Introduction
Modern general practice and telephony
High quality, effective telephony and online journeys are key enablers of a modern general practice access model. They should integrate well with and support care navigation and administrative processes within a practice or primary care network (PCN).
This guidance helps practices and PCNs choose, purchase and optimise the use of advanced cloud-based telephony.
This guidance is 1 of 5 modern general practice ‘how to’ guides’. The other four guides focus on:
- How to align capacity with demand in general practice
- Creating highly usable and accessible GP websites (includes sections on integrating with the NHS App and encouraging patients to use online channels)
- How to improve telephone journeys in general practice
- How to improve care related processes in general practice
These are all available via the resources page of the national General Practice Improvement Programme.
The national General Practice Improvement Programme (GPIP) provides a range of ‘hands on’ support offers to practices, primary care networks (PCNs) to help move to a modern general practice model. Skilled facilitators work with practices to help map out their model, to analyse and interpret their own data and to support them with improvements.
Why high-quality telephone journeys matter to patients
Since 2021 there has been a sharp drop in patient satisfaction with accessing care through general practice, especially by telephone.
- In the 2023 General Practice Patient Survey (GPPS) 54.4% of patients said they had a good overall experience when making an appointment. This is down from 70.6% in 2021 and down by 1.8 percent since 2022 (56.2%).
- Of patients who had tried, around half (49.8%) in 2023 said it was easy to get through to their GP practice on the phone, a decrease of 17.6 percentage points compared with 2021 (67.6%) and a 2.9 percentage decrease from 2022 (52.7%).
- Around in 8 in 10 (82.2%) in 2023 said the receptionists at their GP practice were helpful, this is a 6.5 percentage point decrease from 2021 (88.7%) and 0.1 percentage decrease since 2022 (82.1%).
- 1 in 5 people report they did not get through or get a reply when they last attempted to contact their practice [Department of Health and Social Care pulse-check survey, December 2022].
Long waits, lack of information, no appointments, no choice of accessing appointments and having to call back another day all impact the quality of the conversations when patients do get through to speak to someone. These are all frustrations faced by patients calling their practice. Further information is available in the Patient Experience Library (Healthwatch Sussex September 2022, Healthwatch Barnsley July 2022, Healthwatch)
The benefits of well-integrated telephone journeys
The use of cloud-based telephony (and improved online journeys) alongside optimised care navigation and triage, understanding and better aligning capacity to demand can help:
- smooth the 8am rush and other peaks throughout the day
- reduce call wait times including giving patients the option of ‘call back’, improving patient satisfaction and experience
- support equity of access across all channels as part of an integrated care navigation model
- reduce the burden on practice teams through integration and easy view data dashboards to support demand and capacity planning and through recording functions, which save time and support development of both clinical and administrative staff
- increase practice resilience by supporting remote and at-scale working.
Compared with analogue telephony, advanced cloud-based telephony provides much greater capability to practices including:
- Call back and queue position capability informs the patient of their position in the queue and gives them an option to keep their position and request a call back (where the system automatically re-dials the patient as they approach the front of the telephony queue). This helps reduce the wait times for patients and helps smooth peaks in demand, increasing patient satisfaction and reducing complaints.
- Call routing enables patients to choose options via their keypad or voice options to enable direct routing to the right person or team. These can be configured to match the services in a practice or PCN. This can divert some demand away from phones at busy times. This can be further supported by effective care navigation.
- Welcome and queue messages help set expectations and support up front information gathering, quicker signposting and clinical triage. Recorded messages with health information or information about your practice can help share news and inform callers of other services run by multidisciplinary team members.
- Call recordings (and being able to retrieve recordings) can support individual staff training when used as part of ongoing staff development conversations. The search facility means less time is spent documenting conversations in response to complaints or patient incidents, because they are recorded.
- Reporting supports planning and demand management, improving the ability to plan and track progress and make practice staff capacity and resourcing decisions on evidence.
- Live dashboard reporting enables your practice to react quickly when demand peaks.
- Flexible configuration supports hybrid and home working with the use of ‘soft phones’. The flexible configuration enables the ability to scale with little difficulty when staff and services are shared across more than 1 site or when a new individual, team, service or practice joins. For PCN working, advanced telephony functionality supports business continuity and provides resilience if there is a major incident at the practice (floods, emergencies, covid etc). It supports remote working, sharing of demand or calls being directed to other sites and services.
- Bypass feature allows other services to bypass the usual queuing system.
Which pathway should my practice or primary care network follow?
There are 3 pathways through this document:
- 1 for practices without advanced cloud-based telephony already installed
- 1 for practices with advanced cloud-based telephony already installed and wishing to optimise its use
- 1 for PCNs wanting to move towards more standardised models across their member practices
If your practice does not have advanced telephony installed, start with section 1 which covers:
- understanding advanced cloud-based telephony functionality and benefits
- funding and choosing an advanced cloud-based telephony solution
- contract support and procuring an advanced cloud-based telephony solution
- installation steps.
If your practice does have advanced telephony installed, start with section 2 which covers:
- understanding phone data
- configuration/optimising set up
- staff training and effective conversations
- measure and improve.
If you work in a PCN or within a hub model, start with section 5. You will need to understand the starting points and needs of each practice and agree a local strategy to optimise the use of telephony, staff and capacity.
Section 1: choosing and installing advanced cloud-based telephony
This section describes the differences between analogue and cloud-based technology and why it is important to move to advanced cloud-based telephony.
It provides guidance on how to choose, fund and procure a new system.
If you already have advanced cloud-based telephony, you can skip to the next section.
Why do I need to change my telephony system? By when?
You may not need to if you are already on an advanced telephony or cloud-based telephony system.
By 2025 British Telecom (BT) expect to have moved all customers from the analogue public switched telephone network (PSTN) to a fully digital network. The analogue network will then be decommissioned. If your current telephony system is reliant on the PSTN network, you will need to make the change.
Further information on the UK’s PSTN network switch off can be found on the BT website.
Ensuring all practices on analogue phone systems are supported to move to advanced telephony is a priority for NHS England. It is a key part of the Delivery plan for recovering access to primary care, which was published in May 2023.
Telling the difference between telephony systems
Analogue telephony does not use the internet. Incoming and outgoing capacity on the lines is limited. It is being decommissioned in the UK.
Advanced telephony uses the internet and voice over internet protocol (VOIP). Data and voice travels over the internet and the system prioritises voice over data. The system is usually stored on a local site. Static desk phones are used. It can be more expensive to set up and may need to be set up again if you move or change premises.
Advanced cloud-based telephony is an advanced telephony system which also uses VOIP but data is stored in the cloud providing more data storage and resilience. ‘Soft phone’ extensions are used so the phone number is mobile and can follow the individual, so they are not tied to the same desk or location, scalability is also far easier.
Data and metrics can be accessed by practices and primary care networks (PCNs) using both advanced and advanced cloud-based telephony. The type of data and functionality available may vary, this is covered in more detail later in this document.
Choosing an advanced cloud-based telephony system
A new advanced cloud-based telephony system should provide easy monitoring of data in real time and provide detailed reporting, enabling trends to be monitored over time. Access to rich data like this can help practices adjust their call-handling capacity and processes to meet the needs of their patients, to improve speed of handling, reduce waiting time and generally make the practice more efficient and resilient.
In line with the GP contractual requirements practices should procure a solution from the Advanced telephony better purchasing framework. There are a range of telephony solutions to choose from, all of which offer as a minimum the core level of functionality to meet the national standards and specification.
Choosing an appropriate telephony solution will depend on your practice circumstances and local patient needs.
Using the same cloud-based telephony provider across a PCN can make it easier to share workload, information and resources and to direct patients to the right care more easily. It can build resilience in times of emergency such as a flood or power outage at one practice.
It is advised that you work with your PCN or integrated care system (ICS) and the National Commercial and Procurement Hub to ensure value for money and the best contract terms and conditions.
The procurement hub can support you with understanding:
- usability and flow of the system (demonstration videos for approved Advanced telephony better purchasing framework suppliers are available)
- supplier experience in implementing digital telephony in similar practices or PCNs
- other practices experiences that have been through the installation with the same supplier (and how you might speak with other practices)
- whether the supplier’s system integrates with your clinical system
- when the supplier will be ready to implement, what preparation is required and how long it takes to set up, install and train
- understanding the different training packages on offer (and understanding what kind of training is needed for different roles in the practice or PCN)
- The ongoing support packages the supplier offers. Whether they provide support for the hours you are open and identifying if you will you need extra technical or configuration support.
Functionality offered by advanced cloud-based telephony
Advanced cloud-based telephony systems offer flexibility and scalability making them more future proof than traditional systems.
They offer more functionality than analogue solutions, including unlimited incoming lines, helping you to manage demand and deal with peak time calls more efficiently. The solutions on the Advanced telephony better purchasing framework offer integration with clinical systems, essential for efficient and smooth call handling.
Table 1 in the commissioning support pack lists detailed essential and optional functionality requirements of telephony systems on the Advanced telephony better purchasing framework.
This is a high-level summary of the key functionality:
- Call routing using auto attendant, interactive voice response (IVR), bypass lines for other services, flexible parameters (eg open/closed hours or day/night mode).
- Call back function; enables callers to request a call back instead of waiting in the call queue to be answered.
- Recording and retrieval of active calls or conference calls.
- Messaging, including greeting and hold messages, queue announcements and voicemail.
- Office telephony functions, including hunt groups, practice and group directories, caller ID, hold, transfer, mute, speakerphone, conferencing, local configuration and call monitoring for training and support.
- Reporting that enables practices or PCNs to see call data for the day, week or month.
Contact the National Commercial and Procurement Hub for more information.
Funding for an advanced cloud-based telephony system
Telephony is a practice responsibility funded via the Global Sum and contracts are held by practices.
The Delivery plan for recovering access to primary care provides time-limited funding to enable practices using legacy analogue systems to move to cloud-based telephony solutions, procured from the Advanced telephony better purchasing framework.
Plans identifying practices using analogue systems have been produced by integrated care boards (ICBs). If you meet these criteria, you will be eligible for the support. Your ICB will be able to provide further detail of the offer.
Please note that you will hold the contract with the supplier and following transition remain responsible for the ongoing costs.
There is around £90 million funding attached to the Delivery plan for recovering access to primary care for purchasing and implementing advanced cloud-based telephony systems.
In addition, the National General Practice Improvement Programme (GPIP) provides hands on support for practices and primary care networks (PCNs) over 2 years (2023-2025) to help practices and PCNs move to a modern general practice model incorporating advanced cloud-based telephony.
There is also funding for integrated care systems (ICSs) to provide local or wider support through the Primary Care System Development Funding (SDF).
Further information on funding can be accessed on our website.
Discovery exercise before procuring a new telephony solution
It is advisable to undertake a discovery exercise (see Commissioning support pack – available on the FutureNHS platform which requires a log in) to identify your needs before procuring a new system. You might consider:
- Understand existing practice telephony provision, eg local PBX based, local VOIP etc.
- Identify all existing extensions and external lines (PSTN, ISDN, SIP) and numbers and confirm this matches current billing. Identify the purpose/usage of each external number, eg outgoing calls only, appointments line(s), specific clinics etc. Analyse the activity on each number and extension to identify any unused and any high demand numbers and extensions.
- Identify any existing sources of stored patient identifiable data, eg call recording, call logs and any requirement to retain this data.
- Identify any third-party products, not provided directly by your telephony system vendor, integrated with your current telephony system including clinical systems and clinical system integrators, call recording, call logging etc. Identify and understand the contracts with suppliers of these third-party products.
- Identify any single purpose/dedicated lines and determine if they need to continue in that form, eg alarms. (Note other actions, outside the scope of this document, may be needed here as PSTN (and ISDN) lines will no longer be supported after 2025).
- Identify any branch sites, however small, as a cloud based VOIP telephony system should be able to support these as part of the same practice telephone service.
- Identify any locations, other than authorised practice premises and home working, where access to the telephony system may be required (eg a dedicated GP hub site or PCN site used for remote provision).
- Identify if the existing system is shared with or used by any other party (ie multi-tenant) and if so on what basis and if there will be any impacts of changing.
- Understand any existing practice mobile telephone use and contracts and consider how or if these will be affected by migrating the practice to an advanced telephony solution.
- Identify how many staff currently work from home or remotely or may need to do so?
- Identify where fixed IP handsets are needed (ie phone based VOIP) and where a software-based phone application (softphone) is installed on an end user device (eg PC, laptop, tablet, smartphone) and connected to the service through broadband internet or wireless data connection. See Emergency access considerations later in the support pack.
- Examine existing associated contracts and opportunities and exit terms including notice period and costs.
- Examine the expected organisational and service model developments expected locally in the future.
- Assess existing connections (HSCN or equivalent) and available bandwidth to determine suitability to be used by VOIP. Request technical support from the ICB as necessary for this.
- Determine with the ICB how local IT infrastructure, eg networks may be accessed and utilised. It is important to give this consideration prior to issuing a specification and embarking on procurement.
Equipment you might need
Suppliers will provide you with information on the equipment you need but also consider the following:
- The use of 2 screens is helpful when accessing and moving between the clinical system, text messaging and telephony data.
- A headset with a specific noise reducing microphone is helpful to cancel out any background noise for the patient and member of staff. You may need to check your phone has a USB port to connect the headset to.
- Some practices or hubs have a wall board to display in real time call wait times and abandoned calls. It can usually be configured to show other metrics. Other practices prefer to restrict this to the supervisor’s screen only as some staff can feel anxious when they see the number of calls waiting.
Purchasing a cloud-based telephony solution from the framework
Contact the National Commercial and Procurement Hub, they will help you to:
- obtain a copy of your contract from your current supplier if you don’t already have it
- check your contract expiry dates and help you to exit your current contract, ensuring that you avoid automatic renewal into a lengthy contract extension.
- review and compare the solutions available from the Advanced telephony better purchasing framework
- negotiate standard contract terms, conditions and best price with your chosen supplier.
Installation steps for cloud-based telephony
Different telephony suppliers may use different approaches to installation so always seek their advice or the advice of the National Commercial and Procurement Hub, if you are unsure what’s included.
In general, the steps are:
- site survey
- setting up a new broadband connection
- receive or purchase phones
- porting of numbers (this is if you are keeping your current phone numbers)
- installation of the system
- reviewing and updating information on the practice website (practice privacy notices should be updated to advise of call recording if this is a new feature)
- training on the phone system.
Section 2: understanding and using practice call data
Benefits from being able to see call data
Advanced cloud-based telephony systems collect detailed call data which you can use to help make informed decisions to improve telephony journeys for patients and ease pressures on practice staff.
This data can help you understand:
- when people call and why (broken down by day of the week and hour of the day)
- how many people abandon their call before getting through
- how long people are waiting before their call is answered
- trends over time
- demand across different sites, if you have more than one site
- what hours are peak times when you may need additional capacity
- where effective signposting could help divert non urgent or administrative demand away from the phones during peak times.
Real time data, shown in dashboards enables you to act quickly to flex support. For example, some practices ask the wider team to answer calls if they can see the call wait times increasing.
In addition, having access to call recordings can support individual staff training and development and improve call handling and patient satisfaction.
Accessing your telephony data
Advanced cloud-based telephony datasets provide data in 2 main ways; via a real-time dashboard or by reports.
All suppliers/products on the telephony framework are required to support GP practices with a reporting functionality. Suppliers should provide training on reporting and dashboard set up and use.
4 key telephony metrics
Each system offers a wide range of data to practices, but 4 key metrics are important for measuring improvement in telephony journeys for patients.
Abandoned and missed calls [3]
- daily count by day and hour, Monday to Friday
- total count during the first hour lines open, Monday to Friday.
Some cloud-based telephony systems differentiate between abandoned calls, missed calls and dropped calls. See the glossary for definitions.
Call wait times (time taken to answer call)
- daily average wait time by day and hour, Monday to Friday
- average wait time during the first hour lines open, Monday to Friday.
Number of calls answered
- daily count by day and hour, Monday to Friday
- total count during first hour lines open, Monday to Friday.
Call length times
- daily average by day and hour, Monday to Friday.
What other telephony data is available?
All suppliers/products on the telephony framework are required provide data/metrics to GP practices on the following:
Metric 1: call abandoned (a) – Standardised abandoned call volumes.
National reporting definition: numbers of callers have passed through an IVR selection or have spoken to a member of the practice, and they abandon, disconnect or cancel the call.
Data:
-
Volumes in numbers.
-
Percentages versus total calls.
-
Available in days, weeks and months.
-
Trend analysis added overtime.
Metric 2: time period abandoned (b) – Wait time
National reporting definition: time period abandoned (b) – wait time before call is abandoned.
Data: Total abandoned call times in time brackets. (0-1min 59s, 2min-3min 59s etc)
Metric 3: missed call volumes.
National reporting definition: numbers of calls where the caller rings the practice, there is no connection (engaged tone or unanswered ringing) and the patient abandons the call or a connection is lost before the call is answered and the IVR begins.
Data:
- Volumes in numbers.
- Percentages versus total calls.
- Available in days, weeks and months.
- Trend analysis added overtime.
Metric 4: call backs requested
National reporting definition: number of calls where the caller has requested a call back from a queue position.
Data:
- Volumes of call backs requested.
- Available in days, weeks and months.
- Trend analysis added overtime.
Metric 5: call backs made.
National reporting definition: number of calls where the caller has received a call back from a person in the practice. (Include only call backs where a conversation takes place, or a voicemail is left).
Data:
- Volumes of call backs requested.
- Percentages of made versus requested call backs.
- Available in days, weeks and months.
- Trend analysis added overtime.
Metric 6: average call length times – once connection has been made, average call length for incoming calls only (talk duration).
National reporting definition: total duration of every call. From connection to disconnection.
Data:
- Total average call times in time brackets. (0-2min 59s, 3min-6min 59s etc).
- Call lengths at different times of day and viewable rolling 12m view.
Metric 7: call times to answer – time taken for a patient to reach their required destination or speak to a member of staff.
National reporting definition: total duration of every call from connection to reach the IVR selected or to speak to a member of staff.
Data:
- Total average call to answer in time brackets. (0- 59s, 1min-1min 59s etc)
- Call lengths at different times of day and viewable rolling 12 month view.
Metric 8: call volumes – standardised call volumes.
National reporting definition: total number of calls received by the practice. (Some solutions may also include volume of outgoing calls).
Data:
- Volumes in numbers.
- Percentages versus total calls.
- Available in different points in the day, days, weeks and months.
- Trend analysis added overtime.
Metric 9: system outage reports (not mandatory as standard but must be available on request from practice).
National reporting definition:
- Total number of outage events and minutes lost of telephony systems in the last rolling 12 months.
- Time taken to re-establish full system functionality at each outage event.
Data:
- Total no of outage events.
- Total minutes lost.
- Viewable on 12month rolling view.
Real time telephony dashboards
The dashboard is useful for real-time monitoring of calls throughout the day. This real-time view enables practice to flex the number of call takers if demand peaks.
The call metrics included and displayed in the dashboard can be adapted to practice requirements. These often include:
- number of calls waiting
- number of calls abandoned
- length of time waiting
- length of calls.
Practices also find having a breakdown of the above data by staff member helpful. This helps them identify anyone that may need support or training.
It is important to agree who will view the dashboard. Some staff have reported feeling anxious when they can see the number of calls waiting, therefore practices may find it useful to have the option to switch their individual dashboard on or off for staff taking calls, leaving the dashboard available only for those overseeing the call taking or who are responsible for monitoring peaks in demand.
It is important to also agree if the use of a wallboard would be helpful in call centres or hubs and what metrics would be useful to show. It can show real time information for responsive management of calls.
Image 1: example of a telephony dashboard
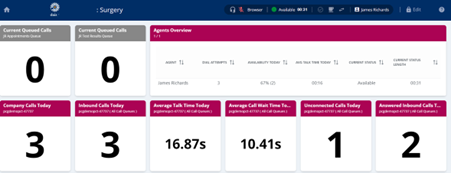
Image 1 is an example of a real time telephony dashboard which gives a simple data overview of call activity over a specific period of time including volume of calls, calls waiting, average wait times, etc.
Image 2: example of a telephony wallboard
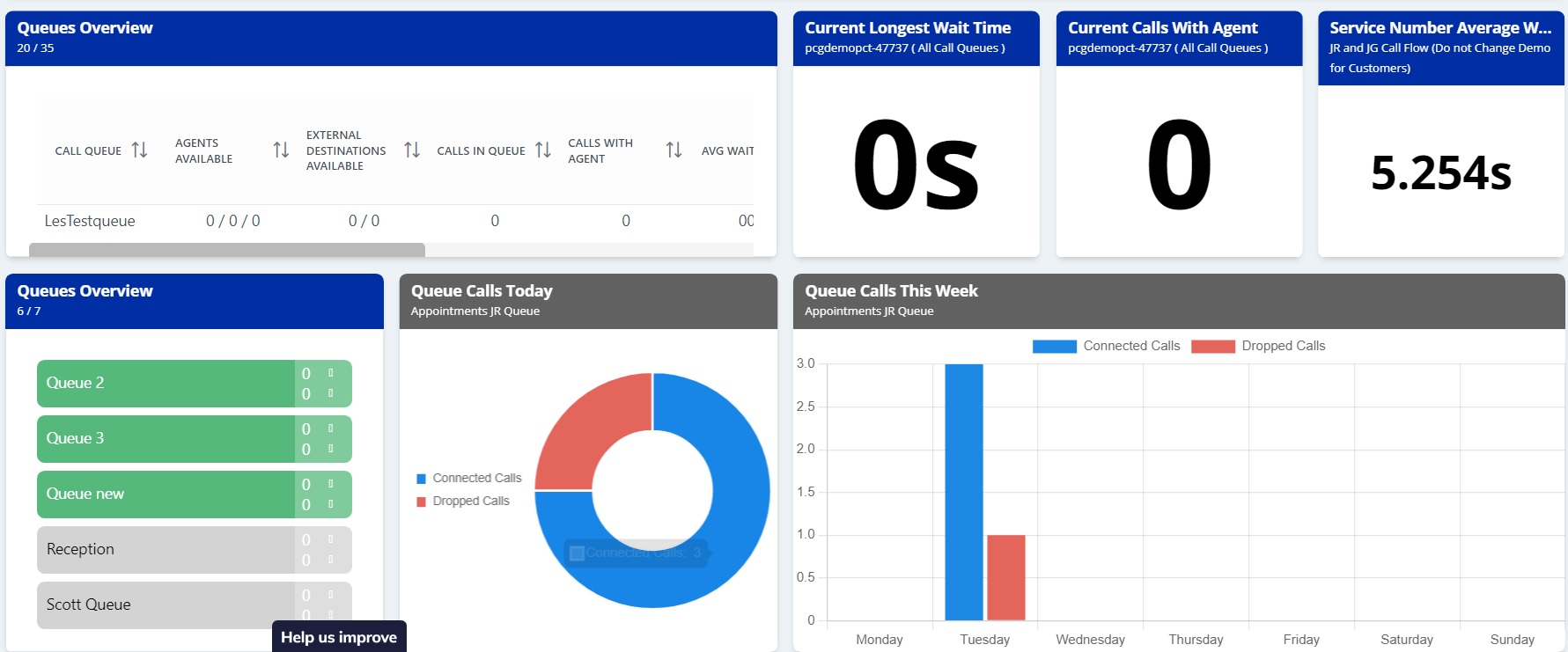
Image 2 is an example of a telephony wallboard. It shows an overview of the queue including how many are in each queue, how many calls were connected versus dropped today and over the past week, the longest wait time, the current calls with call takers and the average wait time in seconds.
Image 3: example of a telephony wallboard
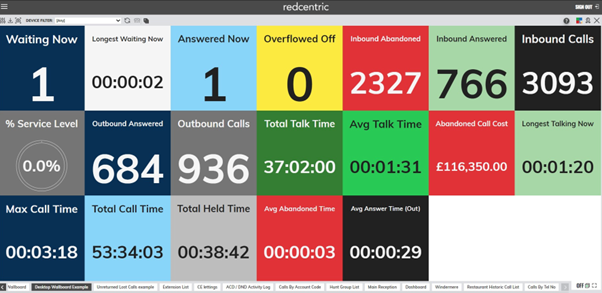
Image 3 is a different style of showing telephony data in an easy to understand format showing different types of key data that might be shown on a wallboard, including call volume, average call time and unanswered calls.
This example shows how many calls are waiting, the longest wait, the total calls answered and total inbound calls. It also shows average talk time, a service level percentage view, abandoned calls and total time on hold.
Telephony data pitfalls
Knowing some of the potential pitfalls can be helpful when interpreting telephony data. This section aims to share learning to help you avoid them.
When monitoring missed or abandoned calls, it may not mean each call is from a unique number or 1 individual. It may be the same person calling back several times.
There is a difference between abandoned and missed calls and between volume of calls and calls answered. Make sure you’re measuring the right ones for your purpose.
You may see an increase in average call length times if you are introducing call scripts to collect structured clinical information as part of a care navigation model for the first time.
When improving telephony journeys, you may initially see an uplift in total contacts to practice when reviewing data across all access routes (phone, in person, online). This may be due to some patients calling the practice and choosing to divert to online options, or it might be the same person sending the same request to different channels.
Setting clear expectations on when a patient will hear back from the practice about next steps for their clinical or administrative request is vital especially in online channels.
Clear expectation setting helps patients choose an appropriate channel (for example if the online response time is ‘within 2 working days’ it’s not suitable for urgent clinical requests) and to avoid follow up calls or online contacts to check on progress.
You can read more about this in companion guidance ‘Creating highly usable and highly accessible GP websites’ available via the resources page of the national General Practice Improvement Programme.
Understanding and using telephony data
The exercises below aim to provide you with:
- an understanding of the volumes of calls throughout the day, especially at peak times
- a breakdown of what patients call you for
- how you might match your call handling capacity to the demand
- how you could divert some of the demand away to more appropriate places (for example physio, community pharmacy, online).
It is advisable to carry out all four exercises below in the order they appear.
Peak time call volumes exercise
The aim of this exercise is to quantify call volumes and highlight the issue that additional resource, to cover peak times isn’t sufficient on its own to resolve the problem. It is often unachievable to answer all calls in the first 30 minutes or hour.
- First look at the following practice data:
- average length of calls
- total number of calls answered
- per day per week
- per hour per day
- total missed and abandoned calls
- per day per week
- per hour per day
- Work out how many people it would take to answer all the missed and abandoned calls that come in the first 30 minutes or hour.
Calculation: Missed and abandoned calls x call length = the number of people it would take to answer those calls in the first 30 minutes. In this example we are assuming an average call length of 5 minutes, therefore 1 person can answer 6 calls in 30 minutes.
Practice X has a total of 50 missed and abandoned calls between 8am-8.30am.
50 calls/6 = over 8 people to answer the missed and abandoned calls in first 30 minutes.
Include: The total missed and abandoned calls, where possible.
See: The glossary for definitions of abandoned and missed calls.
Appropriate calls exercise
The aim is to identify how many calls were appropriate calls by collecting a sample of call outcomes during peak hours and reviewing how many were for urgent appointments, and how many were not for urgent appointments and/or could happen outside of peak times.
How to get this information:
- If menu buttons are used, identify how many callers pressed 1, 2 etc. This may only work if there is a broad enough range of options and if the reporting is set up
- or if calls are recorded – listen to a sample of 8am-9am calls – how many calls were for an urgent appointment versus not appointment.
- collect a simple log of calls with the reception team regarding the number of calls that were not appointment related (eg sick note, results, referrals, prescriptions, medication, contact information queries).
To help, you may wish to break down calls in this way:
- appointments – break down by new (urgent/non-urgent), reminder and cancellations
- referrals and signposting – break down to secondary care, mental health improving access to talking therapies, physiotherapy, pharmacy, any other practice Additional Roles Reimbursement Scheme roles.
Call handling rota exercise
The aim is to match capacity and skills to demand.
Using the information from the peak-time call volumes exercise, and the appropriate calls exercise to:
- identify peaks in demand by day of the week and by hour of the day
- review the number of staff and skill sets available, where there are gaps, where is their capacity used?
- identify who else within the practice could support call handling at peak times?
Diverting calls exercise
The aim is to spread demand away from peak call times or to other appropriate channels:
- Review the reasons for calls from the appropriate calls exercise. What are the alternatives?
- Can any of them be diverted to the most appropriate person or service more quickly? Switch channel – where appropriate move administrative calls to online (eg repeat prescriptions, sick notes, cancel appointments).
- Do you have the right options in the right order on the phone menu to divert people before they reach reception/admin team? eg physiotherapy, community pharmacy, specific non triage appointment booking, eg flu or cervical screening.
- How else could you divert patients to other channels? eg recorded message signposting sick notes, repeat prescriptions, cancelling appointments to online channels and introduce signposting as part of a standard call script.
- Actively signpost to other appropriate services using call menu options to support this and an up-to-date directory of services for quick and efficient signposting and information, eg pharmacy for medication enquiries, physiotherapy, internal services and external services and organisations.
- Can you reduce the length of some calls? (Note: if call handling scripts have not previously been used, the introduction of them may increase the length of some calls, especially at first).
- Increase call handling capacity to match the peak times.
Section 3: setting up or optimising telephone journeys
A new telephony system alone will not reduce the 8am rush, reduce call lengths or immediately reduce the burden on your practice.
Practices need to take advantage of some of the functions advanced telephony offers and to adjust ways of working to be able to improve the patient experience and ease the pressures on staff in the practice.
This section provides top tips grouped by theme which should help you optimise your telephony system and improve the experience for you and your patients.
Aligning call handling capacity with demand
Data should help drive decisions. By using data, you may be able to smooth demand away from peak times. You could:
- Rethink staff rotas and try to match capacity to the call volume data and patterns. Consider if you need more people on a Monday or at peak times such as 8am, lunchtimes and 3pm. The rota pattern should mirror regular demand patterns.
- Use the real time data to identify sudden peaks in demand or longer queuing times.
- Ask the whole admin team to answer calls at peak times such as a Monday morning. Once set up, cloud-based telephony can allow anyone in the practice to view real-time data and pick up a call from any phone they are logged into to, in any room.
- Re-arrange the appointment book so only urgent appointments are available on a Monday, non-urgent need can be diverted to the next day or later in the week when the peak has dropped. You can read more about this in companion guidance Aligning capacity with demand available via the resources page of the national General Practice Improvement Programme.
- Introduce call taker scripts to standardise the gathering of information and to support practice protocols. Initially the introduction of scripts may cause a slight increase in the length of calls. You can read more about this in companion guidance Care navigation available via the resources page of the national General Practice Improvement Programme.
Diverting call demand
Diverting patients to options that may be more appropriate for them can help divert and reduce phone demand.
Adding phone message selection options to alert patients to other services and alternative ways of sending a request can be a useful way of diverting patients to more appropriate services. Those that prefer, may choose to use online services.
Practices can:
- Set up menu options to divert patients directly to other services such as physiotherapy, community pharmacy, results and letters.
- Re-order menu options to alert patients to alternatives rather than always selecting the first option for appointments.
- Set queuing messages to inform patients they can carry out administrative tasks online such as ordering repeat prescriptions, sick notes or cancelling appointments.
- Where appropriate make non triage appointments directly bookable or have an option on the phone system to select this, eg cervical screening, immunisations.
- Switch on messages for out of hours to divert callers to NHS 111 and out of hours services.
Reducing missed or abandoned calls
Missed calls happen when the patient can’t get through. This often occurs on analogue systems when the number of lines is restricted, however it can also happen on advanced telephony systems. To help prevent this you can increase the setting for the number of callers ‘allowed’ in the queue. For example, if the limit is set to 50, caller 51 will not be able to get through. Increasing this to 500 will resolve the problem.
Abandoned calls occur when the patient has joined the call queue and then decides to leave the queue. Patients may leave the call queue for several reasons. If you have effective messaging that diverts administrative or non-urgent demand to online, you may see an increase in abandoned calls.
- Keep an eye on trends especially if you change your phone queue messages.
- Review how long your welcome message is, it may be too long.
Setting up effective call routing and flows (call trees)
Call routing rules help you decide where you want calls to go. This will depend on your practice staff structure, use of additional roles and services such as first contact physiotherapy roles or community pharmacy consultation service (CPCS), day of the week and time of the day, the season and in some cases, caller identification.
Practices can use phone queuing messages or option buttons to signpost patients to other roles within the practice. For example, to encourage patients to use online services for admin requests, this can help filter the calls before they reach the reception team. Always be clear about response times for alternative routes.
Setting up option buttons and using clear terms helps identify what patients are calling for and helps get patients through to the right team or person for their enquiry. For example, ‘press 1 for admin’ is quite broad, ‘press 1 for referrals and letters’ is more specific and clearer. Using language used by patients is important, for example ‘press 1 for blood tests’ is likely to be more familiar than ‘press 1 for phlebotomy’.
Set up seasonal option buttons to cope with seasonal demand. For example, some practices signpost hayfever enquiries to community pharmacy during the summer season by adding an additional option on their phone system. The use of options can also provide a practice with more detailed data on the reason for calling, supporting future changes to call routing or demand and capacity management.
Put the options buttons in the right order. This may have a positive impact on call volumes. Some practices prefer to offer patients alternatives before asking them to press an option for an appointment. Not only can this inform patients of other services but can route patients away from usual choices to more appropriate services, eg community pharmacy or first contact physiotherapy services.
Always log out from a phone when you walk away from it. Not logging out can cause a delay to calls being answered because they bounce around the phones until one becomes free.
If you work in a hub or a group of practices:
- agree where to route overflow calls
- set up your telephony system so you can identify which practice the patient call originated from.
Once you have mapped out your call tree, you will need to test it.
You may need to change your call tree from time to time. For example, if the usual practice opening hours change, if team structures change or a new role is introduced. Monitor the 4 key metrics so you can identify trends or anomalies that might tell you how well call routing and flows are working.
Image 4: shows an example of a call routing and flow map, sometimes called a ‘call tree’
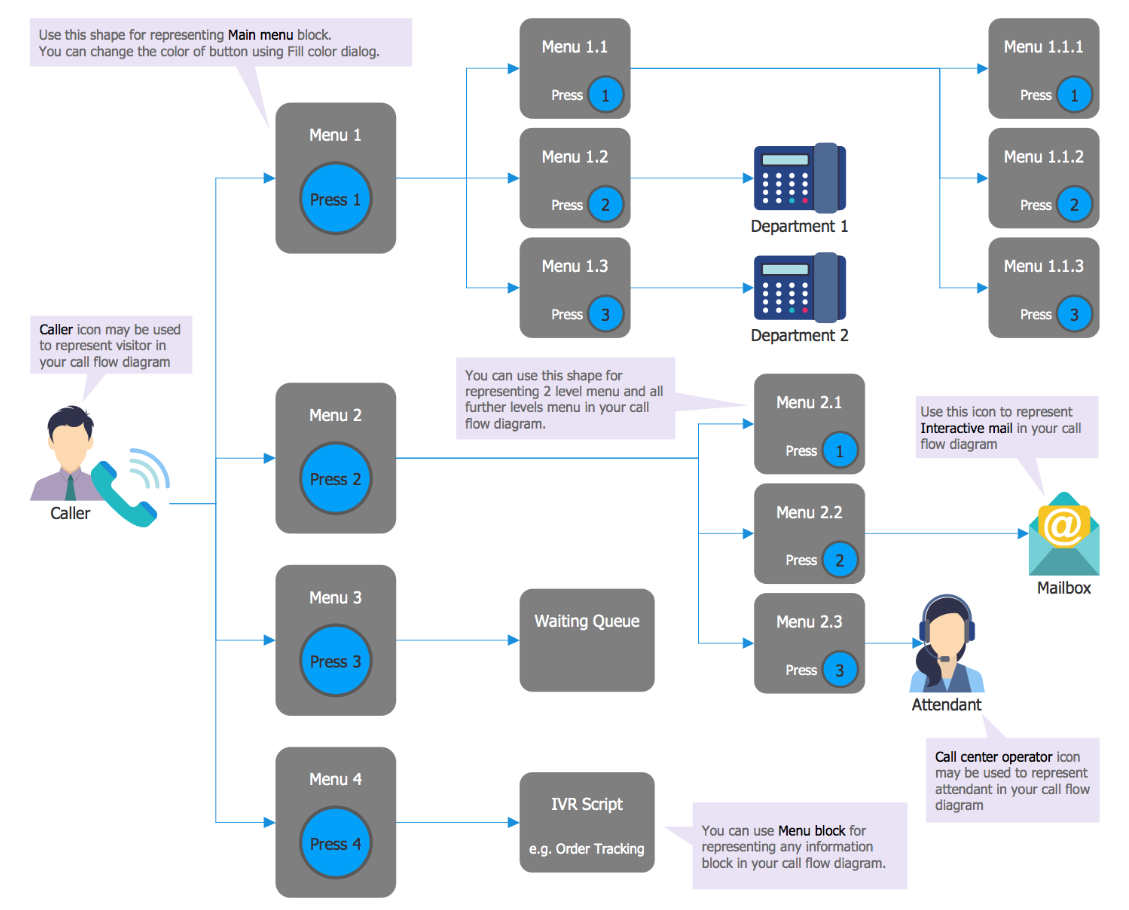
Image 4 is an example of a call tree in the format of a flow chart which shows the different ways calls can be routed to the most appropriate place, based on the patients need and time of call.
Setting up messages and using call queue time
Use a short welcome message to explain to patients they will be asked some structured questions about the nature of their enquiry, to get them to the right person and to help the clinicians prioritise the calls.
- This welcome message is also an opportunity to tell the caller about accessing services online through the practice website or the NHS App.
- It’s advisable not to make this welcome message any longer than necessary. Patients may get frustrated if the introductory message is too long. 60 seconds is a good maximum length.
Personalise your recorded phone messages or change them at regular intervals to keep attention of regular callers. Some practices record a familiar voice, such as the GP at the practice, others change the automatic voice and messages at regular intervals to stay up to date and keep interest.
Use the queue ‘hold time’ to explain what things a patient can do in which online channels and encourage their use or to share health information.
Set up out-of-hours messaging or routing to signpost to out of hours care and inform callers when the practice will be open again. You may be able to set up time schedules to automatically switch over the message at the right time.
Example welcome and queue messages
“Welcome to The Medical Practice. Please note, that all our inbound and outbound calls are recorded for quality and training purposes.” (Daisy Communications example welcome message).
“The receptionist will ask you about the nature of your problem. By providing the receptionist with a brief reason for your call, our GPs and other team members can identify the best source of help for you. This information is entirely confidential.
“Did you know you can request medical help, order repeat prescriptions and request sick notes via our website and the NHS App?
“Our highly trained reception staff have been asked by our GPs to ask you for a brief reason for your call. This is so they can direct you to the person or service that would be most suitable for you. You can order prescriptions and find your test results via the NHS App.
“There are now more ways to get in touch with us. You can now use a secure online form on our website to request help. Just answer a few questions, click send, and we will ensure you get the help and support that’s right for you. And, as always, you can choose to contact us by phone or by visiting us. (Administrative triage using digital tools in General Practice – elearning for healthcare (e-lfh.org.uk)).
“However you choose to get in touch with us, our dedicated medical team will respond based on your unique circumstances.
“The next steps will be tailored to your needs: it could be a face-to-face appointment, a phone or video consultation, or a simple text message with advice or inviting you to come in for a blood test, for example”.
Setting up bypass access
Some teams and services require fast, direct access to the practice team and may require bypassing the phone queuing system. Identify if your system has this feature and how to set up bypass routes with your telephony supplier.
- Identify which services should have access to bypass numbers (eg ambulance service, care homes, pharmacy, community services, palliative care, tertiary services).
- Identify how to set up caller identification (caller ID) and what happens if a number is withheld.
Testing business continuity
Whilst cloud-based telephony offers additional resilience, it won’t work in the event of a power outage. Practices and primary care networks (PCNs) should always test business continuity when there is a change in practice.
- Carry out a full review of your business continuity plans. This should include operational resilience and contingency arrangements for the telephony service. Some practices have back up power and emergency mobile phones charged and ready.
- Complete a clinical safety risk assessment DCB0160. This should be carried out by the integrated care board (ICB) on behalf of their practices with individual practices working collaboratively with the local clinical safety officer to complete the risk assessment.
- Test the end-to-end journey with a test patient in different scenarios and patients with different needs is always advisable to identify any problems with the flow, routing or diverting.
- Test the end-to-end journey with services you connect with, eg ambulance, community, palliative care.
Section 4: continuous improvement
Improving telephony journeys is one part of a modern general practice model and it is recommended you measure the key metrics outline in section 2 regularly and consider further improvements you could make.
Some key principles when improving the experiences for staff and patients whilst re-designing services or processes are:
- Co-design services with patients and staff from the start and throughout.
- Share data and learning in your team and with your patients.
- Encourage open discussion, set up peer-peer support.
- Have a supplier contact if you need training, support, to report any issues or make system changes to adapt the offer to meet local need.
- Remember telephony is one part of the solution to implement the modern general practice model.
- You will need to iterate changes. That’s ok.
- Meet as a team to better understand everyone’s needs and to discuss what needs attention. Ensure it is mitigated as soon as possible to maintain momentum and quality of service.
Using telephony to measure patient satisfaction
Measurement is key to improvement.
Some telephony systems enable rules to be set up to collect feedback from the caller. The caller can be asked to press 1 for a positive experience and 2 for negative. More detailed options can be configured if required.
“Thank you for calling the practice, to let us know how we did, please press 1 if your experience was positive or 2 if it wasn’t”.
Example staff satisfaction questions
“On a scale of 1-5 how are confident are you feeling about using the telephony system?”
“What’s going well with the new system?”
“Is there anything that could be improved?”
“Please tell us what support or training you would find helpful”
Section 5: primary care networks and at scale working
Practices within a primary care network (PCN) deliver local services by working together with each other and other local services such as community care, voluntary services, social care, physiotherapy and community pharmacy.
Having a larger, more flexible workforce means they can develop efficiencies in how services are delivered and give patients better access to specialist health services closer to home.
PCNs can also share resources and information and can create local networks of knowledge and peer support. This shared active learning is often a positive step towards developing a sustainable approach to improvement and change.
This section shares learning from others on how to proactively move from whichever improvement stage you are starting at, to the next through manageable steps.
Primary care network and cloud-based telephony
You may already be working collaboratively as a PCN and are looking to align more closely and work collaboratively and share peer learning.
Working at scale in telephony can help increase alignment; starting with common equipment and common configuration of telephony used across the PCN. A second level of integration with shared operating processes and training. These first 2 stages of alignment can also facilitate shared call handling.
Stage 1: common telephony system
The need to move from analogue telephones to advanced cloud-based telephony provides an opportunity (and funding in many cases) to improve telephony journeys and also for PCNs to purchase the telephony systems.
All or most practices using the same telephony systems provides many potential benefits:
- The ability to share training and learning across practices; potentially reducing cost and increasing resilience.
- Peer support; everyone using the same tools.
- Purchasing leverage.
- Resilience; the ability to provide support to other practices in case of emergency.
Different practices will be at different stages, with different needs and current pressures. It is important all parties have an opportunity to discuss the potential benefits of using the same telephony system, how things might work and what commitment needs to be made by when. These conversations should include discussion with wider practice staff and patients.
If agreement in principle is reached, practices often undertake a mapping exercise to:
- map processes
- identify capacity and skills you have in each team and what functions they carry out
- identify locations, estates and services
- identify telephony contractual position.
Following this, practices move to finalising their needs, reviewing options and committing to purchasing their individual phone systems from the same supplier. (See section 1 for further details). They also agree:
- Finance and funding flows – some practices have reported significant savings made because main calls between main and branch sites which are now free and savings on handset lease costs. (See Midlands and Lancashire CSU case study: supporting primary care with robust IT infrastructure, 14 March 2019).
- Data processing agreements and privacy notices – complete a data protection impact assessment to identify any impact on the handling of personal confidential data across a PCN.
The final stage is for each practice to install and migrate to the same telephony supplier:
- local data metrics to be monitored, agreed and set up (step 1)
- local call flow plans agreed (step 3)
- local call routing set up (step 3)
- individual practice privacy notices should be updated to advise of call recording (if this is a new feature)
- telephony training can be standardised yet tailored to provide different types of training to meet your needs, depending on your set up.
Stage 2: common processes and data led approach
As practices and the PCN develop, they often work to align their processes and use telephony and other data to help define the way they want to work (the ‘to be’ process) and the governance around that. This can include:
- Alignment of processes, protocols, and the directory of services across the PCN supported by call routing. This means patients can expect a similar experience with whomever they interact with and with shared information, patients shouldn’t have to repeat their story.
- Combined reporting and dashboard data is easier to compare across the same telephony provider. The same provider, underpinned by the same processes and protocols at each practice, means that data is easier to compare. It may also be easier to manage discussions, support, training, system development and costs with one telephony supplier. By analysing the data, it can tell you where and when demand is at its greatest or lowest and what the demand is for.
To do this you need to agree strategy and principles. This should include the vision, the benefits and key principles that will be applied to the change and the way you implement the change. For example, a key principle might be to keep patient experience at the centre.
Once you have an agreed strategy and principles, you can develop a plan to move to single approach.
- Consider the different starting points of each practice. Some may be further along the journey than others.
- Engage each practice and their team in the plans and identify who else needs to be involved.
- Make sure you have regular touch points and opportunities for all staff to feed back.
Stage 3: shared call handling and a proactive data led approach
Having common telephony equipment and common working arrangements and comparable data enables practices/primary care networks (PCNs) to work together more closely:
- Managing demand across all sites is easier at peak times or times of unexpected high demand, because there is a larger staff pool. Cloud-based telephony ‘soft phone’ capability means staff can view and pick up calls from any practice or home, offering ever greater flexibility. Sharing this demand across the PCN team can ease the pressure.
- Matching the right capacity and skills to demand and identifying any gaps in roles can be highlighted with the use of data. Practices may have different population demographics and demand may peak at different times, one practice may require more mental health support another may require more social prescribing.
- Offering patients choice and access to other health professionals such as mental health practitioners, paramedics, nurse practitioners, pharmacists and social prescribers can be supported by setting up routing and keypad options to the patient when they phone the practice. This can divert calls away from the main reception to part of the team that can help them with specific queries or online services.
Setting up active learning systems
- A process for staff and patients to feed back their experiences can hugely benefit patient and staff.
- You may need to change the way the team works, set up new training or protocols. Providing safe spaces for staff to feed into the plans and to feedback on what’s working and what is not working so well, is an important part of the journey and learning for everyone.
Data led
- Proactively manage demand and capacity across PCN service in place. Make sure the data from practices is measuring in the same way. Combine the data to give a complete picture across the PCN.
- Use the data to monitor trends, identify differences or similarities.
- Use data to support your decisions about resources, capacity, services and to improve experience.
Difficult decisions
When making improvements and implementing change, there are sometimes difficult decisions to make, for example regarding staffing, skillsets, role changes, working hours and locations.
Practices we spoke to used data to support transparent decision making, and when designing their delivery models. Some decisions included where to locate future services and data was used alongside open discussions with patients and staff to help build a strategy and approach.
One practice moved to an integrated call centre supporting 5 different sites. The call centre staff are provided with specific call centre training. The staff here specialise in call handling, gathering information from the patient and signposting. Requests are entered into a workflow for review-navigation-prioritisation-allocation.
Another group of practices has a smaller call centre, for about 10 people. They reviewed their call data and realised some practices were busier than others, so they adjusted their capacity to match the demand and rotated staff across all sites to support their development and balance the load. During their induction, staff gain insight into other roles within the practice by spending time with key members of the practice team, clinical and administrative.
This has encouraged several to develop their interest in other areas and move into health care assistant, nurse and phlebotomy roles whilst keeping the knowledge of the administrative team and their skills within the NHS.
Support offers for primary care networks
There is nationally funded training and support available for primary care networks (PCNs) as part of the General Practice Improvement Programme (GPIP).
Find out more about capability building support offers.
Glossary
Active learning
Active learning is an approach, rather than a fixed set of activities. It can include any activity that encourages [taking] an active, engaged part in the learning process, such as:
- group discussions
- presentations
- experiments
- quizzes
- problem-solving
- role-play
Active learning is about providing the environment and opportunities for students to build knowledge and understanding of a subject for themselves.
Analogue telephony
Does not use the internet. Incoming and outgoing capacity on the lines is limited. It is being decommissioned in the UK.
Advanced telephony
Uses the internet and voice over internet protocol (VOIP). Data and voice travels over the internet and the system prioritises voice over data. The system is usually stored on a local site. Static desk phones are used. It can be more expensive to set up and may need to be set up again if you move or change premises.
Auto attendant
Is generally considered basic in the sense that all it can do is route calls. Most advanced phone systems have an auto attendant capability. The auto attendant can have several parameters, such as day/night mode, open/closed hours but the call’s final destination is a call queue, a ring group, an external number or a voicemail box. Auto attendant can play hold music, or pre-recorded information while it routes the call.
Cloud based telephony
An advanced telephony system which also uses VOIP but data is stored in the cloud providing more data storage and resilience. ‘Soft phone’ extensions are used so the phone number is mobile and can follow the individual, so they are not tied to the same desk or location, scalability is also far easier.
Hunt groups
A hunt group is a number of people (or members) that are set up to take incoming calls. Each group can be set to ring in 3 different modes:
Broadcast – simultaneously rings at each non-busy telephone in the hunt group.
Sequential – rings the first telephone in the hunt group list. If that telephone is busy, the system continues down the hunt group priority list until a non-busy telephone accepts the call.
Rotary – the call starts at the member telephone that appears on the list after the telephone that answered the last call. If that telephone is busy, the system proceeds down the priority list until a non-busy telephone is reached.
Missed calls
A missed call occurs when the patient can’t get through.
It’s when the caller rings the practice and there is no connection (engaged tone or unanswered ringing) and the patient abandons the call or a connection is lost before the call answered and the interactive voice response (IVR) begins.
This often occurs on analogue systems when the number of lines is restricted, however it can also happen on advanced telephony systems. To help prevent this you can increase the setting for the number of callers ‘allowed’ in the queue. For example, if the limit is set to 50, caller 51 will not be able to get through. Increasing this to 500 will resolve the problem.
Abandoned calls
Numbers of callers have passed through an IVR selection or have spoken to a member of the practice, and they abandon, disconnect or cancel the call.
This can be for a number of reasons. If you have effective messaging that diverts administrative or non-urgent demand to online, you may see an increase in abandoned calls.
Dropped calls
(Working definition) This is where a call has dropped out for technical reasons or a fault.
Call wait times (call times to answer)
Total duration of every call from connection to reach the IVR selected or to speak to a member of staff.
Call length times
Once connection has been made, average call length for incoming calls only (talk duration). Total duration of every call. From connection to disconnection.
Interactive voice response (IVR)
A technology that allows telephone users to interact with a computer-operated telephone system through the use of voice and dual-tone multi-frequency (DTMF) tones input with a keypad.
Further information is available on the BT Cloud Work website.
General Practice Improvement Programme (GPIP)
The national General Practice Improvement Programme, was introduced as part of the delivery plan for recovering access to primary care in May 2023. The programme will provide support for practices and primary care networks (PCNs) over 2 years (2023-2025) to make changes and improvements to how they work.
The focus will be on helping practices and PCNs to have more control over their workload, maximise the use of all staff roles and local services, meet the needs of patients and provide safe, equitable care.
GPIP will provide 3 levels of support, all underpinned by the principles that change should be clinically-led, data-driven and evidence-based.
Primary care network (PCN)
GP practices are working together with community, mental health, social care, pharmacy, hospital and voluntary services in their local areas in groups of practices known as primary care networks (PCNs).
PCNs build on existing primary care services and enable greater provision of proactive, personalised, coordinated and more integrated health and social care for people close to home.
Integrated care system (ICS)
Integrated care systems are partnerships of organisations that come together to plan and deliver joined up health and care services, and to improve the lives of people who live and work in their area.
Integrated care board (ICB)
An integrated care board is a statutory NHS organisation responsible for developing a plan for meeting the health needs of the population, managing the NHS budget and arranging for the provision of health services in the ICS area.
Voice over internet protocol (VOIP)
Technology that allows people to make phone calls over the internet
DCB0129 standard
This standard provides a set of requirements to promote and ensure the effective application of clinical risk management by those organisations that are responsible for the development and maintenance of health IT systems for use within the health and care environment.
DCB0160 standard
This standard provides a set of requirements to promote and ensure the effective application of clinical risk management by those health organisations that are responsible for the deployment, use, maintenance or decommissioning of health IT systems within the health and care environment.
Other resources you may find helpful
- Advanced telephony better purchasing framework
- Advanced cloud-based telephony commissioning support pack
- Advanced telephony better purchasing framework and buyer’s guide
How to improve telephony journeys in general practice
Bakhai M, Vallely D, Croney L
This guidance was prepared by NHS England’s Primary Care Transformation team as part of the national General Practice Improvement programme.
If you have any questions or would like to send feedback, please get in touch: england.pctgpip@nhs.net.
With thanks to:
- Better Health MCR Primary Care Network (PCN), Rothschild House Group and all the practices and PCNs we spoke to, for their invaluable time and expertise.
- National Commercial and Procurement Hub
- GPIT Digital Primary Care team
- Folkestone and Hythe Rural PCN
Publication reference: PRN00615_iv

