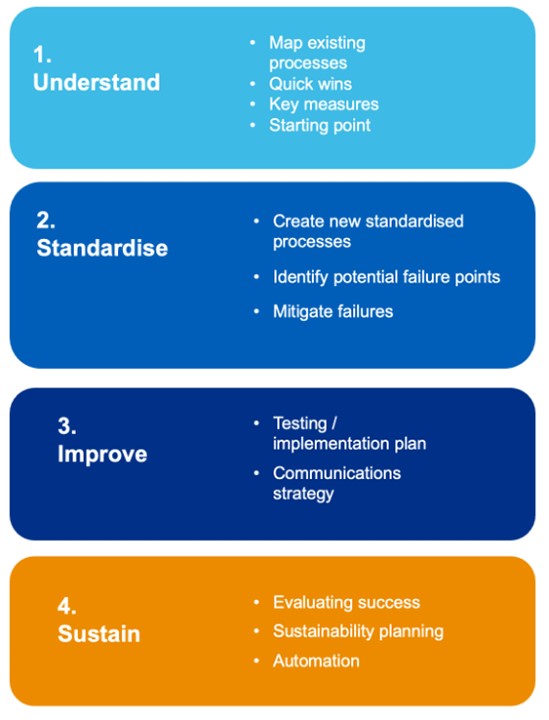
Four stage process for creating and implementing improved care-related activity
Figure 3 – Four stage process for creating and implementing improved care-related activity
Improving the efficiency of processes underpinning the elements of care-related activity requires a process.
This approach has four steps which focus on understanding the problem, through to how to put sustainable, evidence-based solutions in place.
Step 1: understand
The first step within the process is to fully understand and define the problem that is trying to be solved, undertake a range of activities that give an understanding of the current process, and where to focus, or test areas of improvement.
Activities that could be undertaken are:
- measure the demand for the service, understand the current capacity and all the activities associated with the service
- undertake process mapping of the current way the process is delivered, please see this guidance from the Quality Service Improvement and Redesign online library Guide to process mapping
- analyse the process map and identify tasks that do not add value, or could be a bottleneck within the way the current service is delivered
- conduct a Root Cause Analysis (Ishikawa/Fishbone) to fully explore the causes of any specific issues that have arisen from the process map – this teases out effects of variation or imperfection in the current processes and can be grouped into themes. This video from The Institute for Healthcare Improvement (IHI) explains more about how to do this
- using the above processes might lead to identifying some quick wins that you can implement and measure
- define set of measures that cover inputs, process, output and outcome measures along the process you have, giving a baseline
Step 2: standardise
This step starts to redesign the new process, reducing variation within the process, looking at technologies that can reduce the manual processes and build the to be process.
Key elements of this are:
- involve staff and patients in designing the new process, be aware that these are the customers, their voice is crucial to improving the process
- pay attention to being equitable and inclusive in the future design of the process
- map the new process and draft standard operating protocols or procedures
- train staff in the new process and take active feedback from users as part of this process
Step 3: improve
This step helps iterate the process and involves fully testing and implementing improvements as you learn and refine from testing.
Fully test the new process and walk through each step:
- analyse the process and technical solutions at each step of the process and how they integrate with users
- identify potential failures and review the process if failures in the process occur
- design steps to mitigate these failures
- produce final tested process ready for implementation
Develop Communication and Engagement plan
This needs to consider a range of audiences, wider than the practice staff, think through the links with secondary, community, patients and use all channels to ensure the process is robust and all elements have been considered.
Ensure safe and reliable processes
Whenever processes are designed, the approach must be to make the process as safe and reliable as possible. The design approach is to reduce the errors within a process, therefore preventing failures, in a continuous improvement cycle. The model below indicates our approach to preventing failures when designing a process.
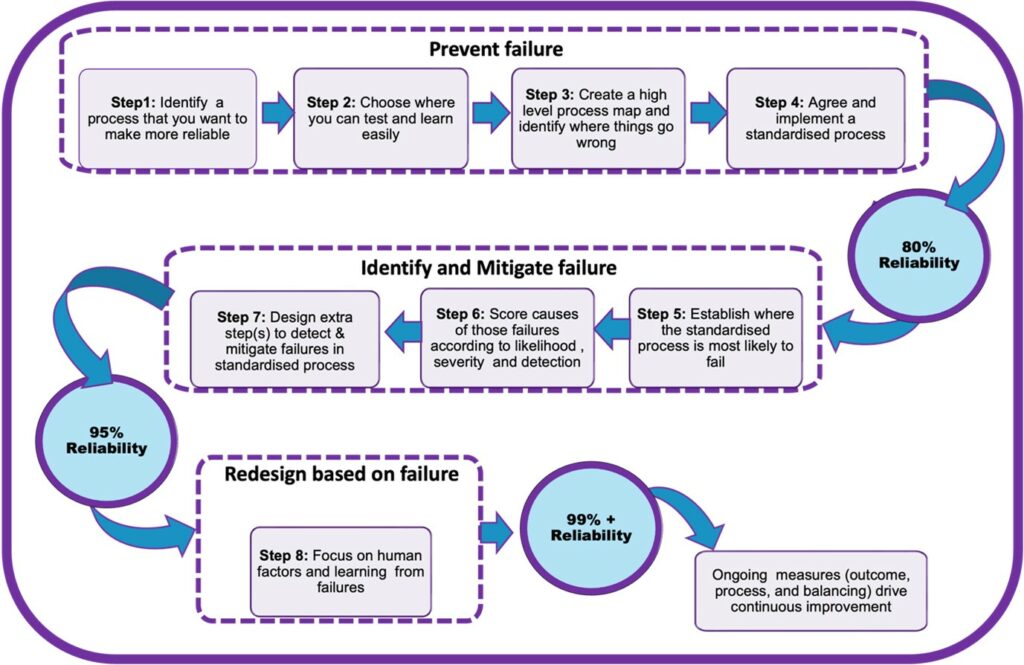
The image is a flowchart describing a process with six main steps.
The steps in the flowchart are – prevent failure: step 1: identify a process that you want o make more reliable; step 2: choose where you can test and learn easily; step 3: create a high level process map and identify where things go wrong; step 4: agree and implement a standardised process. Identify and mitigate failure – step 5: establish where the standardised process is most likely to fail; step 6: score causes of those failures according to likelihood severity and detection; step 7: design extra step(s) to detect and mitigates failures on standardised process. Redesign based on failure – step 8: focus on human factors and learning from failures.
Reliability percentages indicated are: 80% after step 4; 95% after step 7 and 99% after step 8.
Ongoing measures contribute to continuous improvement.
Step 4: sustain (including automation where possible)
Within this step the new process will be live and the key tasks will measure the improvement and impact of implementing the solution.
Ongoing measurement of the process is key, it is important to have a balanced set of measures that can also identify unintended consequences. Some examples of measures could be:
- reduction in phone calls
- staff experience
- patient experience
- reduction in complaints
- improved safety
Ensure there is a robust process for evaluating and acting on the ongoing learning.
Review and build strategic plan around further potential automation of the tasks (Use of current technology or improving Robotic Process Automation) and how the process might be scaled.
How to improve care related processes in general practice
Bakhai M, Vallely D, Fox Z, Joyce J, Silk M
This guidance was prepared by NHS England’s Primary Care Transformation team as part of the national General Practice Improvement programme.
If you have any questions or would like to send feedback, please get in touch: england.pctgpip@nhs.net.
Publication reference: PRN00615_iii