Introduction
This toolkit has been developed in conjunction with the review and refresh of the Maternity support worker competency, education and career development framework. It has been developed with the support of an expert stakeholder group and by a team who have experience of transforming the support worker element of a maternity unit’s workforce.
This toolkit provides a guide for teams who are implementing the updated national framework and includes examples of plans for people who have support worker roles in maternity services. It provides direction for individuals in roles who will be tasked to lead, project manage and operationalise the development of support workers. This includes examples for those who will be responsible for undertaking assessments and mapping of staff, and those who will be required to report progress on the safety and quality agenda to their trust board.
This toolkit will support you to undertake your own strategic planning and support the long-term goals for your service. Full implementation of the Maternity support worker competency, education and career development framework provides assurance that maternity care assistants (MCAs), maternity support workers (MSWs) and assistant practitioners (APs) (maternity) are appropriately educated and competent and support your service to deliver high quality and safe care.
Overview of processes
Example pathway for heads of midwifery (HoMs)/directors of midwifery (DoMs): project planning
Steps 1 to 5 below are the recommended considerations and actions that should be taken by HoMs and DoMs.
Step 1
- identify obectives and targets to implement the maternity programme transformation
- consider and identify membership of the implementation group
- identify a project lead
- start to develop your communication plan
- engage HR services and the finance team to be part of the implementation group
- engage with your Local Maternity and Neonatal System to report progress and to explore any funding opportunities
- engage with trust leads to integrate service planning
Step 2
- scope current service delivery (what tasks the support workers currently perform)
- review your workforce tool for safe staffing and calculate the skill mix for your service
- assess what level these tasks are at when compared to national job description
- consider your staffing strategy/projections/birthrates/complexities for the next 5 years
Step 3
- oversee the preparation of new job descriptions for levels in trust templates and expediate sign off by directorate managers and finance teams
- consider any regional work which may have been completed
Step 4
- review gap analysis with project team after mapping process of education and competency levels
- support the team with management of any HR issues
- oversee business case
- meet with local providers of education to show what could be offered for midwifery apprenticeships
Step 5
- support arrangements for upskilling and upgrading plans, and add to business case
- present business case
- prepare process with HR for any upgrading
- ensure adequate communication and preparation to support the transformation process
- ensure correct coding of your data returns for the MSWs who have met the requirements of the transformation on ESR
- use your transformation to inform your safety quality assurance goals
Practical implementation: heads of midwifery/directors of midwifery
Follow the steps within the pathway below.
Work with your project leads to plan what your workforce will look like in the short term and then over a period of 3 to 5 years. Consider the following questions:
- have you factored in the backfill required to support your apprenticeships (0.2WTE per week)?
- how many of your support workers in maternity could you support without compromising safety?
Once you have your high-level workforce plan and overall maternity workforce strategy, the project leads can begin to implement the MSW element using the Maternity Support Worker competency, education and career development framework, and thereby supporting the Three year delivery plan for maternity and neonatal services.
Case study 1: All Saints Maternity Unit
All Saints Maternity Unit is based within a district general hospital and has a birth rate of around 4000 births per year. The DoM and HoM are under pressure to meet safe staffing levels, impacted by a 5.4% midwifery sickness rate and some challenges recruiting and retaining midwives. The DoM is now considering how support workers in the maternity setting can be used to ease these staffing shortfalls within budget constraints. Therefore, the unit is going to implement the Maternity Support Worker competency, education and career development framework, which will support the Three year delivery plan for maternity and neonatal services and the NHS Long Term Workforce Plan. Local implementation will provide a development pathway and more job satisfaction for support workers in maternity services. In turn, this will support the midwifery workforce to deliver safer maternity care.
The maternity unit has a steady stream of applicants for MSW roles, although the attrition rate seems high and several level 2 MCAs on the delivery suite are dissatisfied with their job. They believe that most of their time is taken up with cleaning and they want to have the skills they need to support clinical care. The inpatient matron reports that they only have level 2 MCAs on the delivery suite and some on the ward to make beds, but often level 3 competencies are required. Due to this, MSWs need to move across the unit to support variations in activities and staffing.
The DoM and HoM gather the senior team to look at strategies to retain staff and review the service needs. A review of safe staffing levels using a workforce tool has been commissioned and they are awaiting the results to inform budget planning. The senior team holds a listening event with the workforce to discuss how best to meet service needs. They also consult with neighbouring trusts.
To align to the framework, All Saints Maternity Unit decides that level 3 MSWs would be preferable across the majority of the service to support gaps in provision and support new level 2 MCAs prior to their level 3 development. Some level 2 MCA positions will remain for current staff not wishing to become level 3 MSWs. This model will meet their current local requirements but may change as midwifery staffing levels improve.
The local multi-site tertiary unit has a different approach and decides to keep more MCAs to operate at level 2, because the level 3 workforce has the flexibility to support across all sites.
In addition, All Saints Maternity Unit is seeing an increasing number of women diagnosed with gestational diabetes. They have a full-time diabetes specialist midwife but want to release some of their time to deliver a midwife led clinic to relieve consultant time pressures and improve continuity and deliver more personalised care. They consider a level 4 Assistant Practitioner (maternity) who would be able to provide tailored information to women, prioritising safety and becoming active in teaching. The team is also considering level 4 AP (maternity) posts in bereavement, infant feeding, and their home birth service.
All Saints Maternity Unit decides to advertise for level 2 MCAs with the view to developing fully competent MSWs at level 3 in 18 months’ time via an apprenticeship route. Apprenticeships attract new talent and support retention of staff. The team recognises that some may aspire to become midwives in the future through an apprenticeship route. The HoM and DoM have read the Registered midwife degree apprenticeship evaluation report showing that recruiting from the local workforce which has direct experience of the realities of the workplace leads to increased resilience. This is thought to contribute to the successful retention of midwives qualifying via this route.
Example pathway for project leads
Steps 1 to 5 below are the recommended considerations and actions that should be taken by the project lead.
Step 1
- review the Maternity support worker competency, education and career development framework
- establish your working group in liaison with HoMs and DoMs
Step 2
- review current job descriptions (levels 2/3/4) and align with national JDs
- liaise with relevant Agenda for Change team
- engage with support workers in the maternity services and midwives.
- work with midwives to support them to understand their role, for example, accountability and supervision.
- arrange an event/introduction to transformation and involve:
- human resources
- union representatives
- your allocated finance lead
- trust-wide Practice Development Team
Step 3
- meet with local providers of education to show what could be offered locally
- review all trust resources/apprenticeships and support for healthcare workers
- review care certificate provision and access to maths and English functional skills level 2
Step 4
- produce a gap analysis of skills and provision
- use intelligence from mapping review to phase any upgrades to inform the business case
- check dates for submission
- submit business case
Step 5
- support delivery of upskilling
- process upgrading where needed and ensure adequate communication for those who have yet to meet the framework
Example pathway for practice development teams
Steps 1 to 5 below are the recommended considerations and actions that should be taken by the practice development team.
Step 1
- review the Maternity support worker competency, education and career development framework
- contact finance for all names of support workers in maternity services – WTE and current levels
- join FutureNHS/community of practice for MSWs
Step 2
- prepare your templates for review
- support project lead with launch
- meet with midwifery team leads to discuss the project so that they can support staff release for review
- work with midwives to support them to understand their role, for example, accountability and supervision
- prepare a database for recording each review
- allow an hour per person for the review
Step 3
- email each support worker in your maternity services, requesting their qualifications so that this can be discussed at their review meeting
- arrange career development discussions on an individual basis
Step 4
- meet with all support workers in your maternity services at all levels and undertake the career development review
Step 5
- supply gap analysis following mapping of skills.
- produce a development plan for any upskilling and feed into training needs analysis (may include study days for themes identified and/or individual development plans)
- follow up with signing off skills in the workplace using the agreed competency passports where required
Practical implementation: project leads and practice development teams
Follow the steps within the pathways below.
Early considerations
Get to know the Maternity support worker competency, education and career development framework. Read and re-read this as it will be your blueprint for assessing your MCA/MSW/AP (maternity) workforce.
There are 4 domains of practice:
- supporting women and families
- public health: prevention and health promotion
- personal and clinical skills
- creating safe environments
Within the domains are the 14 competencies required of support workers to deliver competent capable care across levels 2 (MCA), 3 (MSW) and 4 (AP (maternity)).
The framework sets out competency levels and the expectation of the depth of knowledge and skills needed to demonstrate the level of competency across levels 2, 3 and 4. Before you can set your assessment questions for the career development reviews, you will need to become familiar with these.
You need to assess what level your workforce is at across all 4 domains and 14 competencies; therefore, you will need to devise a consistent way of assessing the level that your workforce is currently at.
Depending on their current role, support workers in your maternity service may be undertaking duties of a level 2, 3 or 4 role. Project leads and Practice Development Teams should carry out a mapping process to show what tasks are being undertaken and at which level they are performed at within the service. A career development review process with each member of staff will determine at which level the individual support worker is currently working at. Devising assessment tools provides a structured and consistent way to conduct staff mapping. The examples included within this toolkit can be used or modified to support you with this.
Consider your communication strategies early in the transformation process. Ensure that union representatives and human resource staff are involved and invited to introductory meetings. Clarification is needed as early as possible within your project plan. Be mindful that this process may be new to many staff within your organisation, and could be a worrying time for some, therefore being transparent and supportive is crucial.
Investing time into your planning will pay dividends and is likely to result in a successful transformation process. The programme is about professionalising the role and recognising the significant contribution of support workers across maternity services, as well as enhancing the experiences of woman and families.
Setting assessment questions
Start to set your assessment questions in preparation for the career and development review meetings with each support worker within your maternity workforce. How you approach this will form your mapping tool. You may want to consider preparing a proforma, similar to an interview format. This would then provide you with a foundation and supply evidence for any further discussions needed later in the process.
Here is an example question developed from one element of domain 2 of the competency framework:
Domain 2: public health: prevention and health promotion
How you support women and families to make healthy choices
Competency 5: Promote a culture of health and wellbeing through providing information, advice and support to enable healthy lifestyle choices for all individuals, whilst understanding the causes of ill-health related to women of childbearing age, and their families.
Indicator 4: Supporting behaviour change
Level 2: Seeks support from a suitably qualified practitioner when women or members of their family signal a desire to make behaviour changes that can impact on health and wellbeing
Level 3: Understands the principles of behaviour change and interventions to prevent ill-health and effectively applies these to practice and personalises the individual’s right to privacy and choice.
Level 4: Applies principles of behaviour change within personalised contexts to enable personalised discussion, sensitively communicating complex, and/or potentially challenging information to women, if appropriate, to facilitate change.
The question developed to assess this part of domain 2 would vary according to the workplace of the support worker you are having the career development discussion with. For example, if they worked in a clinic environment, they may be supporting women with their decision-making about changing their diet or needing help on making choices around vaccinations. In a ward environment there may be opportunities to support smoking cessation or prevention of sudden infant death syndrome. In a community setting there could be support needed for infant feeding. Whatever maternity setting the support worker is in, they will be involved in some way, and at each level (2, 3, 4), in supporting the midwife to deliver the public health requirements.
Example question:
You are working on the ward and a woman asks you if you would look after her baby while she goes outside. You notice she has some cigarettes in her pocket. It’s a tricky situation, how would you manage that?
Top tip: This part of the process is investigatory, it is not an interview – it is about the level of contribution to this domain as an individual and being able to analyse your support worker in your maternity workforce overall. Later the documentation can be reviewed for any further individual development that may be required.
How to apply your mapping tool in career development discussions
As a development team it is likely to take several team meetings and some deliberations to devise your question proforma (around 8 to 10 questions should be sufficient). You should be confident that it covers all the domains and indicators within the competency framework. Once you have reached this point, you will be ready to commence the career development discussions with the support workers.
Top tip: Ensure your overall career review includes all the competencies across the domains in some form. Many questions you develop will include core competency threads (for example, communication skills, women centred care). They will run across multiple competencies so you should be able to cover all with the everyday skills that your support workers in maternity settings undertake.
Top tip: It may be that there are recurring themes during your interviews indicating that this would be one of the competency gaps across your workforce which requires upskilling. You will gain this information as you progress through the reviews and the analysis of the mapping.
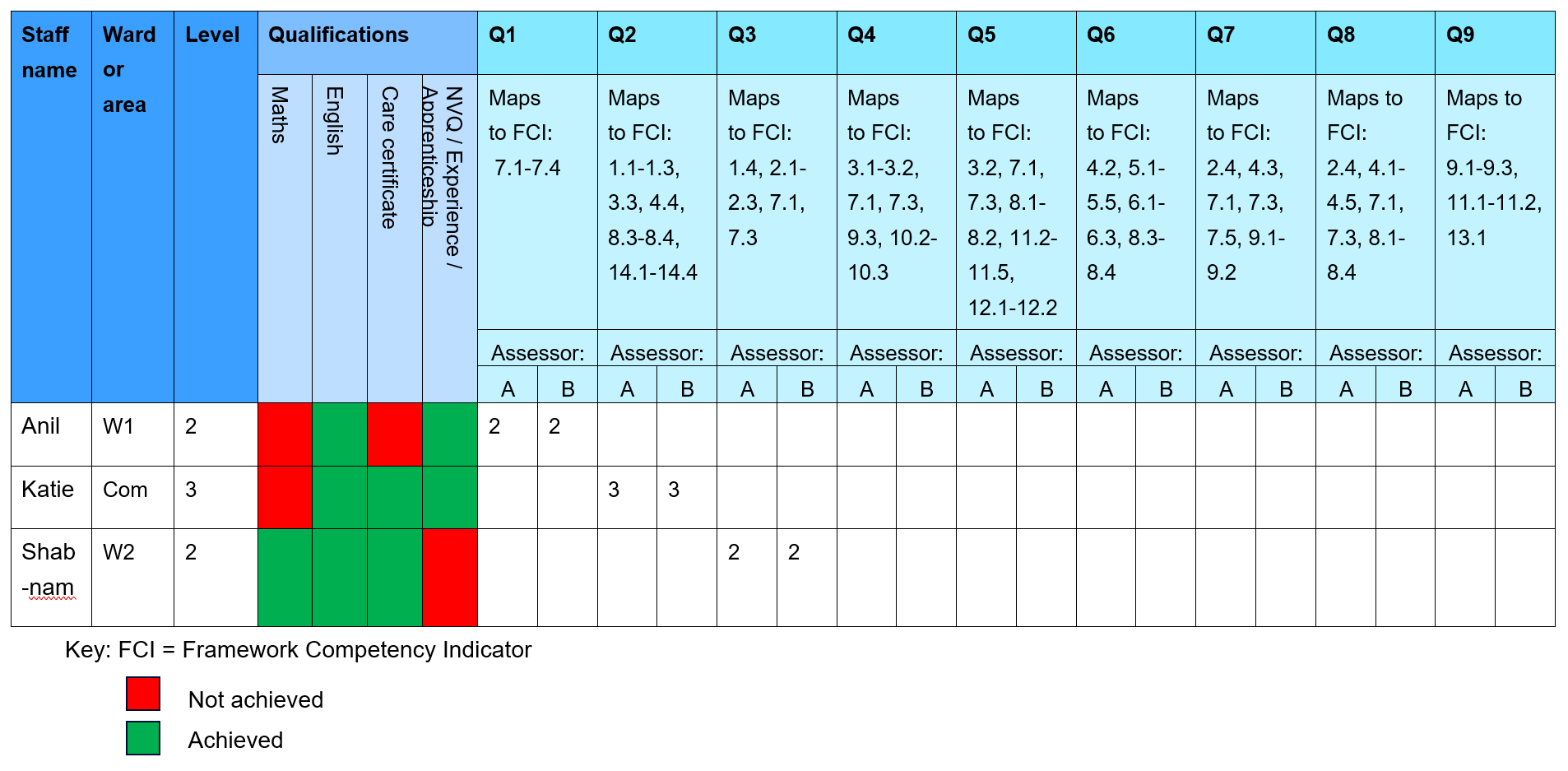
Case study 2 – Anil
The Practice Development Team (PDT) consists of two midwives who do not have any line management responsibility for the support worker they are assessing. For consistency, they will be assessing all the support workers across the maternity unit and community setting. This approach helps them to ensure that a fair, transparent and equitable process has been maintained, and will help if any appeals are raised against the process later. Keeping a record of the reviews in a consistent manner will also help as the project progresses.
The PDT is ready to meet with Anil who is a support worker with four years’ experience in the maternity unit, currently employed as a level 2. The PDT needs to assess the competency levels Anil is working at to develop a gap analysis of any skills and competencies needed to ensure Anil will be able to meet level 3 requirements. This will help to provide assurance of quality and competency to inform any upgrade, paving the way for potential career progression.
Anil works on the ward and the PDT has arranged a meeting to discuss career development and the competency framework. The review could either be face-to-face or virtual dependant on circumstances. The PDT is offering flexibility on how the meetings are facilitated to fit around shift patterns and other commitments people may have.
The PDT asks about any formal qualifications gained and refers to the data they collected prior to review. Anil has a NVQ level 2 in childcare but did not complete the care certificate course. Anil has a GCSE level 4 English, however, does not have this for maths. The PDT logs these details on the database for discussion later.
The PDT asks Anil to talk about a normal shift and what tasks are undertaken. Anil replies there are maternal observations and neonatal observations undertaken and help is given to the women to mobilise after caesarean section. After the initial conversation, it looks like Anil may be undertaking tasks aligned to a level 3 role as described within the framework. The PDT now needs to assess if Anil meets all the competency requirements to undertake a level 3 role, by asking questions around the domains.
The PDT asks the following question to explore Anil’s competency levels for Domain 2 of the framework:
“Anil you are working on the ward and a woman asks you if you would look after her baby while she goes outside. You notice she has some cigarettes in her pocket. It’s a tricky situation, how would you manage that?”
Anil responds by saying:
“Well, I’d advise that we couldn’t safely look after the baby and ask her to wait until her partner came so that she could leave the baby safely because the ward is very busy.”
The PDT continues with a prompt question:
“Would you do anything else Anil?”
Anil responds with:
“I would advise her if she did go outside for a cigarette, she needed to wash her hands and not handle the baby for 30 mins”.
At present, this is a level 2 answer, because at this point Anil does not initiate or plan any interventions. Anil is waiting for the woman to initiate a desire to change behaviour. It may be that Anil lacks confidence in the approach or lacks the knowledge to deliver it. The PDT could add a further question by asking how Anil would feel about offering a brief intervention.
For Anil to provide a level 3 answer she would need to provide more information, for example:
“This isn’t the right time for very brief advice, but when the woman returns to the bedside, I would initiate a very brief advice discussion about smoke free homes and second-hand smoke using the ask, advise, and act techniques.”
The PDT uses the proforma they developed during step 2 of the process to record comments on Anil’s responses to this question.
Anil’s proforma: domain 2
Qualifications: Maths/ English/ NVQ/apprenticeship/care certificate/other (circle as appropriate)
|
Question: You are working on the ward and a woman asks you if you would look after the baby while she goes outside. You notice there are some cigarettes in the pocket. It’s a tricky situation, how would you manage that? |
|
|
Domain and competency reference: Public health initiatives Indicators considered by this question: 5.2 to 5.5, 6.1 Screening, Making every contact count, healthy lifestyle choices, signposting. Social and cultural considerations. |
|
|
Responses: |
|
|
Level 2 answer example: |
Yes/No |
|
Signposting if woman initiates desire to stop |
No |
|
Identifies the opportunity for engagement |
No |
|
Gives some advice on safe handling of baby |
Yes |
|
Level 3 answer example: |
Yes/No |
|
Able to verbalise knowledge of CO Screening |
No |
|
Offers personalised service to engage for opportunities |
No |
|
Makes every contact count by actively encouraging conversation about their health and wellbeing |
No |
|
Actively engages health promotion opportunity (screening) showing insight into behaviour change |
No |
|
Comments: Anil gives some advice on how to handle baby afterwards but doesn’t actively engage in an opportunity to make a very brief intervention. When asked how she would feel about a very brief intervention, Anil says she would feel uncomfortable and wouldn’t feel confident to introduce the subject. Anil’s overall knowledge base for public health interventions requires upskilling. Will require development plan for this domain. |
|
|
Competency score: 2 |
|
The PDT continues to ask the remaining questions to conclude the assessment within the career development discussion meeting and identify any further areas requiring development in addition to public health.
So far, the PDT has only asked Anil one question. Based on Anil’s response to that question, she will need to complete the care certificate and maths functional skills level 2. Support will be needed to develop the public health part of the role before stepping up to level 3.
After the meeting with Anil, the PDT opens the database to record the scores under the domain and competency reference (see page 22 for an example of a database).
Case study 3 – Katie
Katie works in the community and is currently working as a level 3 MSW with 8 years’ experience. The PDT has arranged the career development review at 7pm, as Katie can put her children to bed and feels more relaxed in a virtual meeting from home.
As with Anil, the team reviews Katie’s current qualifications. Katie has the care certificate but doesn’t have an apprenticeship or NVQ, however she has achieved an A level in English. Katie does not have a maths qualification.
The team asks about current everyday activities undertaken. Katie explains that she runs glucose tolerance test clinics in the community, as well as carrying out blood spot tests and providing infant feeding support visits.
Katie is working at a level 3 in line with tasks indicated in the national level 3 job description. The PDT asks whether she has any interest in career progression. Katie responds by explaining that she would really like to get a level 4 job and consider a midwifery career later.
The PDT then conducts the assessment by asking Katie a series of questions mapped to the domains, starting with domain 1, competency 3, indicator 1: safeguarding.
Domain 1: supporting women and families
How you support women and their families, providing care throughout their maternity journey.
Competency 3: Notice and respond appropriately to the changing needs of the individual and their family.
Indicator 1: Safeguarding
Level 2: Understands and follows the principles of safeguarding and protection, to include adhering to local security procedures.
Level 3: Is vigilant for cues indicating safeguarding issues related to women and families. Escalates safeguarding concerns and reports to the MDT in a robust, timely manner; complying with legal requirements.
Level 4: Independently undertakes agreed risk identification and assessment activity, within scope of role and practice, in accordance with local and national safeguarding pathways.
The PDT asks the following question to explore Katie’s competency levels for this domain of the framework:
“Katie, you are asked to help a woman in the community with some breastfeeding concerns. Yana is a new mum who can speak English, but it is her second language. She arrived in the UK when she was 6 months pregnant. Yana lives with her partner who is present at the review. As you are supporting Yana you notice there is some bruising to the arm in a couple of places. The partner is answering all the questions for Yana, although you know Yana can speak English. What would you do?”
Katie responds with:
“I would feel concerned about this. Yana is vulnerable. This is a case of a new mum in a foreign country who is quite isolated. The partner sounds a little overbearing.”
The PDT continues with a prompt question:
“It’s a difficult one isn’t it, what would you do?”
Katie responds with:
“Well, if the partner is there, I wouldn’t be able to ask anything because I could put Yana and the baby at risk. I would contact the midwife urgently to ask for advice. I would check the baby and report my findings to the midwife so that a plan of care can be devised for us to continue to care for Yana and the baby. I would work on developing my relationship and getting to know Yana better.”
This is a level 3 answer, because Katie recognises the vulnerability of Yana and notices the overbearing nature of the partner. Katie is mindful that a plan needs to be put together and that part of her role will be to contribute to that plan.
An example of a level 2 answer could be “I would be concerned because I don’t know the reason for the bruising and Yana may be at risk of harm, so I would report this to the midwife”.
The PDT continues to ask the remaining questions to conclude the assessment within the career development discussion meeting. They use the proforma they developed during step 2 of the process to record comments on Katie’s responses.
So far, the PDT has reviewed Katie’s qualifications and asked her one question. Based on this information, Katie will need to complete maths functional skills level 2. If Katie continues to provide level 3 answers to the remaining question, she can consider a level 4 apprenticeship as achievement of level 3 competency will be met.
After the meeting with Katie, the PDT opens the database to record the scores under the domain and competency reference (see Appendix 1 for an example of a database).
Case study 4 – Shabnam
Shabnam has been in post for 12 months and is a level 2 support worker working on the postnatal ward. The PDT has established, from their first review of evidence, that Shabnam has successfully completed the care certificate and has both maths and English functional skills at level 2. Shabnam doesn’t have an NVQ or equivalent experience at level 3. The PDT asks whether she has any interest in career progression. Shabnam responds by explaining that she would like to progress into a level 3 role and would be happy to stay at that level.
The PDT then conducts the assessment by asking Shabnam a series of questions mapped to the domains, starting with domain 3, competency 7, indicator 3: providing care.
Domain 3: personal and clinical skills
How you develop and use your skills to care for women and their families.
Competency 7: Provide and monitor care safely and effectively.
Indicator 3: Providing care.
Level 2: Accurately undertakes delegated tasks, for which they have received training, ensuring basic care needs for women and babies are met. Reports completion of the task and any findings to an appropriately qualified practitioner.
Level 3: Utilises a range of clinical information and associated knowledge of normal baseline observations in women and babies to confirm wellbeing, reporting findings to a registered practitioner and escalating where wellbeing is not confirmed.
Level 4: Working as a member of the MDT, uses a range of clinical information to inform a judgment on the effectiveness of an existing care plan and the requirement to immediately escalate concerns to a registered practitioner or to make a referral back to the MDT for review.
The PDT starts by asking Shabnam to talk through a typical shift. Shabnam replies by explaining that she usually prepares the beds for new admissions and supports mothers with infant feeding. She also helps women to the shower and toilet when needed and carries out observations when the midwife asks.
The PDT asks the following question to explore Shabnam’s competency levels for this domain of the framework:
“Shabnam, you answer a call bell, and the woman asks you to help her to the toilet. You are helping her get out of bed and she says she feels faint. What would you do?”
Shabnam responds with:
“I would get her safely back into the bed and arrange a bedpan. Then I would let the midwife know she was feeling faint.”
The PDT continues with a prompt question:
“Would you do anything else?”
Shabnam responds with:
“Once the lady was in bed, I would then report my findings to the midwife.”
This is a level 2 answer.
An example of a level 3 answer could be: “I would get her safely into bed and check the blood loss. I would take a full set of observations using a MEOWS review and report any abnormality to the midwife. I would record this in the woman’s records.”
It may be that Shabnam is currently undertaking tasks at level 3, but she needs support to develop the knowledge and skills to build a picture on the clinical information.
The PDT continues to ask the remaining questions to conclude the assessment within the career development discussion meeting. They use the proforma they developed during step 2 of the process to record comments on Shabnam’s responses.
So far, the PDT has reviewed Shabnam’s qualifications and asked her one question. Based on this information, Shabnam has already achieved some of the education qualifications but needs support to meet level 3. If Shabnam continues to provide level 2 answers to some or all of the remaining questions, she will require experience and support to meet the level 3 competencies. To achieve this Shabnam can complete the skills passport and will require a MSW associate educationalist or practice development midwife to observe her in practice and sign off the competencies as they are achieved. She could also be supported to do an apprenticeship.
After the meeting with Shabnam, the PDT opens the database to record the scores under the domain and competency reference.
Top tip: The support workers in your maternity unit will be at various levels according to their area of work, degree of experience and levels of competence. This is where the mapping exercise will help you to determine the initial assessment of what level the support worker is practising at right now. The important thing to remember at this point is that all support workers in your maternity services will have areas of strength and areas that require development.
Recording career development reviews
In each of the case study examples for Anil, Katie and Shabnam, a proforma was used to ensure that responses to questions determine and support scoring decisions. After the career development discussions, the PDT recorded information in a central database.
An example database is provided in Appendix 1. You can use this example to create an excel version or you can design your own. Essentially, the key components of an effective database are to provide:
- the provision of one central record of your support worker workforce in your maternity services
- the ability to record information about work base and levels of your staff
- a record of qualifications to include maths, English and care certificate as a minimum
- mapping of the framework domains, competencies and indicators to your questions
- evidence of the score/level achieved by the member of staff against each question
Having this information will support ongoing career development conversations with your team. It will act as a standardised way to provide feedback to each support worker in your maternity services, and it will provide direction in terms of supporting individual and group upskilling.
Top tips: Checklist for career development reviews:
- Practice development teams and project leads should make sure they have prepared the review questions mapped against the competencies.
- Use the same reviewers or a very small team of reviewers for consistency.
- Have two reviewers at the assessment with each reviewer scoring the responses independently. Scores can be discussed and agreed between the reviewers after the assessment.
- Maintain privacy during the review.
- Provide flexibility of appointments (time, online, face-to-face) as per the preference of the support worker.
- Adopt supportive techniques and offer encouragement to those support workers who may be concerned. Fostering an environment that alleviates anxiety can facilitate an individual to perform better and accurately demonstrate how they are meeting the levels of the framework.
- Use open questioning techniques to get the full extent of the support worker’s knowledge base.
- Have your database ready to record your reviews to support the next steps.
Project leads: next steps
When you have your completed database that records all skill levels mapped to the framework, and educational requirements for each of your support workers, it is time to consider what the educational needs are for your established and future support worker workforce. You should:
- complete your gap analysis report
- if there are any shortfalls in competencies evidenced:
- identify what these shortfalls are
- highlight any common themes emerging
- plan and provide some ‘upskilling days’ to address the common themes to meet the needs of multiple support workers in your organisation
- plan and provide some individual support to supplement the upskilling of less common areas
Once you have your gap analysis you have the information you need to prepare the business case. For example, consider the following:
- How many of the support workers in your maternity services will require a care certificate?
- Identifying what you need to cost in your business plan to support the service development needs for the first part of your transformation plan to succeed. This can be facilitated by identifying the gaps in your workforce across educational requirements and meeting the framework.
- Consider your longer-term goals, for example, apprenticeships across the levels and associated funded needed for these.
In summary, having considered from the start what you need from your workforce you can ensure that your organisational transformation plans are aligned to this goal. Achieving transformation takes time, and to succeed you need effective planning, sound communication and partnership working with a number of key colleagues within the organisation, including your support workers.
Frequently asked questions
Q: When we completed the review, we found some discrepancies in scoring. What should we do?
This can be discussed by reviewing the notes taken at the time and further discussion with the individual if needed. Remember this is not an exact science.
Q: I am working with a support worker who is close to retirement and doesn’t want to develop any further. Do I need to do the review?
Yes. Remember you are assessing the quality of the service, so you need an overview of all of your support workers across the maternity services workforce to help you understand the roles needed for your service.
Q: The support worker referred to in the question above is very experienced and has met all the competency assessments for level 3 but would find the maths and English qualification at this stage in life incredibly stressful – although they are happy to complete the care certificate. Can there still be an uplift to the next level?
Theoretically if the support worker is completing tasks at level 3 and meets the competencies at level 3, but meets education requirements for level 2, then once the new job descriptions are completed the support worker would be expected to undertake level 2 tasks only. Take advice from your senior team and HR colleagues. It may be that these cases could be looked at individually. Take into consideration what your organisation needs, ask what the risks are to the organisation and the individual to help to decide your course of action. Use a common-sense approach. There are likely to be a very small number of these cases in your total support worker workforce.
Q: I am thinking of taking on some new MSWs, how should I plan to support their future and the organisation’s aspirations for workforce development?
You can recruit straight into a level 3 post (on the new JD) if that’s what your organisation needs. Then you could support level 4 apprenticeships if you are looking for potential level 4 APs (maternity) through this route. You could then also support registered midwife degree apprenticeships (RMDA) for those support workers who wish to train to become registered midwives. If you decide to recruit into level 2 posts, this would be into MCA roles. However you could identify the post as Trainee MSW and support these individuals to achieve level 3 after completion of an apprenticeship.
Q: I have a MSW who has been in post for 18 months. She hasn’t got all her competencies yet. Should I get her onto an apprenticeship?
Usually an apprenticeship at level 2 would be for new starters who have lots to learn. If your MSW has been in post for a while you could use a competency skills passport to meet the framework for upgrading to a level 3 role. It may be after this that the MSW wants to develop further and look at a level 3 apprenticeship for ongoing development.
Q: Can a Nursing Associate (NAs) be used instead of a level 3 Maternity Support Worker or a level 4 Assistant Practitioner (maternity) within maternity services?
Providers are looking to adopt innovative workforce solutions to support ongoing service delivery in maternity services. The Nursing and Midwifery Council has provided delegation and accountability guidance with reference to NA’s in nursing environments, however there are several areas of concern in relation to the deployment of nursing associates in maternity settings. Having a maternity support worker workforce which is educated to an agreed national standard and tailored to maternity settings promotes safety, care that is centred around women and their babies and reduces the levels of fragmented care.
Glossary
- AP (maternity): Assistant Practitioner (maternity)
- DoM: directors of midwifery
- ESR: Electronic Staff Record
- GCSE: General Certificate of Secondary Education
- HoM: heads of midwifery
- HR: Human Resources
- JD: Job description
- NHS LTWP: NHS Long Term Workforce Plan
- MCA: maternity care assistant
- MEOWS: Modified Early Obstetric Warning Score
- MSW: maternity support worker
- NVQ: National Vocational Qualification
- PDT: practice development team
- RMDA: Registered Midwife Degree Apprenticeship
- WTE: Whole time equivalent
References
NHS England (2023) Three year delivery plan for maternity and neonatal services
NHS England (2023) NHS Long Term Workforce Plan
Appendix 1: database example
Appendix 2: coding MSWs and support staff on ESR
In 2019 Health Education England published the Maternity support worker competency, education and career development framework. This has now been superseded by NHS England’s updated version, published in May 2024.
MSWs who have already met the framework requirements and apprentice MSWs who are currently working towards completion of the 2019 framework requirements will not have to move onto the new 2024 framework, unless directed to by their employer.
New employees and existing MSWs who have yet to commence their development pathway should meet the 2024 framework requirements.
On 17 June 2021 an update was issued to all NHS organisations with instructions on the coding for MSWs and support staff. This means that following your mapping exercise individuals at level 3 or 4, who meet the Maternity support worker competency, education and career development framework, can now be coded as maternity support workers using the N9C code.
Full details can be found in the NHS Occupation Code Manual.
|
Staff group |
Job role |
Notes |
ESR code |
|
Additional Clinical Services |
Maternity support worker |
Staff who meet the MSW competency, education and career development framework at education and competency level 3 or 4. This is normally achieved by undertaking the Senior Healthcare Support Worker Apprenticeship and additional maternity modules in line with the MSW curriculum or through APEL. |
N9C |
There is also an apprentice MSW option available in ESR – for individuals on the apprenticeship, use this code until they complete the apprenticeship and then transfer them to the N9C code.
Level 2 maternity care assistant (previously ‘Housekeeper’) roles
Those individuals who undertake the level 2 maternity care assistant role, as defined by the MSW competency, education and career development framework, should be coded as H2C for now, until planned H-Matrix changes are undertaken to bring support workers into the N-matrix and enable recoding of such staff.
Action required by organisations
Once your maternity support workers fully meet the framework at levels 3 or 4, you should amend your ESR coding for these individuals to ensure they are on a N9C code. Your level 2 support staff, carrying out the maternity care assistant role or equivalent, should be coded as H2C.
Publication reference: PRN01141_ii