What is PSIRF?
The Patient Safety Incident Response Framework (PSIRF) sets out the NHS’s approach to developing and maintaining effective systems and processes for responding to patient safety incidents for the purpose of learning and improving patient safety.
Patient safety incidents are unintended or unexpected events (including omissions) in healthcare that could have or did harm one or more patients.
The PSIRF replaces the Serious Incident Framework (SIF) (2015) and makes no distinction between ‘patient safety incidents’ and ‘Serious Incidents’. As such it removes the ‘Serious Incidents’ classification and the threshold for it. Instead, the PSIRF promotes a proportionate approach to responding to patient safety incidents by ensuring resources allocated to learning are balanced with those needed to deliver improvement.
The PSIRF is not a different way of describing what came before – it fundamentally shifts how the NHS responds to patient safety incidents for learning and improvement. Unlike the SIF, the PSIRF is not an investigation framework that prescribes what to investigate. Instead it:
- advocates a co-ordinated and data-driven approach to patient safety incident response that prioritises compassionate engagement with those affected by patient safety incidents
- embeds patient safety incident response within a wider system of improvement and prompts a significant cultural shift towards systematic patient safety management
Organisations are required to develop a thorough understanding of their patient safety incident profile, ongoing safety actions (in response to recommendations from investigations) and established improvement programmes. To do so, information is collected and synthesised from a wide variety of sources, including wide stakeholder engagement.
A patient safety incident response planning exercise is used to inform what the organisation’s proportionate response to patient safety incidents should be. The PSIRF approach is flexible and adapts as organisations learn and improve, so they explore patient safety incidents relevant to their context and the populations they serve.
The principles and practices within the PSIRF embody all aspects of the NHS Patient Safety Strategy and wider initiatives under the strategy, including the introduction of patient safety specialists, development of a national patient safety syllabus, development of the involving patients in patient safety framework and introduction of the Learn From Patient Safety Events service. The NHS Patient Safety Strategy sits alongside and supports the NHS Long Term Plan.
Who does PSIRF apply to?
The PSIRF can be used by any healthcare service but is mandatory for services provided under the NHS Standard Contract, including acute, ambulance, mental health, and community healthcare providers. This includes maternity and all specialised services.
Providers that are not NHS trusts
Organisations that provide NHS-funded care under the NHS Standard Contract but are not NHS trusts or foundation trusts (e.g. independent provider organisations) are required to adopt this framework for all aspects of NHS-funded care and may apply this approach to their other services (including social care) for consistency. Organisations should take a proportionate approach when applying PSIRF principles. For example, smaller providers (or similar) may not need to undertake the full analysis required for patient safety incident response planning (e.g. due to limitations on data availability).
Find out more about how to apply PSIRF principles proportionately.
Primary care
Primary care services contracted under the NHS Standard contract are required to comply with PSIRF. Other primary care providers may wish to adopt this framework. Primary care providers that wish to adopt PSIRF should work with their integrated care board (ICB) to do so.
Social care
The PSIRF is a patient safety framework, and as such applies to the delivery of healthcare services. Therefore, social care organisations are required to adopt PSIRF for care provided under the NHS Standard Contract. Social care organisations are not required to adopt PSIRF for social care, but may wish to do so.
Achieving effective learning and improvement using PSIRF
The PSIRF supports the development and maintenance of an effective patient safety incident response system that integrates four key principles:
1. Compassionate engagement and involvement of those affected by patient safety incidents
The PSIRF recognises that learning and improvement following a patient safety incident can only be achieved if systems and processes that support compassionate engagement and involvement of those affected by patient safety incidents (patients, families, and staff) are in place.
Compassionate engagement and involvement mean working with those affected by patient safety incidents to understand and answer any questions they have in relation to the incident and signpost them to support as required. When a patient safety incident investigation (PSII) or other learning response is undertaken, organisations should meaningfully involve those affected, where they wish to be involved. Organisations must have policies to support this to happen and should consider how they will meet the needs of those affected. Detailed guidance and standards are available in Engaging and involving patients, families and staff following a patient safety incident.
2. Application of a range of system-based approaches to learning from patient safety incidents
The PSIRF promotes a range of system-based approaches for learning from patient safety incidents, rather than methods that assume simplistic, linear identification of a single cause.
Organisations are encouraged to use the national system-based learning response tools and guides, or system-based equivalents, to explore the contributory factors to a patient safety incident or cluster of incidents, and to inform improvement.
Those leading patient safety incident responses (learning response leads) and those involved in the oversight of learning and improvement emerging from patient safety incident response require specific knowledge and experience. These requirements are detailed in the patient safety incident response standards.
3. Considered and proportionate responses to patient safety incidents
Organisations have finite resources for patient safety incident response. The PSIRF supports organisations to use their incident response resources to maximise improvement, rather than repeatedly responding to patient safety incidents based on subjective thresholds and definitions of harm, from which new learning will be limited.
Some patient safety incidents, such as never events and deaths thought more likely than not due to problems in care (that is, those meeting the Learning from Deaths criteria for investigation) all require a PSII to learn and improve. Some incident types will also require specific reporting and/or review processes to be followed. These requirements are detailed in the Guide to responding proportionately to patient safety incidents.
The PSIRF sets no further rules or thresholds (other than those set out in the Guide to responding proportionately to patient safety incidents) to determine what needs to be learned from to inform improvement. Incident response activity may include investigation of an individual incident where contributory factors are not well understood, or a thematic review of past learning responses to inform the development of a safety improvement plan. If an organisation and its ICB are satisfied risks are being appropriately managed and/or improvement work is ongoing to address known contributory factors in relation to an identified patient safety incident type, and efficacy of safety actions is being monitored, it is acceptable not to undertake an individual response to an incident – other than to engage with those affected and record that the incident occurred.
4. Supportive oversight focused on strengthening response system functioning and improvement
All healthcare organisations providing and overseeing NHS-funded care must work collaboratively, with a common understanding of the aims of this framework, to provide an effective governance structure around the NHS response to patient safety incidents. The PSIRF expects ICBs to facilitate collaboration at both place and local system level.
The PSIRF requires regulators and ICBs to consider the strength and effectiveness of NHS providers’ incident response processes. Accountability for the quality of learning responses to individual incidents sits with provider leaders. Providers are not required to seek sign off for incident response reports from their ICB; however, they must be open with information relating to patient safety incidents and findings from incident responses, including formal reports, to support continuous development of an effective incident response system. Further information is given in oversight roles and responsibilities specification.
What are organisations required to do?
Organisations are required to apply this framework in the development and maintenance of their patient safety incident response policy and plan.
An organisation’s patient safety incident response policy should describe its overall approach to responding to and learning from patient safety incidents for improvement and identify the systems and processes in place to integrate the four key principles of PSIRF. It should describe how those affected by a patient safety incident will be engaged, what governance processes for oversight are in place and how learning responses are translated into improvement and integrated into wider improvement work across the organisation. The policy should also outline how patient safety incident response integrates with other activities such as clinical governance, HR and complaints management, and underline that the remits of different response types are distinct and must be kept so. A national policy template is available.
An organisation’s patient safety incident response plan should specify the methods it intends to use to maximise learning and improvement and how these will be applied to different patient safety incidents. It should be based on a thorough understanding of the organisation’s patient safety incident profile, ongoing improvement priorities, available resources and the priorities of stakeholders including patients and local Healthwatch. A national plan template is available.
Both documents – the policy and plan – should align with and be integral to the organisation’s wider approach to safety improvement and must be published on the organisation’s website.
Plans should be updated regularly based on new learning, an organisation’s changing risk profile and ongoing improvements. In this way, incident response becomes part of a wider safety management system approach.
Involvement of patient safety partners
The NHS Patient Safety Strategy promotes the involvement of patients, families, and carers as partners both in their own care and in the wider oversight of healthcare. Such involvement in oversight is of specific value in the development of an organisation’s patient safety incident response policy and plan. Patient Safety Partners should also play an important role on incident response oversight committees, or similar groups. More information is provided in the framework for involving patients in patient safety.
PSIRF and inequalities
Some patients are less safe than others in a healthcare setting. The PSIRF provides a mechanism to directly address these unfair and avoidable differences in risk of harm from healthcare:
- the PSIRF’s more flexible approach makes it easier to address concerns specific to health inequalities: it provides the opportunity to learn from patient safety incidents that did not meet the definition of a ‘Serious Incident’
- PSIRF prompts consideration of inequalities in the development and maintenance of patient safety incident response policies and plans
- tools in the patient safety incident response toolkit prompt consideration of inequalities during the learning response process including when developing safety actions
- engaging and involving patients, families and staff following a patient safety incident gives guidance on engaging those with different needs
- the framework endorses a system-based approach (instead of a ‘person focused’ approach) and is explicit about the training and skill development required to support an approach. This will support the development of a just culture and reduce the ethnicity gap in rates of disciplinary action across the NHS workforce
How to use the PSIRF
This framework describes the four main principles of PSIRF in relation to responding to patient safety incidents.
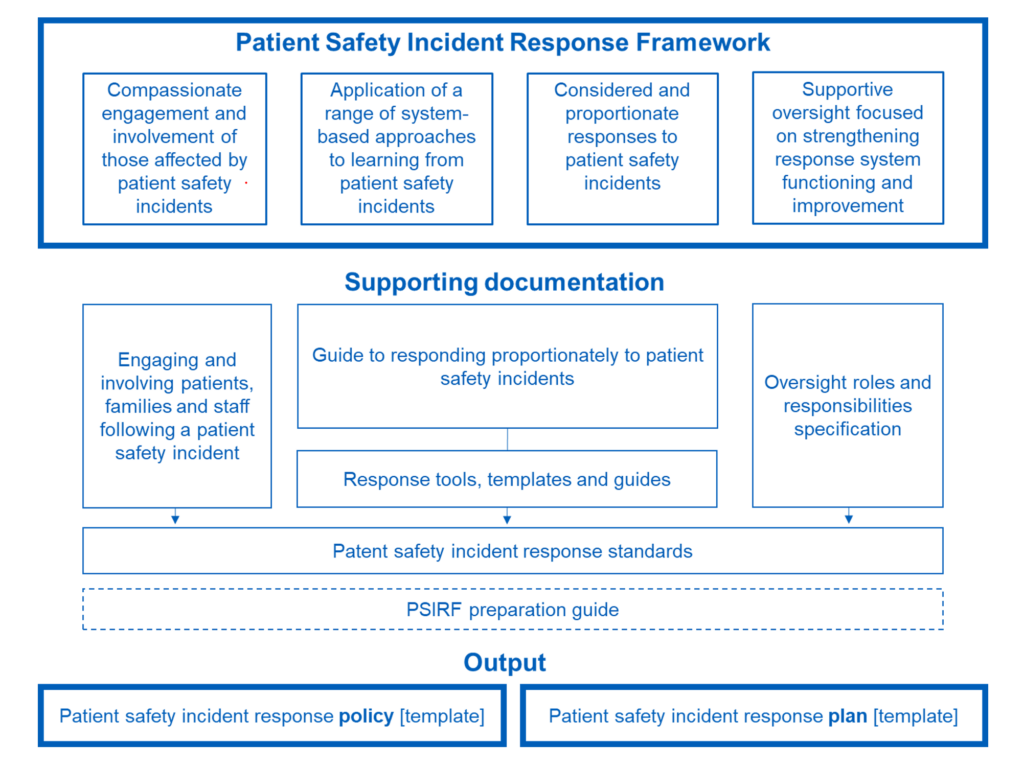
It is supplemented by the detail in the following documents:
- a comprehensive preparation guide that describes the steps organisations should take to prepare for and transition to the framework. This includes national templates for developing a local patient safety incident response policy and plan
- detailed guidance on engaging those affected by patient safety incidents and, with agreement, involving them in the learning response process
- a guide to responding proportionately to patient safety incidents including planning, response tools, guides, and report templates
- a detailed specification for the roles and responsibilities for those overseeing patient safety incident response
- patient safety incident response standards including training requirements
Organisations should use this guidance, together with relevant local information, to inform and maintain the corresponding sections of their local policy and plan as needed.
Figure 1: Overview of the Patient Safety Incident Response Framework documentation
Text description: figure 1 provides an overview of the framework and associated documents.
Links to other processes
This framework describes how the NHS manages patient safety incidents, including how it plans its response activities for the purpose of improving patient safety and how it engages with those affected. This framework and the response activities it supports explicitly exclude activities that apportion blame or determine culpability, determine preventability, or identify cause of death.
Some patient safety incidents may also require a separate response that is not focused on learning for patient safety improvement. For example, some incidents where a patient dies may be subject to investigation by a coroner to determine how, when and where they died. Others may involve the police where there is a reason to think criminal activity may have taken place. Some incidents will lead to concerns about an individual’s fitness to practise or ability to do their job, and so may be considered by the employer or a professional regulator.
Where a response is required that is not focused on learning for patient safety improvement, relevant referrals should be made to ensure it is conducted entirely separately. Care must be taken not to conflate and combine patient safety incident response activity with other remits.
What next?
The implementation and impact of PSIRF is being evaluated via a National Institute for Health Research (NIHR)-funded study that started in May 2022.
The National Patient Safety Team will use the evaluation findings together with national indicators of effectiveness to inform future iterations of PSIRF in formative and summative manner, to enable the NHS to continue to improve its approach to patient safety management. The team will continue to build on the foundations set by PSIRF in developing a safety management system that ensures a methodical and systematic approach to risk management as used in other high-risk industries.
Note of acknowledgement
Seventeen early adopter provider organisations tested the introductory version of the PSIRF alongside their commissioners (now ICSs) and NHS England regional leads. An independent evaluation of the early adopter programme found widespread support for the PSIRF; all recommendations from this were carefully considered by the National Patient Safety Team when revising PSIRF documents. The experience of early adopters and insights gained from the early adopter programme have also informed this revision.
We would like to thank our early adopters, patient safety partners and wider stakeholders who have generously given their time to share their experiences of the PSIRF. This revised framework would not have been possible without their help, constructive feedback, and ideas.
Publication reference: PRN01274