Foreword
Support workers in maternity settings are vital members of the maternity team providing a wide range of care and support every day to the women and families we care for, and the whole maternity team. The first competency framework allowed us for the first time to put a formal support structure around these important roles. Now, as we have continued to see the evolution of their work and the continued dedication of those in the roles, we are delighted to be able to publish this updated version to reflect the breadth and depth of the work they do.
This framework provides the blueprint for the development of support worker roles across maternity services. It was originally created in 2019 in response to the Government recognising that professionalising the role of support workers is vital to delivering safe and personalised care. This refreshed framework ensures that this essential group of staff working within our maternity services can continue to develop by having the right knowledge, skills, education and training to work alongside midwives and others within the multidisciplinary team to provide effective and seamless care.
We would like to extend our thanks to all those colleagues who have supported and engaged with us so constructively throughout this process to develop the refreshed framework.
This framework not only achieves an ambition of the Three year delivery plan for maternity and neonatal services (NHS England 2023), but it also contributes to the vision of the NHS Long Term Workforce Plan (NHS England 2023) to train and retain our workforce.
Kate Brintworth, Chief Midwifery Officer, NHS England.
How to use this framework
Employers should use this framework in conjunction with the Maternity support worker implementation and mapping toolkit to understand and implement maternity support roles safely and effectively. This framework describes the different levels of competence expected of the maternity support workforce, as well as associated activities, entry criteria and academic requirements for working at each level, the different pathways to achieve framework competencies and onward career opportunities.
Educators should use this framework to develop curricula to enable the maternity support workforce to achieve academic exit requirements at each level in order to operate safely within role.
Maternity care assistants (MCA), maternity support workers (MSW) and assistant practitioners (AP) (maternity) should use this framework to understand the requirements of their role, the knowledge, skills and values they need to work safely and the development pathways potentially open to them, including opportunities beyond level 4 of the framework.
Women and their families should use this framework to understand the capabilities of the MCAs, MSWs and APs (maternity) providing care to them, their newborns and families during their maternity journey.
This framework is split into 3 parts:
- part 1 summarises the changes made to this framework following our review
- part 2 details updated MSW roles and aligned educational levels (including role descriptors)
- part 3 details the updated competencies and supporting indicators
This framework replaces the 2019 version. New entrants and existing support workers who have yet to commence their development pathway or who have not yet started to prepare for assessment should meet the requirements of this framework.
MSWs who have already met framework requirements and apprentice MSWs who are currently working towards 2019 framework requirements will not have to move onto this new framework unless directed to by their employer. However, it is recommended that ongoing support with development is provided to enable these individuals to identify any gaps in their knowledge and skills that are features of this framework.
Part 1: the context and outcomes of the framework review
Since the launch of the original framework in February 2019, other structures have been developed, including the new 2023 Senior Healthcare Support Worker Apprenticeship Standard (Option 2: maternity support), the HEE Level 3 voluntary curriculum, care certificate, ESR coding, eLearning and functional skills training and support.
NHS England commissioned a review to produce a revised framework, alongside an MSW implementation and mapping toolkit to support trusts.
With the support of an expert stakeholder group representing employers, midwives, academics, the Royal College of Midwives and maternity support workers, the 2019 framework was reviewed and refreshed. Role descriptors, education pathways and the competencies at level 3 were mapped against the new 2023 Senior Healthcare Support Worker Apprenticeship Standard (Option 2: maternity support). In addition, the emerging requirements of employers in successfully recruiting, preparing and developing the MSW workforce, along with the experiences of maternity support workers and education providers were considered. Collectively, these informed the changes detailed below.
Summary of changes to the framework
The following changes have been made to the framework:
1. A change of name of support worker has been made at level 2 and 4 to reflect current naming convention practice and to improve clarity:
- maternity care assistant (MCA) replaces maternity housekeeper
- assistant practitioner (AP) (maternity) replaces level 4 maternity support worker
2. The role descriptors have been updated to include:
- updated role titles
- the words “newborn infants” when women and families are mentioned, for clarity
- the addition of safety descriptors at level 2 (maternity care assistant) for example, “work safely under the direction…” and “may undertake delegated basic care tasks…”
- the alignment of language to the 2023 senior healthcare support worker apprenticeship standard (option 2: maternity support) descriptor at level 3 (MSW) for clarity
3. The education and training section has been reworked to include:
- refreshed, simplified diagrams to clarify entry criteria at each level of the framework, and the pathways to achieve academic exit awards and other framework requirements at each level, including reference to NHS England MSW modules
- an updated academic exit award to reflect new 2023 senior healthcare support worker apprenticeship standard
- removal of reference to a study skills module and preparation for higher education within the academic exit award section at level 3
4. Competencies and indicators have been mapped and changes made to include:
- updated role names at level 2 and 4 of the framework
- language and activities have been updated to align to the 2023 senior healthcare support worker apprenticeship standard (option 2: maternity support) and knowledge, skills and behaviours descriptors
- the addition of “newborn infants” to all competencies and indicators that reference women and their families
- the inclusion of enhanced safety language, where required, to improve clarity of scope of role
- competency gaps in relation to new apprenticeship standards were identified and new descriptors added:
- competency 1, domain 1: Supporting women, babies and their families (existing descriptor split into 3 levels)
- new descriptor to incorporate dealing with conflict
Part 2: roles, education and career progression
Support worker roles in maternity settings
Support workers provide care to mothers, their newborn infants and their families through pregnancy, labour and during the postnatal period. Their role can be integral to the successful deployment of maternity transformation projects (RCM, 2017) and their contribution maximised through appropriate training, role alignment and MDT participation (RCM, 2018).
To confidently and capably deliver care, support workers must acquire a level of knowledge, competence and skills specific to the population they serve. Following appropriate preparation, they can deliver elements of healthcare and undertake clinical work under supervision or independently within agreed standard operating procedures, as identified within the Skills for Health Career Framework (2010).
Traditionally, support workers in maternity settings have assisted midwives. This framework recognises that they work as members of the wider MDT, assisting and reporting to a range of other practitioners in accordance with the duties they are undertaking. The role of support workers in maternity settings should therefore be recognised and valued in their own right.
All support worker roles should have role descriptors which reflect the scope and level of responsibility expected of the post holder. Similarly, job descriptions should be regularly reviewed to ensure that development and career progression is being supported. Dependent on role and level of preparation support workers in maternity settings may:
- support the work of registered and non-registered practitioners
- work under direct or indirect supervision, and/or as lone workers, where appropriate
- work across service settings and professional boundaries, according to the needs of women, their newborn infants and their families and local service provision (adapted from Skills for Health, 2018)
Domains of support worker practice in maternity settings
As progressive and innovative provision emerges to transform maternity services, so does the opportunity to position support workers as integral members of maternity teams that prioritise holistic, safe and personalised care. Central to this is the need to define the scope and role of their future practice.
The 4 domains below represent broad areas of practice for support workers in maternity settings.
- supporting women and families
- public health: prevention and health promotion
- personal and clinical skills
- creating safe environments
The domains provide a framework for competencies, detailing the minimum standard of practice expected of post holders to safely perform their role. The competencies at levels 2, 3 and 4 determine and describe the difference in knowledge, skills, values and behaviours according to the level of their role specification. The levels used mirror those in the Skills for Health Career Framework (2010), as below.
| Level 2 | Level 3 | Level 4 |
|---|---|---|
| People at level 2 require basic factual knowledge of a field of work. They may carry out clinical, technical, scientific or administrative duties according to established protocols or procedures, or systems of work. | People at level 3 require knowledge of facts, principles, processes, and general concepts in a field of work. They may carry out a wider range of duties than the person working at level 2, and will have more responsibility, with guidance and supervision available when needed. They will contribute to service development and are responsible for self-development. | People at level 4 require factual and theoretical knowledge in broad contexts within a field of work. Work is guided by standard operating procedures, protocols or systems of work, but the worker makes judgements, plans activities, contributes to service development and demonstrates self-development. They may have responsibility for supervision of some staff. |
Role titles and descriptors
Historically, support workers have had numerous titles associated with their roles. For consistency, the following titles are recommended and will be used in this framework:
- Level 2 maternity care assistant (MCA)
- Level 3 maternity support worker (MSW)
- Level 4 assistant practitioner (AP) (maternity)
The role descriptors below identify the scope of role for support workers at levels 2, 3 and 4 and highlight some of the typical responsibilities and activities that could be undertaken at each level, allowing differentiation between roles and consistency of application across services.
The descriptors use the Skills for Health (2018) role directory tool. They should be used by employers to shape a job description for a post they wish to fill, or to inform decisions regarding the deployment of MCAs, MSWs and APs (maternity) within current or emerging care structures.
The exemplar role titles, role descriptors and accompanying responsibilities are not considered exhaustive and do not constitute a job description or person specification. Instead, employers should use the role titles and descriptors to inform decisions about the level of responsibility a post holder could have, to reflect the set of circumstances in which a person could be working. To support this work, employers are advised to use the MSW implementation and mapping toolkit. It is important to note that the career and educational levels and role descriptors detailed within this framework do not directly correspond to Agenda for Change banding. This requires employer led job evaluation.
Role descriptor: Level 2 maternity care assistant
Level 2 MCA: Uses general skills to enhance the service offered to women and their newborn infants and families across a range of aspects of maternity service delivery under the close supervision of a registrant ordinarily a midwife, or a Level 4 AP (maternity).
Scope of role: Level 2 MCAs possess the minimum level education and competency requirements to work safely under the direction of registered practitioners and other members of the maternity service team who provide direct delivery of care to women and newborn infants accessing hospital-based services. Level 2 MCAs may undertake delegated, basic care tasks as part of routine care for women and their newborn infants, if they have been appropriately trained. Where they do so, they will follow planned care and support programmes while being closely supervised by a registered or Level 4 practitioner.
Leadership: the role holder will take responsibility for improvements in their own performance within familiar work contexts and will support changes and improvements within maternity services. They take responsibility for the completion of tasks that are delegated to them.
Contextual knowledge: the role holder can recall, comprehend, and make use of basic facts, processes, and core ideas. They have an underlying awareness of public health and health promotion initiatives, policy and legislation, and of ethical and legal issues relevant to the scope of their role.
Process knowledge: the role holder can solve routine problems and make straightforward judgements within familiar areas of practice. They can solve limited problems using simple rules and tools, escalating concerns when necessary. They can perform basic care, technical, administrative, or clinical tasks in a narrow and defined area. They will be required to record information in appropriate documentation, including where support has been sought from suitably qualified practitioners or where concerns have been escalated. They will hold responsibility for the care of equipment and resources used by the team in which they work. They can perform simple audits or surveys relevant to their work area.
Personal and professional values and behaviours: the role holder will demonstrate self-directed development to ensure they are able to practise in accordance with established protocols and standard operating procedures under close, but not continuous, supervision. They recognise the importance of positioning women and their newborn infants and families at the centre of care. Within the scope of their role, they recognise their limitations and present themselves in a credible and competent manner at all times.
Activities may include: supporting the smooth running of maternity services including clinics, day assessment and maternity triage by locating and filing notes, preparing documentation, general housekeeping, stock rotation and ordering; undertake basic care tasks including supporting hydration and nutrition needs of women and their newborn infants, documenting hydration and micturition on fluid balance charts; preparing women for clinical examination and tests, screening and immunisations; and acting as a chaperone. required
Role descriptor: Level 3 maternity support worker
Level 3 MSW: Uses additional skills within focused aspects of service delivery to enhance the service offered to women and their newborn infants and families; working alongside, but under the guidance of practitioners at all levels from across the maternity multidisciplinary team including, but not limited to: obstetricians; midwives; ultra-sonographers; physiotherapists; and advanced clinical practitioners.
Scope of the role: Level 3 MSWs provide direct delivery of clinical care to all women and newborn infants accessing maternity services and may be based within specialist and integrated teams such as in theatre, fetal medicine units and community hubs. Level 3 MSWs may serve as a point of contact for women and their families and provide clinical, physical, psychological and emotional care and support; they provide appropriate information and signpost to other health sector organisations. They report directly to registered practitioners where planned care and tasks delegated by a registered or level 4 practitioner has been provided.
Leadership: the role holder reflects on and actively seeks ways to maintain and improve their own performance. They demonstrate qualities of leadership, identifying risks and taking appropriate action, supporting change management, and offering suggestions for service improvement. They prioritise their own workload to ensure timely completion of tasks delegated to them, reporting to registered practitioners and documenting outcomes of care offered and/or provided.
Contextual knowledge: the role holder possesses generalised knowledge to inform understanding of their duties, and specific knowledge related to tasks or activities within their scope of role. This includes awareness of the role and duties of other professionals. Through their practice, they demonstrate an awareness of public health and health promotion initiatives, policy and legislation, local and national standards and protocols, and legal and ethical issues relevant to the scope of their role.
Process knowledge: the role holder can make fact-based judgements requiring a comparison of options to effectively perform tasks and activities. They will undertake well defined, familiar tasks. In some instances, workload will include some complexity, but supervision and guidance are available to assure safety. The role holder will demonstrate effective application of problem solving and planning skills and a broad skill base related to their practice. They will be able to document care appropriately, detailing actions taken, where support has been sought from suitably qualified practitioners or where concerns have been escalated. They engage in, promote and support others to undertake routine audits or surveys relevant to their work.
Personal and professional values and behaviours: the role holder can independently plan tasks and workload activities while ensuring that their practice is guided by standard operating procedures and established protocols. Their practice will reflect the principles of personalised care to promote the health and wellbeing of women, their newborn infants and families. They will demonstrate self-directed development, recognising the limits of their own competence, and work within the scope of their role at all times. They will prioritise their own workload and may be responsible for planned care and tasks delegated from a registered or Level 4 practitioner. Depending upon the level of complexity and risk present, the role holder may exercise an appropriate degree of autonomy, ensuring they present themselves in a credible and competent manner at all times.
Activities include: (in addition to that of the Level 2 care assistant) routine maternal and neonatal monitoring including clinical observations such as blood pressure, temperature, respirations, urinalysis, weighing, maternal and neonatal phlebotomy, infant feeding support, leading and supporting routine clinics for example glucose tolerance testing, public health promotion and education either as a group or on a one-to-one basis, including antenatal classes.
Role descriptor: Level 4 assistant practitioner (maternity)
Level 4 AP (maternity): Uses enhanced skills across the range of maternity services to support specialist and multi-disciplinary teams including, but not limited to: midwives, health visitors, safeguarding leads, mental health nurses, psychologists, psychiatrists, social workers, general practitioners, prison officers, advanced clinical practitioners and other key and peer-support workers.
Scope of the role: APs (maternity) support the delivery of integrated maternity services to women, their newborn infants and families during pregnancy, labour and the postnatal period. The role holder will liaise with a number of community and hospital-based services to enhance the service offered to women, their newborn infants and families through the direct delivery of care, and as a point of contact for support or signposting. Level 4 APs (maternity) are key members of the maternity team, providing support to women, newborn infants and families who have complex care and support needs.
Leadership: the role holder can delegate tasks appropriately to MCAs and MSWs working at levels 2 and 3 and may have day-to-day supervisory responsibilities and line management responsibility for them, as determined by their employer. They are able to evaluate their own and other’s practice and suggest and implement changes to improve service delivery.
Contextual knowledge: the role holder will have a detailed knowledge of the scope of their role and that of others within the multidisciplinary team. This will include cross professional knowledge which will enhance multidisciplinary team working. Through their practice, they will apply a working knowledge of public health and health promotion initiatives, legal and ethical frameworks, and demonstrate understanding of wider health and social care issues and policy that impacts upon service delivery and provision.
Process knowledge: the role holder will have enhanced skills in their area of work, which may include specialist practice areas. They will demonstrate a high degree of technical proficiency and contextual knowledge while undertaking both routine and more complex tasks and activities. They will make judgements requiring comparison and evaluation of options to inform decision making and effectively perform their role. They will be required to document appropriately, detailing actions taken, where support has been sought from suitably qualified practitioners, referrals have been made or where concerns have been escalated. They engage in, recommend, promote and lead audits or surveys to support service improvement.
Personal and professional values and behaviours: the role holder will be able to independently plan individual and team tasks or activities, prioritising own workload and ensuring effective and appropriate delegation and referral to others. They will apply and promote the principles of personalised care in all aspects of their practice. They will demonstrate self-directed development, working within standard operating procedures, protocols and their scope of role at all times. They will assume the role of mentor or teacher within their area of practice and in relation to the scope of the other’s role. Recognising limitations within their own role and practice, the Level 4 AP (maternity) will exercise appropriate autonomy and present themselves in a credible and competent manner at all times.
Activities include: (in addition to that of a Level 3 MSW) planning care in partnership with women and registered practitioners, training and teaching, appraisals, providing advice to support discharge of women and newborn infants from maternity care settings, providing specialist support to women, newborn infants and families with complex needs, leading and coordinating support worker teams and service improvement initiatives.
Employers and support workers should use the MSW implementation and mapping toolkit to support the development and implementation of support worker roles in maternity settings.
Education and training
The framework takes account of the characteristics of the existing workforce, as well as the future workforce and supports organisations to accept a wide diversity of entry qualifications and/or equivalent experience. T-Levels are recognised within the framework. These qualifications offer equivalence to three A Levels and furnish students with technical knowledge and practical skills specific to their chosen industry or occupation (DH, 2018).
Additional education and training for existing support workers in maternity settings should be offered to enable them to demonstrate occupational competence. This may include bespoke, inhouse bridging programmes which use the MSW voluntary curriculum or NHS England’s MSW e-learning modules to support transition requirements. All programmes of study should ensure support workers develop specific knowledge and skills related to maternity care and, where possible, allow this group of MSWs to operate on a par with new entrants, to progress through the framework and to step into higher education programmes if they so wish.
The model adheres to the following set of principles:
- employers should recognise transferable skills and competencies
- education should be work based and employer led
- education entry and exit points should be recognised for their merit to support progression
- support workers should be enabled to participate in CPD to develop within their role, and progression routes should be available
- when in training, support workers should be recognised as learners and supported to develop their confidence and newly acquired skills (Skills for Health 2018)
The tables below provide the:
- entry criteria for levels 2, 3 and 4 based on:
- academic qualifications, and/or clinical experience
- capability in relation to values
- education and development pathways for levels 2, 3 and 4
- academic exit and employer outcome requirements to fulfil the role at levels 2, 3 and 4.
Figure 6 illustrates how NHS staff can progress from level 2 to level 3, from level 3 to level 4 and, potentially, beyond into specialist roles, higher education or pre-registration midwifery education. Employers and support workers should use the MSW implementation and mapping toolkit to support implementation of the educational framework.
Entry requirements and educational outcomes
Level 2 MCA
| Entry requirements | Education pathway | Educational and employer outcome requirements |
|---|---|---|
| Experience: Minimal clinical experience within health and social care settings and/or Qualifications * GCSE English and maths (or equivalent) or willingness to undertake Level 2 functional skills and Capability: Evidence values associated with NHS Constitution and a commitment to L2 role development | Intermediate Apprenticeship (Level 2: Healthcare Support Worker) ** or Local training packages with appropriate maternity focus *** plus L2 Functional skills * plus Care certificate | Level 2 Diploma in Healthcare or Other suitable academic preparation to ensure knowledge and understanding related to role at level 2 plus Level 2 English and maths (GCSE or equivalent) Care certificate Able to evidence level 2 requirements of competency framework |
*Level 2 functional skills not required if able to evidence English and maths GCSE
**Intermediate apprenticeship may not be required if applicant can evidence science/biology GCSEs or A-levels
***Local training packages to prepare MCAs to evidence level 2 requirements of competency framework and care certificate may be used for MCAs already in post or new entrants who have science/ biology GCSEs or A levels
Level 3 MSW
| Entry requirements | Education pathway | Educational and employer outcome requirements |
|---|---|---|
| Experience: Previous clinical experience within health and social care settings relevant to role and/or Qualifications * GCSE English and maths (or equivalent) or willingness to undertake Level 2 functional skills and Capability: Evidence values associated with NHS Constitution and commitment to L3 role development | Advanced Level Apprenticeship Level 3 (Senior Health Care Support Worker: Maternity Support) ** or Local or national training packages (such as NHS England’s MSW modules) with appropriate maternity focus *** plus L2 Functional skills * plus Care certificate | Level 3/ 4 qualification relevant to role of MSW or Other suitable academic preparation to ensure knowledge and understanding related to role at level 3 plus Level 2 English and maths (GCSE or equivalent) Care certificate Able to evidence level 3 requirements of competency framework |
*Level 2 functional skills not required if able to evidence English and Maths GCSE
**Advanced Level Apprenticeship Level 3 (Senior Health Care Support Worker: Maternity Support) may not be required if applicant can evidence science/biology A-levels or Health and Science T-level or a Certificate of Higher Education (following successful completion of year one of a pre-registration midwifery programme) or if they are already in role as a level 3 MSW
***Local or national training packages to prepare MSWs to evidence level 3 requirements of competency framework may be used for MSWs already in post or new entrants who have appropriate qualifications at level 3 or above.
Level 4 AP (maternity)
| Entry requirements | Education pathway | Educational and employer outcome requirements |
|---|---|---|
| Experience: Significant clinical experience within health and social care settings relevant to role and Qualifications* A minimum of 2 A Levels, or a Health and Science T-level or a Certificate of Higher Education (following successful completion of year one of a pre-registration midwifery GCSE English and maths (or equivalent) or willingness to undertake Level 2 functional skills and Capability: Evidence values associated with NHS Constitution and commitment to L4 role development | Higher Apprenticeship (Level 5: AP with appropriate maternity focus) ** or FdSc Health and Social care with appropriate maternity focus **** or Local or national training packages (such as NHS England’s MSW modules) with appropriate maternity focus *** plus L2 Functional skills* plus Care certificate | RQF Level 5 qualification relevant to role of MSW or Other suitable academic preparation to ensure knowledge and understanding related to role at level 4 plus Level 2 English and maths (GCSE or equivalent) Care certificate Able to evidence level 4 requirements of competency framework |
* Level 2 functional skills not required if able to evidence English and maths GCSE
** Higher Apprenticeship may not be required if applicant can evidence FdSc or DipHE Health and Social Care or a Dip HE with appropriate maternity focus or following successful completion of year 1 and 2 of a pre-registration midwifery programme or if they are already in role as a level 4 MSW
***Local or national training packages to prepare AP (Maternity) to evidence level 4 requirements of competency framework
**** FdSc Health and Social care qualifications must have an appropriate maternity focus.
Progression
Figure 1: Progression through levels 2, 3 and 4 for MCAs, MSWs and APs (maternity) employed by NHS trusts
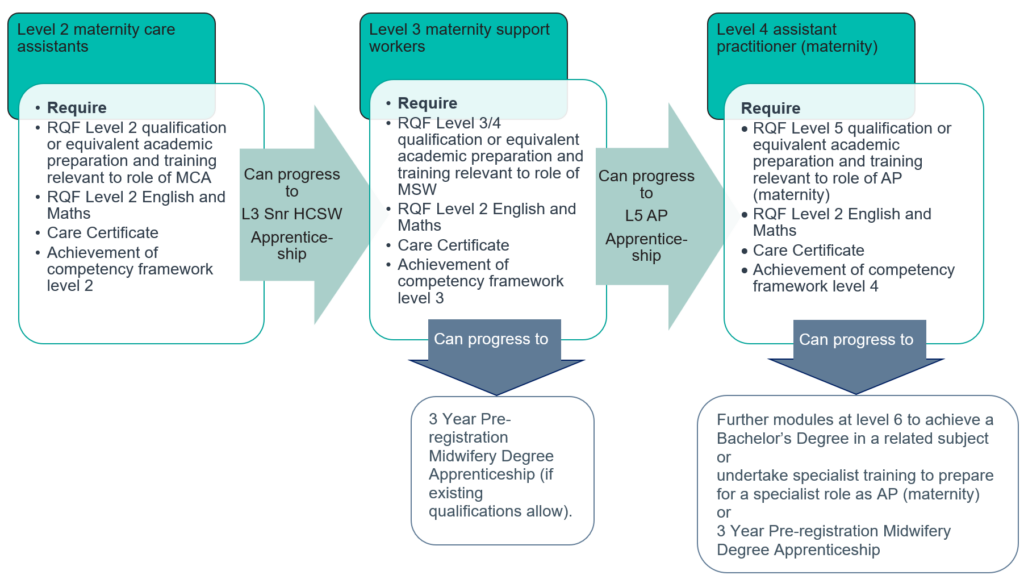
Figure 1 image text:
Level 2 maternity care assistants
Require:
- RQF Level 2 qualification or equivalent academic preparation and training relevant to role of MCA
- RQF Level 2 English and Maths
- Care Certificate
- Achievement of competency framework level 2
Can progress to L3 Snr HCSW apprenticeship
Level 3 maternity support workers
Require:
- RQF Level 3/4 qualification or equivalent academic preparation and training relevant to role of MSW
- RQF Level 2 English and Maths
- Care Certificate
- Achievement of competency framework level 3
Can progress to:
- L5 assistant practitioner apprenticeship
- 3 Year Pre-registration Midwifery Degree Apprenticeship (if existing qualifications allow).
Level 4 assistant practitioner (maternity)
Require:
- RQF Level 5 qualification or equivalent academic preparation and training relevant to role of AP (maternity)
- RQF Level 2 English and Maths
- Care Certificate
- Achievement of competency framework level 4
Can progress to:
- further modules at level 6 to achieve a Bachelor’s Degree in a related subject or
- undertake specialist training to prepare for a specialist role as AP (maternity) or
- 3 Year Pre-registration Midwifery Degree Apprenticeship
All MCAs, MSWs and AP (maternity) should participate in continuing professional development to ensure they maintain required knowledge and skills, as well as being offered the opportunity to develop in their role.
Where MSWs want to make the transition to being a registered midwife, NHS employers should work with Midwifery Degree Apprenticeship providers to determine what experience and qualifications MSWs at level 3 require to step onto these programme, as a potential alternative to undertaking an Access to HE programme.
Note: RQF is the UK’s regulated qualifications framework.
- Level 2 is equivalent to GCSEs
- Level 3 is equivalent to A-Levels and T-Levels
- Level 4 is equivalent to a Certificate of Higher Education
- Level 5 is equivalent to a Diploma of Higher Education or a Foundation Degree
- Level 6 is equivalent to a Bachelor’s degree
Part 3: competencies and indicators
This framework provides MCAs, MSWs and APs (maternity) and their employers with an understanding of the expected minimum level of knowledge, skills, values and behaviours of those practising within each level of the framework. Grouped under the 4 domains of MSW practice, competencies are expressed at levels 2, 3 and 4, mirroring role descriptor levels, as mapped to the Skills for Health Career Framework (2010). The framework allows the developmental and experiential journey of MCAs, MSWs and APs (maternity) to be recognised. Those entering at level 3 of the framework would also be expected to demonstrate, through their practice, competence at level 2 and, similarly, those entering at level 4 would be expected to demonstrate that they also hold competence at levels 2 and 3.
Each competency within the framework is underpinned by a number and range of indicators. These guide support workers and those undertaking assessments of their competence.
Supervision and assessment of competence
Until competence is achieved and signed off, the trainee MCAs, MSWs and APs (maternity) should be directly or indirectly supervised by an appropriately qualified practitioner, as determined by the employer. Direct supervision involves close proximity to the trainee to enable direct working or direct monitoring of their activities. Indirect supervision is appropriate at the point at which the trainee needs consolidation of skills and confidence building to enable independent working. The principles of delegation should be considered to ensure the safety and wellbeing of women, their newborn infants and families, as well as other staff, and the trainee themselves, and applied in line with professional body requirements. Competency can be assessed by an appropriately qualified practitioner, as determined by the employer. Multiple forms of evidence can be considered and used to demonstrate competence, but this must be subject to quality assurance processes.
When assessing competence, consideration should be given to how the support worker might:
Know it: Demonstrate their knowledge
Show it: Demonstrate their skills
Live it: Demonstrate appropriate attitudes and behaviours
Reflect: Demonstrate their ability to reflect on their own practice and on feedback given
(adapted from Institute of Apprenticeships 2018)
Employers and support workers in maternity services should use the MSW implementation and mapping toolkit for support in assessing competencies and indicators.
Domain 1: Supporting women, their babies and families
How you support women, their newborn infants and families, providing care throughout their maternity journey
Competency 1: Create effective and supportive relationships with women and their families to enhance the provision of personalised and safe care
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
Indicator 1 Positive relationships | Develops, manages and maintains positive, appropriate relationships with women, their partners, families and carers, demonstrating respect, kindness, compassion and empathy at all times |
Develops, manages and maintains positive, appropriate relationships with women, their partners, families and carers, demonstrating respect, kindness, compassion and empathy at all times |
Develops, manages and maintains positive, appropriate relationships with women, their partners, families and carers, demonstrating respect, kindness, compassion and empathy at all times |
Indicator 2 Woman-centred care |
Provides woman-centred, personalised care and support |
Demonstrates understanding of the importance of working in partnership with women and their families, of providing education and resources to support informed decision making, and of respecting their decisions |
Consistently employs strategies to promote personalised, informed decision-making when planning, implementing and evaluating care activities. Tailors information to meet the needs of women, including where complex care and support needs exist |
Indicator 3 Empowering others |
Shares knowledge and teaches skills that empower women and their families to safely and effectively care for themselves |
Supports registered health practitioners to implement strategies that engage woman and partners in self-care and in the care of their newborn infant |
Develops and implements strategies, within scope of role, that encourage women and their partners to optimise self-care, care of their newborn infant and parenting |
Indicator 4 Consent |
Understands and gains valid consent prior to action or providing care |
Understands and gains valid consent prior to action or providing care |
Understands and gains valid consent prior to action or providing care |
Competency 2: Understands their scope-of-practice and works within limits of own competence and within agreed ways of working | |||
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Acts with integrity |
Is trustworthy, focuses on the needs of women and their families, takes ownership of mistakes and reports errors to a registered practitioner in a timely manner |
Understands the principles of duty of care and human rights and applies these to ensure individuals do not come to harm. Represents known preferences of women to the MDT to inform care planning, within scope of role |
Demonstrates leadership by advocating with or on behalf of women, their families and/or colleagues, within scope of role |
|
Indicator 2 Professionalism |
Recognises the importance of MCA roles within national frameworks for health and care and acts in a professional manner, demonstrating NHS Constitution values |
Recognises the importance of the role of the MSW within national frameworks for maternity care. Understands the additional responsibilities associated with being self-directed when carrying out tasks, giving advice and in updating the MDT |
Understands own responsibility and accountability when forming a judgement of an individual’s health, wellbeing, or social condition, uses factual and theoretical knowledge as a basis for decision making, and escalates concerns appropriately to the MDT |
|
Indicator 3 Implementing care |
Understands the importance of following standard operating procedures, protocols, policies and guidelines to promote the safety, health and wellbeing of individuals |
Implements agreed care plans in line with guidance, standard operating procedures, policy and protocols, as directed by the MDT, with agreement from the woman and, where appropriate, their family |
Within scope of role and practice, discusses care plans with women prior to implementation, offering an informed perspective and an evidence-base to optimise a personalised experience |
|
Indicator 4 Reporting, referring and escalating concerns |
Recognises and responds to signs of pain, discomfort, distress and anxiety, or concerns raised by women and their families, by promptly reporting them to an appropriate practitioner |
Uses knowledge and understanding of common physical, mental and behavioural health conditions and the role of prescribed medication within maternity care to recognise changes or signs of deterioration in women and babies. Responds by promptly escalating concerns to an appropriately registered practitioner |
Gathers and interprets relevant information and forms a judgement on the improvement or deterioration in the physical, mental or behavioural condition of women or babies. Responds by referring or escalating concerns to an appropriately registered practitioner |
| Competency 3: Contribute positively to a culture of team working, maintaining effective working relationships to maximise quality of care | |||
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Planning and evaluating care |
Assists in effective care planning and evaluation by sharing relevant information in a timely manner with members of the MDT |
Offers comments or suggestions to the MDT when developing, reviewing and evaluating care plans based on objective evidence and experience |
As a member of the MDT, actively participates in the planning, development and evaluation of personalised care plans by offering objective clinical or evidence-based information to inform planned activities |
|
Indicator 2 Team working |
Understands the principles of team working and can define own role and the roles of others. Asks for guidance and help when unsure |
Understands the principles of human and environmental factors when working in teams and applies these to contribute to safe team working |
Understands the challenges of providing integrated care for women and their families. As a key member of the team demonstrates initiative and leadership where required |
|
Indicator 3 Continuity of carer |
Understands the benefits of continuity of carer for women and their families and how this applies within own role |
Ensures that the principles of continuity of carer are employed when supporting women and their families and when escalating or sharing clinically relevant information |
Consistently applies the principles of continuity of carer when making judgements related to supporting women with complex needs and when referring or transferring care back or on to registered practitioners or specialist teams
|
| Competency 4: Notice and respond appropriately to the changing needs of the individual and their family | |||
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3)
|
|
Indicator 1 Safeguarding |
Understands and follows the principles of safeguarding and protection, to include adhering to local security procedures |
Is vigilant for cues indicating safeguarding issues related to women and families. Escalates safeguarding concerns and reports to the MDT in a robust, timely manner, complying with legal requirements |
Independently undertakes agreed risk identification and assessment activity, within scope of role and practice, in accordance with local and national safeguarding pathways |
|
Indicator 2 Signposting |
Directs queries regarding local and national services to support women and families to a suitably qualified colleague to take forward |
Maintains a working knowledge of local and national support systems available to women, their babies and families. Uses this knowledge to signpost women and families effectively |
As a key member of the MDT, arranges access to services to support personalised care plans, referring women, their babies and their families to agencies and services appropriately |
|
Indicator 3 Supporting vulnerable women, families and those with additional needs |
Notices vulnerability, changing or additional needs and reports these to a suitably qualified colleague to take forward |
Understands and is vigilant against factors that indicate vulnerability, changing or additional needs. Directs women to appropriate practitioners within the MDT for support, while escalating concerns |
As a member of the MDT, within scope of role and practice, undertakes assessments, manages and supports the implementation and evaluation of care plans for vulnerable women, their babies and families and those with additional needs |
|
Indicator 4 Caring for the family unit |
Acts sensitively, compassionately and respectfully in situations where the family unit is separated and/or where mothers and/or babies are critically ill, making sure updates and information sharing with affected family members is accurate and relayed by the appropriate team member. Ensures tasks which separate families are kept to a minimum and are carried out with kindness and empathy |
Acts sensitively, compassionately and respectfully in situations where the family unit is separated and/or where mothers and/or babies are critically ill, making sure updates and information sharing with affected family members is accurate and relayed by the appropriate team member. Ensures tasks which separate families are kept to a minimum and are carried out with kindness and empathy |
Acts sensitively, compassionately and respectfully in situations where the family unit is separated and/or where mothers and/or babies are critically ill, making sure updates and information sharing with affected family members is accurate and relayed by the appropriate team member. Ensures tasks which separate families are kept to a minimum and are carried out with kindness and empathy |
|
Indicator 5 Bereavement and loss |
Acts sensitively, compassionately and respectfully during times of bereavement or loss. Seeks out preferences of bereaved women, partners and families before providing care and follows bereavement care plans/ pathways, within scope of the role |
Acts sensitively, compassionately and respectfully during times of bereavement or loss. Seeks out preferences of bereaved women, partners and families before providing care and follows bereavement care plans/ pathways, within scope of the role |
Acts sensitively, compassionately and respectfully during times of bereavement or loss. Seeks out preferences of bereaved women, partners and families before providing care and follows bereavement care plans/ pathways, within scope of the role |
Domain 2: Public health: prevention and health promotion
How you support women and families to make healthy choices
Competency 5: Promote a culture of health and wellbeing by providing information, advice and support to enable healthy lifestyle choices for all individuals, while understanding the causes of ill-health related to women and their families
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Influences on public health |
Understands that social and cultural influences, individual circumstances, capabilities, behaviours and lifestyle choices impact on health and wellbeing outcomes |
Understands that social and cultural influences, individual circumstances, capabilities, behaviours and lifestyle choices impact on health and wellbeing outcomes |
Understands that social and cultural influences, individual circumstances, capabilities, behaviours and lifestyle choices impact on health and wellbeing outcomes |
|
Indicator 2 Public health promotion |
Understands the aims and principles of health promotion, protection and improvement and the importance of related strategies |
Understands the aims and principles of health promotion, protection and improvement and the importance of related strategies |
Understands the aims and principles of health promotion, protection and improvement and the importance of related strategies |
|
Indicator 3 Makes every contact count |
Appreciates the importance of recognising and supporting physical and emotional health and wellbeing and makes every contact count by actively encouraging women and their families to talk about their health and wellbeing |
Appreciates the importance of recognising and supporting physical and emotional health and wellbeing and makes every contact count by actively encouraging women and their families to talk about their health and wellbeing |
Appreciates the importance of recognising and supporting physical and emotional health and wellbeing and makes every contact count by actively encouraging women and their families to talk about their health and wellbeing |
|
Indicator 4 Supporting behaviour change |
Seeks support from a suitably qualified practitioner when women or members of their family signal a desire to make behaviour changes that can impact on health and wellbeing |
Understands the principles of behaviour change and interventions to prevent ill-health and effectively applies these to practice and personalises the individual’s right to privacy and choice |
Applies principles of behaviour change within personalised contexts to enable personalised discussion, sensitively communicating complex, and/or potentially challenging information to women, if appropriate, to facilitate change |
|
Indicator 5 Personal health and wellbeing |
Recognises the importance of maintaining own health, wellbeing and resilience to ensure that personal performance and judgement is not affected by ill-health |
Recognises the importance of maintaining own health, wellbeing and resilience to ensure that personal performance and judgement is not affected by ill-health |
Recognises the importance of maintaining own health, wellbeing and resilience to ensure that personal performance and judgement is not affected by ill-health |
|
Competency 6: Actively engage with public health initiatives
| |||
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Screening |
Assists in preparing the environment, women and their families for screening activities |
Maintains a knowledge base about local and national antenatal and newborn screening services and directs women and their families to appropriately qualified practitioners if they are undecided or have concerns |
Understands the importance of health screening, and, within scope of role, can assist in the provision of evidence-based information, advice and guidance to enhance choice and consent for participation in national antenatal and newborn screening programmes |
|
Indicator 2 Immunisation |
Assists in preparing the environment, women and their families for immunisations |
Maintains a knowledge base about immunisations offered during pregnancy and to the newborn and directs women and their families to appropriately qualified practitioners if they are undecided or have concerns |
Understands why individual, herd, passive and active immunity acquisition are important and, within scope of role, assists in providing evidence-based information, advice and guidance to enhance choice and consent for participation in common immunisation programmes |
|
Indicator 3 Infant feeding |
In line with baby friendly principles, supports an individual’s choices for infant feeding as part of the MDT |
Assists women and their families with responsive infant feeding, helping them to gain skills and confidence with positioning and attachment. Maintains comprehensive knowledge about infant feeding, to include understanding safety and risk issues and appropriate referral |
Independently provides evidence-based information, advice and guidance to optimise infant feeding and the health and wellbeing of the mother and their family. Evaluates the progress of women and babies on identified infant feeding pathways and enacts adjustments using own judgement, updating the MDT of changes agreed |
Domain 3: Personal and clinical skills
How you develop and use your skills to care for women, their babies and their families
Competency 7: Provide and monitor care safely and effectively
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Safe practice |
Demonstrates safe, evidence-based practice in all skills and procedures stated within job description |
Demonstrates safe, evidence-based practice in all skills and procedures stated within job description |
Demonstrates safe, evidence-based practice in all skills and procedures stated within job description |
|
Indicator 2 Time management |
Manages tasks effectively to ensure timely completion |
Demonstrates ability to manage own time and workload effectively |
Recognises where elements of care can be appropriately delegated to other colleagues, or entrusted to women or family members to support effective time management and safe care |
|
Indicator 3 Providing care |
Accurately undertakes delegated tasks, for which they have received training, ensuring basic care needs of women and babies are met. Reports completion of the task and any findings to an appropriately qualified practitioner |
Uses a range of clinical information and associated knowledge of normal baseline observations in women and babies to confirm wellbeing, reporting findings to a registered practitioner and escalating where wellbeing is not confirmed |
Working as a member of the MDT, uses a range of clinical information to inform a judgment on the effectiveness of an existing care plan and the requirement to immediately escalate concerns to a registered practitioner or to make a referral back to the MDT for review |
|
Indicator 4 Prioritising care |
Demonstrates the ability to respond flexibly to the needs of the working environment |
Can prioritise care activities to meet the holistic needs of individual women and their families, including adjusting normal routines where levels of complexity exist |
Understands the impact of complex care needs and other factors when prioritising care activities across a group of women or babies within their own or the team’s defined workload |
|
Indicator 5 Emergency care |
Recognises an obstetric or neonatal emergency, summons assistance and acts as a member of the MDT within parameters of own competence and defined role. In settings where a registered practitioner is not present, initiates immediate first aid while awaiting the arrival of appropriately qualified practitioners |
Recognises an obstetric or neonatal emergency, summons assistance and acts as a member of the MDT within parameters of own competence and defined role. In settings where a registered practitioner is not present, initiates immediate first aid while awaiting the arrival of appropriately qualified practitioners |
Recognises an obstetric or neonatal emergency, summons assistance and acts as a member of the MDT within parameters of own competence and defined role. In settings where a registered practitioner is not present, initiates immediate first aid while awaiting the arrival of appropriately qualified practitioners |
|
Competency 8: Communicate clearly and accurately using a range of written, verbal and non-verbal methods, maintaining confidentially and upholding the principles of data protection at all times
| |||
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Confidentiality and data protection |
Understands the importance of accessing, maintaining and storing documentation relating to care, in accordance with local guidance and with legal requirements for maintaining confidentiality and data protection |
Understands the importance of accessing, maintaining and storing documentation relating to care, in accordance with local guidance and with legal requirements for maintaining confidentiality and data protection |
Understands the importance of accessing, maintaining and storing documentation relating to care, in accordance with local guidance and with legal requirements for maintaining confidentiality and data protection |
|
Indicator 2 Record keeping |
Keeps complete, clear, accurate and timely records, using digital platforms as required |
Keeps complete, clear, accurate and timely records, using digital platforms as required |
Keeps complete, clear, accurate and timely records, using digital platforms as required |
|
Indicator 3 Methods of communication |
Communicates respectfully with women, their families and colleagues at all times, using verbal and non-verbal communication skills |
Selects appropriate methods of communication, taking account of the circumstances and needs of women and their families; including where disability or complexity may exist |
Uses judgement to select and use appropriate technology and other communication aids to support women to be active participants in their care experience |
|
Indicator 4 Effective communication |
Communicates information clearly, effectively and in a timely way to women, their families and the wider MDT |
Checks understanding by using mechanisms such as clarifying and reflecting back meaning and instruction prior to carrying out tasks and when reporting back to colleagues |
Communicates complex information in a clear, accurate, unambiguous and timely manner to women and their families and across the MDT, checking understanding by using mechanisms such as clarifying and reflecting back |
|
Competency 9: Maintain and further develop own knowledge, skills and behaviours, and contribute to the development of others, through training and education to include local mandatory training
| |||
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Undertakes training |
Identifies training requirements relevant to role, including identifying and undertaking mandatory training when required |
Identifies training requirements relevant to role, including identifying and undertaking mandatory training when required |
Identifies training requirements relevant to role, including identifying and undertaking mandatory training when required |
|
Indicator 2 Maintains knowledge |
Maintains and develops own skills and knowledge. Keeps evidence of personal development, prepares for and participates in appraisal |
Explains the importance of maintaining a knowledge base and skill set to ensure safe care, including demonstrating the skill of critically appraising and applying sources of information to inform own practice |
Explains the importance of using good-quality research to inform evidence-based practice and of lifelong-learning in maintaining an awareness of best-practice |
|
Indicator 3 Seeking feedback and reflection |
Takes responsibility for and reflects on own actions while working within the context of the team providing safe and effective care |
Responds appropriately to constructive feedback, reflects and evaluates own performance as means of enhancing and improving own practice |
Actively seeks feedback related to personal performance to enhance own practice. Provides constructive feedback to others to enhance team performance
|
|
Competency 10: Participate in the training and supervision of staff within the scope of the role, in collaboration with the multi-disciplinary team | |||
|
SfH Career Framework Level |
Level 2 (In addition to Care Certificate) |
Level 3 (In addition to achieving full competence at Level 2) |
Level 4 (In addition to achieving full competence at Levels 2 and 3) |
|
Indicator 1 Role modelling |
Is always welcoming and takes an interest in the education and development of others |
Understands the importance of role modelling to uphold the reputation of fellow MSWs and in supporting the development of others |
Advocates for MSWs and their development needs in order to fulfil their role and optimize their contribution to maternity services |
|
Indicator 2 Mentorship |
Assists trainee MCAs and trainee MSWs to acquire skills and knowledge |
Participates in the teaching, supervision and assessment of trainee MCAs, trainee MSWs and other healthcare professionals, as required |
Is active in teaching and mentoring trainee MCAs, trainee MSWs and other healthcare professionals, developing resources and activities to support learning |
Domain 4: creating safe environments
How you create safe environments for women, their babies and families, and for yourself and your colleagues.
Competency 11: Work within organisational policies and procedures to ensure maintenance of good quality, safe working practices for women, their families and colleagues
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
| Indicator 1 Organisational values | Is aware of organisational aims, objectives, policies and values that relate to the MCA and MSW role | Can explain how organisational aims, objectives, policies, guidelines and values can affect the provision of health and care for individuals and communities | Actively contributes to the development, application and evaluation of organisational aims, objectives, policies, guidelines and values in practice |
| Indicator 2 Legal and ethical responsibilities | Is aware of legal and ethical responsibilities in relation to own role including the need to work in ways agreed by the employer | Explains the importance of adhering to legislation, standards, policies, protocols, codes of conduct and values that underpin national and local provision of health and care | Contributes to the development of systems to promote knowledge, understanding and adherence to legislation, standards, policies, protocols, codes of conduct and values that underpin national and local provision of health and care |
| Indicator 3 Health and safety | Takes appropriate action in response to local incidents or emergencies, following local health and safety guidance and protocol | Demonstrates awareness of health and safety initiatives and applies appropriate precautions to minimise risk and escalate concerns, including adhering to Lone Worker Policies | Ensures the health and safety of other team members by assuming collective responsibility for team risk assessment, precautions and escalation of concerns |
| Indicator 4 Courage and candour | Understands the importance of courage and candour, recognising and reporting situations, behaviours or errors that could result in poor outcomes for women and their families | Understands the importance of courage and candour, recognising and reporting situations, behaviours or errors that could result in poor outcomes for women and their families | Understands the importance of courage and candour, recognising and reporting situations, behaviours or errors that could result in poor outcomes for women and their families |
| Indicator 5 Recognising and responding to conflict | Can identify potential situations and challenging behaviour that may lead to conflict in the workplace and is able to respond using de-escalation strategies or through prompt reporting and/or calling for assistance. Seeks support and engages in debriefing activity following conflict to support own health and wellbeing | Can identify potential situations and challenging behaviour that may lead to conflict in the workplace and is able to respond using de-escalation strategies or through prompt reporting and/or calling for assistance. Seeks support and engages in debriefing activity following conflict to support own health and wellbeing | Can identify potential situations and challenging behaviour that may lead to conflict in the workplace and is able to respond using de-escalation strategies or through prompt reporting and/or calling for assistance. Seeks support and engages in debriefing activity following conflict to support own health and wellbeing |
Competency 12: Assist in the promotion and maintenance of a safe working environment by using resources efficiently to support the smooth running of the area, having due regard for the health, safety and welfare of women, their babies and families, self and others | |||
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
| Indicator 1 Safe environment | Ensures own actions promote a positive and safe working environment and culture. Including checking the clinical area for hazards and equipment for safety and ensuring that each woman feels safe and knows how to access support if required | Ensures own actions promote a positive and safe working environment and culture. Including checking the clinical area for hazards and equipment for safety and ensuring that each woman feels safe and knows how to access support if required | Ensures own actions promote a positive and safe working environment and culture. Including checking the clinical area for hazards and equipment for safety and ensuring that each woman feels safe and knows how to access support if required |
| Indicator 2 Infection prevention and control | Uses a range of techniques for infection prevention and control | Understands the principles and practices of infection prevention and control, adhering to these consistently within own sphere of practice | Supports others to understand the principles and practices that underpin infection prevention and control principles |
Competency 13: Participate in initiatives to enhance service provision | |||
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
| Indicator 1 Service improvement | Supports audit and service improvement initiatives as directed and keeps abreast of changes in policy and practice | Demonstrates knowledge of, contributes to and promotes service improvement activities such as service user feedback, audit, research, team meetings and benchmarking activities | Leads service improvement activities such as collecting, collating and evaluating service user feedback, audit, research and benchmarking activities, within the MDT |
| Competency 14: Recognise and respect equality and diversity, demonstrating an inclusive approach in all environments | |||
| SfH Career Framework Level | Level 2 (In addition to Care Certificate) | Level 3 (In addition to achieving full competence at Level 2) | Level 4 (In addition to achieving full competence at Levels 2 and 3) |
| Indicator 1 Recognises and reacts to discrimination | Promotes equality and challenges discriminatory behaviour with reference to the protected characteristics of age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation | Promotes equality and challenges discriminatory behaviour with reference to the protected characteristics of age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation | Promotes equality and challenges discriminatory behaviour with reference to the protected characteristics of age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation |
| Indicator 2 Awareness of implicit bias | Does not project own experiences and values onto others and demonstrates understanding of own role and contribution in creating inclusive, equitable care | Does not project own experiences and values onto others and demonstrates understanding of own role and contribution in creating inclusive, equitable care | Does not project own experiences and values onto others and demonstrates understanding of own role and contribution in creating inclusive, equitable care |
| Indicator 3 Respects diversity | Takes account of cultural, religious, social, disability and other factors when undertaking care | Shows an awareness of how women’s personal values, assumptions and vulnerability will impact upon their expectations of care and the choices they make for themselves and their babies | Recognises when a woman’s capacity and/or vulnerability will affect their ability to make decisions about their own or their newborn infant’s care, or to give consent. Understands need to escalate to an appropriately qualified practitioner |
| Indicator 4 Widens access to care | Can apply the principles and processes for making reasonable adjustments and supporting equity of access to care services | Can apply the principles and processes for making reasonable adjustments and supporting equity of access to care services | Can apply the principles and processes for making reasonable adjustments and supporting equity of access to care services |
Glossary
- Accountable: to be responsible and answerable to your employer and yourself for the decisions you make and for your actions or omissions.
- Advocacy: doing your best for individuals by speaking on behalf of another.
- Care: providing what is needed for health and wellbeing through physical, social and emotional support. Taking time and patience to listen, explain and communicate; demonstrating empathy, kindness and warmth.
- Competence: the knowledge, skills, attitudes and ability to practise safely and effectively.
- Competent: having the necessary knowledge, skills, attitude and ability to practise safely and effectively.
- Complexity in maternity care: presence of one or more clinical, psychological, social, or medical complications or further needs that require input and collaborative care by the multidisciplinary and multi-agency team.
- Consent: explaining what you intend to do with/ to someone and listening carefully to what they say about it. For consent to be valid, it must be given voluntarily by an appropriately informed person who has the capacity to consent to the intervention in question. Agreement where the person does not know what the intervention entails is not ‘consent’.
- Continuity of carer: a continuous relationship with a care provider or small group of care providers. Specifically, in maternity: care provided by practitioners for a woman and their newborn infant, partner and family throughout the continuum of their maternity journey.
- Delegation: the act of giving responsibility to another person.
- Family: the people identified by individuals who are significant and important to them.
- Holistic: treating individuals as a whole; in healthcare addressing the physical, emotional, psychological, social and spiritual needs as interdependent.
- Maternity journey: the individual’s experience of care and support pertaining to childbearing over time. May be current or historical relating to aspects of the childbearing process from pre-pregnancy, pregnancy, labour, birth, the immediate postpartum, and the early days and weeks of life.
- Mentoring: a work-based method of training using existing experienced staff to transfer their skills informally or semi-formally to learners.
- Multi-disciplinary team (MDT): practitioners providing care and support to individuals at all levels.
- Partner: the person considered by an individual to be their partner or other supportive individual.
- Practitioner: an appropriately qualified person in the practice of an occupation, for example a maternity support worker or a midwife. They may be registered or unregistered.
- Registrant: an appropriately qualified person who complies with and maintains their mandatory requirements and as such is eligible to be recorded as ‘registered’ on the official register.
- Safeguarding: measures to protect the health, wellbeing and rights of individuals. Safeguarding vulnerable childbearing women, newborn infants, partners and families who are at increased risk of harm. Vulnerability may be due to a range of clinical and psycho-social factors. Examples include disability, age, previous mental or physical illness, bereavement, poverty, legal status, ethnicity, not speaking the local language, or being in a situation of intimate partner violence. Potential harm may be emotional, physical, sexual, psychological, material or financial, or may be due to neglect.
- Scope of role: the extent and limits of the care that a practitioner may perform.
- Supervision: the act of overseeing something or someone. Supervision in healthcare means that the supervisor makes certain of safe and effective care.
- Wellbeing: a person’s wellbeing may include their sense of hope, confidence, self-esteem, ability to communicate their wants and needs, ability to make contact with other people, ability to show warmth and affection, experience and showing of pleasure or enjoyment.
- Woman-centred or personalised care: care centred around an individual’s needs, involving them in the decisions about their healthcare, care and support. Co-ordinating care as a collaborative process between the individual and those caring for them.
References
- Campbell, L. and McKendrick, J. (2017) Beyond Aspirations: Deploying the capability approach to tackle the under-representation in higher education of young people from deprived communities. Studies in Continuing Education. 39 (2) pp. 120-137
- Department of Health and Social Care – The Cavendish Review: An Independent Review into Healthcare Assistants and Support Workers in the NHS and Social Care Settings
- Department for Education – Introduction to T-Levels
- Department for Education – Find a regulated qualification
- Royal College of Midwives (2017) – The deployment, education and development of maternity support workers in England. A scoping report to Health Education England
- Health Education England – The Talent for Care: A National strategic framework to develop the healthcare support workforce
- Institute for Apprenticeships – apprenticeship standards
- Institute for Apprenticeships – T-Level organisational maps
- Lewis, R. and Kelly, S. (2015) Education for healthcare clinical support workers. Nursing Standard. 30 (15), pp. 38-41
- O’Shea, S. (2015) Arriving, surviving and succeeding: First in family women and their experiences of transitioning in the first year of university. Journal of College Student Development. 56 (5), pp. 499-517
- Royal College of Midwives – RCM Apprenticeship Guide
- Royal College of Midwives (2018) – Valuing MSWs
- Skills for Health – Roles Directory
- Skills for Health – Key Elements of the Career Framework
Acknowledgements
- Professor Teresa Shalofsky, Associate Professor of Midwifery and Lead Midwife for Education at the University of Birmingham
- Julia Austin, Midwife, Northampton General Hospital NHS Trust
Publication reference: PRN01141_i

