First published: 12 January 2016 (as Policy book for primary medical services)
First update: 9 November 2017
Previous update: May 2022
Current update: July 2024
Executive summary
This Primary medical services policy and guidance manual (PGM) has been updated to reflect ongoing development and changes in the commissioning and contractual management landscape. This suite of policies should be followed by all commissioners of NHS primary medical services. This approach ensures that all commissioners, providers and most importantly patients are treated equitably, and that NHS England and its commissioners meet their statutory and/or delegated duties.
NHS England is committed to reviewing this PGM regularly.
The Health and Care Act 2022
The Health and Care Act 2022 gained royal assent on 28 April 2022. It:
a. formally established NHS integrated care systems (ICSs) and gave their governing bodies – integrated care boards (ICBs) – a broader range of responsibilities. This was done at the same time as abolishing clinical commissioning groups (CCGs)
b. introduced powers for the new NHS provider selection regime (PSR), which have now established a new set of rules for arranging NHS services to give decision makers a more flexible and proportionate decision-making process for selecting providers to deliver healthcare services to the public, including primary medical services
The inception of ICBs from 1 July 2022 has brought a change to who commissions primary medical services. To support commissioners, NHS England has reviewed and updated the 2022 version of the PGM and made a number of additions and amendments.
Integrated care systems
With primary medical services successfully delegated to CCGs for some time, this means ICBs assumed delegated responsibility for primary medical services on establishment under a new delegation agreement incorporating, which now include all dental (primary, secondary and community), general optometry, and pharmaceutical services.
The aim of the delegation is to empower ICBs to join up health and care, improve population health and reduce health inequalities.
Under delegation ICBs have responsibility for commissioning and contract monitoring GP services in their locality/systems, with NHS England maintaining overall accountability.
Commissioner in this PGM means NHS England or ICBs under delegated authority.
NHS provider selection regime
As of Monday 1 January 2024, the NHS provider selection regime (PSR) is in force.
The PSR is set out in the Health Care Services (Provider Selection Regime) Regulations 2023, which the Department of Health and Social Care introduced into Parliament on 19 October 2023.
NHS England has published statutory guidance to support implementation of the PSR regulations, setting out what relevant authorities must do to comply with them. This includes some sector specific considerations, including primary care (annex C).
The PSR seeks to ensure that decisions about who provides healthcare services are:
- made in the best interest of patients, taxpayers, and the population
- robust and defensible, with conflicts of interests appropriately managed
- made transparently
- compliant with the rules of the regime as set out in NHS England guidance
As this PGM update was made prior to confirmation of the PSR coming into effect. The guidance will be updated in due course to ensure it better reflects the PSR. Queries about the PSR should be sent to psr.development@nhs.net .
General
This PGM is divided into 4 parts (A, B, C and D); namely:
- part A – excellent commissioning and partnership working
- part B – general contract management
- part C – when things go wrong
- part D – general
Each part has headed numbered chapters with headed numbered sub-sections, which can be found in the contents list on the left of this page.
Reference to external legislation or guidance may be required to ensure access to current wording mitigating the need to update the PGM where such changes, and hyperlinks may be provided.
Where templates are provided these may be by hyperlink if published elsewhere or embedded as extractable documents for easier onward use.
This guidance supersedes all previous versions of the PGM.
Part A – excellent commissioning and partnership working
1 Introduction
1.1 Introduction
1.1.1 NHS England became responsible for direct commissioning of primary medical services on 1 April 2013 and since then, the emergence of co-commissioning has seen all CCG taking on delegated authority until 30 June 2022. Thereafter, ICBs act as the commissioner under a delegation agreement.
This policy has been reviewed and refined considering:
- feedback from commissioner users
- engagement with stakeholders
- contractual and regulatory changes
- coming into force of the Health and Social Care Act 2022
1.1.2 This PGM provides the policies to support a consistent and compliant approach to primary medical services commissioning across England.
1.1.3 The PGM identifies sections which describe mandatory functions (ie those absolutely defined in legislation and law) versus those which are provided as guidance or best practice.
1.1.4 The PGM is supported by a suite of e-learning modules to provide commissioners a deeper appreciation of some of the more complicated commissioning or contract management scenarios they may face and complement the content within the PGM. A link to each can be found in the following sections and you will need to create a user account with NHS England’s e-Learning for Healthcare to access them.
- part B – chapter 8 contract variation: approving GP practice boundary changes
- part B – chapter 7 special allocation schemes (SAS)
- part B – chapter 8 contract variation: GP contractor changes: incorporation and novation
- part C – chapter 2 unplanned/unscheduled and unavoidable practice closedown: handling threats to the continuity of GP services
- part B – developing a primary medical services procurement strategy
Each module should take between 30 to 40 minutes to complete and there is a short self-assessment at the end of each module with results provided immediately.
1.2 Structure
1.2.1 A number of new policies have emerged since the policy book was first published and these have been incorporated into this manual. The PGM is structured into 4 main sections for ease of navigation. These are:
- part A – excellent commissioning and partnership working
- part B – general contract management
- part C – when things go wrong
- part D – general
1.2.2 NHS England will update and refine policies periodically and following changes in legislation, contracts or central policy and guidance. Users of this PGM are advised this is a controlled document and the most up to date version should always be used. That is, the version which is published on NHS England’s website.
1.3 Transitional arrangements
1.3.1 This PGM replaces all previous versions. In addition, we have embedded as chapters some other related policy/guidance that have been published by NHS England as standalone documents since the original ‘policy book’ was published in July 2016. The processes and procedures set out in this PGM must be followed where a matter arises after the date of publication of this PGM.
1.3.2 Where a matter arose prior to the publication of this PGM (and the parties are therefore following a previous policy) the parties should continue to follow that previous policy as this would have been the expectation of the parties at the time.
1.3.3 Parties following a previous policy should consider switching to the relevant policy set out in this PGM if there is a natural transitional point in the matter and provided all parties agree.
2 The legislation, abbreviations and acronyms
2.1 Links to legislation and other relevant law
2.1.1 The legislation and law applying to primary medical services may be amended from time to time. It is important that users of the PGM are familiar with the relevant in force published documentation.
2.1.2 The PGM must be read in conjunction with the relevant law, which may not be repeated in full in this PGM.
2.1.3 However, to assist users of the PGM, the links below provide access to the relevant documents content pages from where the user may find the appropriate section, regulation etc.:
- Equality Act 2010
- Equality Act 2010 (Specific Duties and Public Authorities) Regulations 2017
- National Service Act 2006
- Health and Social Care Act 2012
- Health and Care Act 2022
- The National Health Service (General Medical Services Contracts) Regulations 2015
- The National Health Service (Personal Medical Services Agreements) Regulations 2015
Note: while www.legislation.gov.uk updates legislation, at any point in time there may be outstanding amendments therefore users are advised to ensure they are familiar with current amendments pending any updating as appropriate.
2.1.4 The law published in directions can be found on the gov.uk website and, at the time of publishing this PGM, the links below provide access to some relevant documents as originally published as a whole from where the user may find the appropriate direction, paragraph etc.:
- Alternative Provider Medical Services Directions
- General Medical Services Statement of Financial Entitlements Directions
- The Primary Medical Services (Directed Enhanced Services) Directions
Note: any subsequent amending directions are not updated, and users are advised to ensure they are familiar with current amendments until any subsequent publication as appropriate.
2.2 Abbreviations and acronyms
The following abbreviations and acronyms are used in the PGM:
- APMS – alternative provider medical services
- APMS directions – alternative provider medical services directions
- CCG – clinical commissioning group
- COSHH – control of substances hazardous to health
- CQC – Care Quality Commission
- GMS – general medical services
- GMS regulations – The National Health Service (General Medical Services Contracts) Regulations 2015
- GMS SFE – general medical services statement of financial entitlements directions
- GP – general practitioner
- HWB – health and wellbeing board
- ICB – integrated care board
- ICS – integrated care system
- LMC – local medical committee
- NBM – new business models
- NHS – Act National Health Service Act 2006
- PSR – provider service regime
- NHSR – NHS Resolution
- PCA – Primary Care Appeals (Part of NHSR)
- PCSE – Primary Care Support England (delivered by Capita on behalf of NHS England)
- PCN – primary care network
- PHSO – Parliamentary and Health Service Ombudsman
- PMS – personal medical services
- PMS Regulations – The National Health Service (Personal Medical Services Agreements) Regulations 2015
- TUPE – Transfer of Undertakings (Protection of Employment) Regulations 2006
Staff working with the NHS may also find this acronym buster helpful (which provides a broader list of NHS acronyms in use beyond this document), alongside our understanding the NHS section.
3 Commissioning described
3.1 Background and delegated commissioning (2014 – 2022)
3.1.1 In May 2014, NHS England invited CCGs to come forward with expressions of interest to take on an increased role in the commissioning of primary medical services empowering and enabling CCGs to improve primary care services locally for the benefit of patients and local communities.
3.1.2 Known as co-commissioning, CCGs collaborated closely with NHS England to ensure that decisions taken about healthcare services were strategically aligned across the local health economy. Joint commissioning arrangements allowed CCGs and NHS England to effectively plan and improve the provision of out of hospital services for the benefit of patients and local populations.
3.1.3 Delegated commissioning was an opportunity for CCGs to assume full responsibility for commissioning general practice services. Legally, NHS England retained the residual liability for the performance of primary medical services commissioning. Therefore, NHS England required robust assurance that its statutory functions were discharged effectively.
3.1.4 The following primary medical functions were included in CCG delegated arrangements:
- GMS, PMS, APMS (including the design of PMS and APMS contracts, monitoring of contracts, taking contractual action, such as issuing breach/remedial notices, and removing a contract)
- newly designed enhanced services (“Local Enhanced Services (LES)” and “Directed Enhanced Services (DES)”)
- design of local incentive schemes as an alternative to the Quality and outcomes framework (QOF)
- the ability to establish new GP practices in an area
- approving practice mergers
- making decisions on ‘discretionary’ payments
3.1.5 Delegated commissioning arrangements exclude reserved functions such as individual GP performance management (medical performers’ list for GPs, appraisal, and revalidation). NHS England retaining responsibility for the administration of payments and list management.
3.2 ICB delegated commissioning arrangements
3.2.1 From July April 2022, ICBs assumed delegated responsibility for primary medical services excluding Section 7A Public Health functions. From April 2023 ICBs assumed delegated responsibility for dental (primary, secondary and community), general ophthalmic services and pharmaceutical services.
3.2.2 NHS England retain reserved functions such as performers list management, and wider aspects of professional regulation. Further functions retained nationally include:
- identifying national priorities, setting outcomes, and developing national contracts or contractual frameworks
- maintaining national policies and guidance that will support ICBs to be effective in their delegated functions
- delivering support services
3.3 Primary care policies
3.3.1 For the purposes of the primary care policies, the commissioner of the primary care service is not referred to by name but simply as the “commissioner”. This reflects the fact the identity of the commissioner in an area is a delegated ICB (see Executive summary on the Health and Social Care Act 2022), which abolished clinical commissioning groups and created ICBs.
3.3.2 Although ICBs may assume the role of the commissioner for the purposes of the policies, for ICB delegation, legally NHS England retains the residual liability for the performance of primary medical services commissioning. However, there will be matters which have not been delegated to ICBs or are not able to be carried out by an ICB in which case the commissioner will be NHS England.
3.3.3 ICB under delegated commissioning arrangements, an ICB will have agreed on a delegation agreement with NHS England. This document will set out for what matters the ICB has decision-making responsibilities. Where the delegation agreement sets out obligations on the ICB, eg liaising with NHS England in relation to managing disputes, the relevant primary medical policy refers to the delegation agreement and highlights relevant points.
Equality and health inequalities
3.3.4 ICBs and NHS England have legal duties in respect of equality and health inequalities. Supporting guidance has been issued within the 2020-2021 planning and contracting guidance, Guidance for NHS commissioners on equality and health inequalities legal duties. A number of data and analysis tools are published by Public Health England (eg the Inequalities calculation tool). In the commissioning and operational implementation of primary medical services due regard should be given to these duties. Further detail is also provided in the next section.
3.4 Primary care networks
3.4.1 Primary care networks (PCNs) build on the core of current primary care services and enable greater provision of proactive, personalised, coordinated and more integrated health and social care, with greater collaboration between general practice and other local system partners including community pharmacy, local authorities, social care, community providers, mental health providers and voluntary services. Clinicians describe this as a change from reactively providing appointments to proactively caring for the people and communities they serve. PCNs can also help to provide stability and resilience for practices.
3.4.2 Refreshing NHS plans for 2018-19 and the NHS Long Term Plan prefigured the formal intention that every practice should be part of a PCN, covering the whole country. This was delivered as part of Investment and evolution: the five-year framework for GP contract reform which introduced from 1 July 2019 a new directed enhanced service – “the network contract DES”. Its goal is to ensure general practice plays a leading role in every PCN and enables much closer working between PCNs and their integrated care board.
3.4.3 PCNs are based on GP registered lists and are made up of a practice or practices (and possibly other providers) typically serving natural communities of around 30,000 to 50,000 people. These parameters mean that PCNs are small enough to provide the personal care valued by both patients and GPs, but large enough to have impact and economies of scale through better collaboration between practices and others in the local health and social care system.
3.4.4 Find out more through case studies from across the country where primary care networks are already making a difference to staff and patients.
3.4.5 In March 2023 (and updated yearly), NHS England published the Network contract DES – contract specification – PCN requirements and entitlements, setting out eligibility requirements and the rights and obligations of practices, PCNs and commissioners under the DES. A range of additional information to assist commissioners and providers in further developing PCNs is also available on the NHS England GP contract page.
4 General duties of NHS England (including addressing health inequalities)
4.1 Introduction
4.1.1 This chapter outlines the general duties that NHS England must comply with that are likely to affect the decisions it takes regarding the provision of primary care.
4.1.2 ICBs carrying out commissioning under delegated authority do so on behalf of NHS England. ICBs need to comply with NHS England’s legal duties when doing this – this is set out in the delegation agreement. Therefore, this chapter is also relevant to ICBs.
4.1.3 In many instances the duties placed on NHS England are mirrored by similar duties placed on ICBs. We have highlighted the equivalent ICB duty. However, this note does not cover any further ICB duties that apply only to ICBs and not to NHS England.
4.1.4 There are many general duties on commissioners. It is important that decision-makers are familiar with all these duties because if a duty has not been complied with when a decision is taken, that decision can be challenged in the courts on the grounds that it is unlawful.
4.1.5 This guidance looks at the general duties that commissioners are required to comply with that are most applicable to primary care, providing examples to illustrate how they might affect decision making.
4.1.6 As has been noted, under delegation arrangements NHS England retains the legal responsibility for compliance with the duties in respect of primary medical services commissioning. Accordingly, NHS England will require assurance that its statutory functions are being discharged effectively by an ICB. This underlines the importance of compliance with the duties outlined in this chapter.
4.1.7 Below is a summary of the duties that are covered by this chapter. The chapter (from 2 onwards) goes on to look at each of the duties in more detail. A table of contents is also provided for clarity.
Duties covered in this chapter – table of contents
- summary of duties covered by this chapter
- equality and health inequalities duties
- other non-equality and health inequalities related duties
Summary of duties covered by this chapter
Equality and health inequalities duties
Equality Act 2010
The Equality Act 2010 prohibits unlawful discrimination in the provision of services on the grounds of age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation. These are the “protected characteristics”.
As well as these prohibitions against unlawful discrimination, the Equality Act 2010 requires commissioners to have “due regard” to the need to:
- eliminate discrimination that is unlawful under the Equality Act
- advance equality of opportunity between people who share a relevant protected characteristic and people who do not share it; and
- foster good relations between persons who share a relevant protected characteristic and persons who do not share it
This can require NHS England to take positive steps to reduce inequalities.
The duty is known as the public sector equality duty or PSED (see section 149 of the Equality Act 2010). The Equality Act 2010 also imposes (through regulations made under the Act) particular inequality related duties on commissioners. Failure to comply with these specific duties will be unlawful.
NHS Act 2006 (as amended by the Health and Social Care Act 2012)
Under the NHS Act 2006 (as amended by the Health and Social Care Act 2012) commissioners also have a duty to have regard to the need to:
- reduce inequalities between patients with respect to their ability to access health services; and
- reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services
- (in respect of NHS England, see section 13G of the NHS Act 2006; and, in respect of ICBs, see section 14T of the NHS Act 2006)
Other non-equality and health inequalities related duties
The “regard duties”
In addition to the above, there are other obligations on commissioners to “have regard” to particular factors. These are set out in the NHS Act 2006 (as amended by the Health and Social Care Act 2012).
The other “regard duties” are:
- the duty to have regard to the desirability of allowing others in the healthcare system to act with autonomy and avoid imposing unnecessary burdens upon them, so far as this is consistent with the interests of the health service (in respect of NHS England, see section 13F of the NHS Act 2006)
- the duty to have regard to the need to promote education and training of those working within (or intending to work within) the health service (in respect of NHS England, see section 13M of the NHS Act 2006; and, in respect of ICBs, see section 14Z of the NHS Act 2006)
- the duty to have regard to the likely impact of commissioning decisions on healthcare delivered in areas of Wales or Scotland close to the border with England (in respect of NHS England, see section 13O of the NHS Act 2006)
The “view to duties”
The “view to duties” are:
- the duty to act with a view to delivering services in a way that promotes the NHS constitution (in respect of NHS England, see section 13C(1)(a) of the NHS Act 2006; and, in respect of ICBs, see section 14P of the NHS Act 2006)
- the duty to act with a view to securing continuous improvement in the quality of services in health and public health services (in respect of NHS England, see section 13E of the NHS Act 2006; and, in respect of ICBs, see section 14R of the NHS Act 2006)
- the duty to act with a view to enabling patients to make choices about their care (in respect of NHS England, see section 13I of the NHS Act 2006; and, in respect of ICBs, see section 14R of the NHS Act 2006)
- the duty to act with a view to securing integration, including between health and other public services that impact on health, where this would improve health services (in respect of NHS England, see section 13N of the NHS Act 2006; and, in respect of ICBs, see section 14Z1 of the NHS Act 2006)
The “promote duties”
The “promote duties” are:
- the duty to promote awareness of the NHS Constitution among patients, staff and members of the public (in respect of NHS England, see section 13C(1)(b) of the NHS Act 2006; and, in respect of ICBs, see section 14P(1)(b) of the NHS Act 2006)
- the duty to promote the involvement of patients and carers in decisions about their own care (in respect of NHS England, see section 13H of the NHS Act 2006; and, in respect of ICBs, see section 14U of the NHS Act 2006)
- the duty to promote innovation in the health service (in respect of NHS England, see section 13K of the NHS Act 2006; and, in respect of ICBs, see section 14X of the NHS Act 2006)
- he duty to promote research and the use of research on matters relevant to the health service (in respect of NHS England, see section 13L of the NHS Act 2006; and, in respect of ICBs, see section 14Y of the NHS Act 2006)
The “involvement duty”
Commissioners have a duty to make arrangements to secure that service users and potential service users are involved in:
- the planning of commissioning arrangements by commissioners
- the commissioners’ development and consideration of proposals for changes to commissioning arrangements, if the implementation of the proposals would impact on the range of health services available to service users or the manner in which they are delivered
- the commissioners’ decisions affecting the operation of commissioning arrangements, if those decisions would have such an impact
(in respect of NHS England, see section 13Q of the NHS Act 2006; in respect of ICBs, see section 14Z2 of the NHS Act 2006)
Duty to act fairly and reasonably
Commissioners have a duty to act fairly and reasonably when making its decisions. These duties come from case law that applies to all public bodies.
Duty to obtain advice
Commissioners have a duty to “obtain appropriate advice” from persons with a broad range of professional expertise (in respect of NHS England, see section 13J of the NHS Act 2006; and, in respect of ICBs, see section 14W of the NHS Act 2006)
Duty to exercise functions effectively
Commissioners have a duty to exercise their functions effectively, efficiently and economically (in respect of NHS England, see section 13D of the NHS Act 2006; and, in respect of ICBs, see section 14Q of the NHS Act 2006)
Duty not to prefer one type of provider
Commissioners must not try to vary the proportion of services delivered by providers according to whether the provider is in the public or private sector, or some other aspect of their status.
5 Working together – commissioning and regulating
5.1 Introduction
5.1.1 This chapter is intended to inform commissioners of work to establish a robust and practical joint working framework.
5.2 Background
5.2.1 Alongside the publication of the GP Forward View (NHS England, 2016), a statement of intent was published by the main national regulatory and assurance bodies, committing to working together with professional bodies and those using services in the development of a shared view of quality in general practice. This would provide the basis of a joined-up approach to monitoring and improvement of quality.
5.2.2 The Regulation of General Practice Programme Board was established in June 2016 to:
- coordinate and improve the overall approach to the regulation of general practice in England by bringing together the main statutory oversight and regulatory bodies and delivering a programme of work which will streamline working arrangements and minimise duplication
- provide a forum for sign-up by statutory bodies to a common framework – a shared view of quality – which will be co-produced with the professions and the public
5.3 Implementation
5.3.1 The Care Quality Commission (CQC), NHS England, and NHS Clinical Commissioners (NHSCC), with the support of the General Medical Council (GMC), published a joint working framework in 2018.
5.3.2 The framework recognises that in many areas’ relationships between commissioners and CQC are working well; in other areas, the framework is intended to help provide structure and support for new relationships with examples of good practice.
5.4 Existing good practice and interim principles
5.4.1 Significant steps have already been taken to streamline processes and share information:
- NHS England regularly share eDec data and information with CQC
- NHS England will share eDec data with all commissioners, including analysis and outlier reports to help commissioners target support locally
- CQC share inspection rating updates every week with NHS England
- CQC share inspection schedules with commissioners wherever possible
- commissioners share local information and intelligence with CQC and NHS England
- in some areas commissioners work closely with GP practices prior to inspections to support them
5.4.2 Collaborative working arrangements:
5.4.3 Positive working relationships are critical for ensuring successful partnership working. Commissioners and CQC have established some formal mechanisms for ensuring successful collaborative working, but these should not be seen as the only means by which those relationships can be developed. We also recognise the role of quality surveillance groups and other forums that have been established for information sharing in some areas of the country.
5.4.4 It is recognised that telephoning the right person at the right organisation at the right time is the best means of developing those relationships and avoiding duplication wherever possible. It is important that commissioners engage with and know their local contacts.
5.4.5 Existing good practice:
- all parties will be transparent, and we will ensure information governance and data protection principles are adhered to without exception and we will ensure GP practices are fully sighted on this
- commissioners should actively and effectively communicate with each other and CQC to ensure GP practices are not overburdened, eg to avoid the situation whereby a commissioner contract visit overlaps with a CQC inspection
- commissioners should keep in regular contact with CQC throughout the year and more targeted and regular communication on the run-up to inspection or annual review
- commissioners should actively engage with and support GP Practices pre- and post-inspection
5.5 Why
5.5.1 The system of medical regulation has evolved over time, rather than having been designed from a single agreed blueprint. There is a perception within the medical profession that it is over-regulated, with too many bodies setting standards and imposing requirements with potential for regulatory overlap. A lack of clarity about which body is responsible for which areas of monitoring and regulation carries a risk of duplication, but also of potential gaps in the system which is designed to ensure patient safety.
1.5.2 These overlaps exist
- between CQC GP practice requirements and GMC revalidation requirements
- between evidence sought by NHS England for contract compliance and CQC’s regulatory requirements
- between NHS England in its oversight role of the national performers list (NPL) and GMC’s regulation of GPs on the GP register
- between NHS England in its oversight of national contracts and ICBs in their oversight of local contracts and accountability for system performance
1.5.3 NHS England, CQC and GMC already work closely together to share data but there is more work to be done to align our processes and minimise the workload for general practice.
5.6 The ambition being delivered
NHS England, CQC and GMC are committed to;
- identifying immediate actions to support GPs and GP practices to reduce the workload associated with regulation
- align and streamline regulatory and commissioning processes taking a more targeted and risk-based approach to regulation and contract management
- improved information gathering and intelligence about services – we need to ensure that the data and information we identify to collect, measure, and monitor, is clear and consistent, and proportionate to risk
- making it easier for commissioners and regulators to access and use shared information about quality, giving GPs time to focus on improving quality of care at the frontline.
Part B – general contract management
1 Contracts described
1.1 Comparison of contract types
1.1.1 Throughout this document there are many references to standard contracts General Medical Services (GMS), Personal Medical Services (PMS) and Alternative Provider Medical Services (APMS). In addition to the statutory provisions regarding eligibility in 1.2, 1.3 and 1.4 below, the following table provides a quick comparator between the 3 contract types:
|
|
GMS contract |
PMS agreement |
APMS contract |
|
Is the contract time limited? |
No Except in certain circumstances when a temporary GMS contract (see 1.1.2) can be used – see urgent contracts below |
Yes Note that a PMS contractor providing essential services may apply for a GMS contract any time prior to the end of the PMS agreement |
Yes |
|
Can the commissioner terminate at will? |
No |
Yes |
If agreed by the parties and contained within the contract |
|
Must the contractor provide essential services? |
Yes |
No |
No |
|
Is there a standard form contract? |
Yes |
Yes |
Yes |
|
Does the standard form contract contain key performance indicators (KPIs)? |
No |
No |
No |
|
Can KPIs be added? |
KPIs can be agreed between the parties in relation to supplementary quality-based services |
Yes |
Yes |
|
Payment arrangements | GMS statement of financial entitlement directions(SFE) |
As agreed by the parties and contained within the agreement – there may be reference to the GMS SFE |
As agreed by the parties and contained within the contract |
1.1.2 Following the termination of a GMS contract, NHS England and integrated care boards (ICBs) have the authority, as per regulation 16(2) of the GMS regulations, to enter into a temporary GMS contract with a contractor. This contract allows the provision of primary medical services to the former patients of the terminated contractor for a maximum period of 12 months. The purpose of this temporary contract is to allow sufficient time for a competitive tendering exercise to be conducted, enabling the establishment of a new contract.
1.1.3 While it is preferable, commissioners are advised against entering into a temporary GMS contract due to the associated risks. The APMS contract is typically commissioned for a predetermined period of time, and competing providers would have understood that the contract would only be awarded to the successful provider for a specific duration. Consequently, the market expects that there will be an opportunity to compete for the contract at some point. Merging with a GMS contract would eliminate that possibility.
1.2 Statutory provisions: persons eligible to enter into GMS contracts
1.2.1 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to ‘the commissioner’.
1.2.2 Section 86 of the NHS Act sets out the types of persons (including organisation types) that may enter into a GMS contract.
- In Section 86: “health care professional”, “NHS employee”, “section 92 employee”, “section 107 employee”, “section 50 employee”, “section 64 employee”, “section 17C employee” and “Article 15B employee” have the meaning given by section 93.
1.2.3 GMS regulations, part 2, regulations 4 to 6 set out the eligibility criteria that must be satisfied before any of the types of persons set out in section 86 of the NHS Act can enter into the GMS contract.
1.3 Statutory provisions: persons eligible to enter into a PMS agreement
1.3.1 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to ‘the commissioner’.
1.3.2 Section 93 of the NHS Act sets out the types of persons (including organisation types) that may enter into a PMS agreement (referred to in the Act as 3ection 92 agreements).
- In Section 93: “health care professional”, “NHS employee”, “section 92 employee”, “section 107 employee”, “section 50 employee”, “section 64 employee”, “section 17C employee” and “Article 15B employee” have the meaning given in this section.
1.3.3 PMS regulations, part 2, regulations 4 and 5 set out the eligibility criteria that must be satisfied before any of the types of persons set out in Section 93 of the NHS Act can enter into the PMS agreement.
Note: where 2 or more persons operate their practice as a partnership, the PMS agreement is not treated as being made with that partnership rather the persons agree to contract together as ‘the contractor’.
1.4 Statutory provisions: persons eligible to enter into an APMS contract
1.4.1 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to ‘the commissioner’.
1.4.2 The NHS Act does not list persons who may (or may not) enter into an APMS contract.
1.4.3 The APMS directions 4 and 5 contain provisions relating to circumstances in which certain types of persons or organisation may not enter into an APMS contract. Provided direction 5 does not apply, any person or organisation may enter into an APMS contract.
1.5 Urgent contracts
1.5.1 Circumstances may arise that require the commissioner to put in place an urgent contract. Such circumstances may include:
the death of a contractor
the bankruptcy or insolvency of a contractor
termination of an existing contract due to patient safety
1.5.2 Where continuity of services to patients is required, the short timescales involved may not allow the commissioner to undertake a managed closedown and transfer to a new provider (details of which are set out in the chapters on planned and unplanned practice closedown). Additional information can also be found in the unplanned closures chapter. The commissioner may therefore, look to award a contract to a specific party that is able to provide the services to patients at short notice.
1.5.3 Prior to awarding a contract in this scenario, the commissioner should consider a number of factors that are set out in the paragraphs below.
Procurement
1.5.4 Commissioners should defer to the published statutory guidance on the provider selection regime (PSR). The urgent provisions within the regime may apply to secure immediate needs, eg to establish caretaker arrangements. However, as this will be a temporary arrangement it must be reconsidered after a set period. The statutory guidance provides further information about proper application.
Premises
1.5.5 The previous contractor may own or lease the premises which, as a result, may not be available for the provision of the services under a new contract. The availability of the premises must be ascertained before entering into a temporary contract.
Primary care networks
1.5.6 The commissioner should facilitate a discussion between the incoming contractor and the primary care network (PCN) to which the outgoing contractor was a member, involving the relevant local medical committee (LMC), with the expectation that PCN membership should be maintained in order to ensure that patients continue to receive uninterrupted network services.
1.5.7 If the contractor is still not willing to join the PCN then the commissioner will work with the existing PCN core network practices (GP practices who signed up to and are responsible for delivering the requirements of the network) to ensure continuity of services to its registered patients.
1.5.8 If the PCN is not prepared to accept the contractor as a member, the commissioner may require a PCN to include the practice as a core network practice of that PCN. Where the commissioner is minded to require a PCN to do so, the commissioner must engage with the relevant LMC and, when making its determination, have regards to the views of the LMC. Section 4.6 of the Network Contract DES 2021/22 – PCN requirements and entitlements sets out the process for allocating a practice to a PCN.
1.6 Public involvement
1.6.1 One of the general duties of commissioners is to ensure there is public involvement where a decision leads to an impact on the provision of primary care services. If under a new contract, services are provided from a different location, this will be an impact on the services which may trigger the need to undertake a public involvement exercise.
1.6.2 Where there is no time for undertaking an exercise prior to entering into the contract, the commissioner should ensure that as soon as possible after the contract is entered into, it arranges for such an exercise to be undertaken prior to the commissioner making any decisions about the long-term provision of services.
Commissioner standing orders (SOs) and standing financial instructions (SFIs)
1.6.3 The commissioner may have organisational standing orders and standing financial instructions that require contracts to be procured in certain ways, eg securing three quotes for contracts up to a certain financial value. Where time does not allow the rules to be followed, there may be an emergency process that must be followed.
Other factors
1.6.4 Further factors may be relevant depending on the circumstances of the matter. Please refer to the chapters on planned and unplanned practice closures for a list of all factors that may be relevant.
1.6.5 Commissioners should also consider that if a practice has closed because of concerns in relation to patient safety, the incoming provider may need to be commissioned to undertake a review of systems and processes. This should include but is not limited to, undertaking audits to provide assurance around patient safety. This recognises the additional work that commissioners may need to reflect in the contract to provide assurance with regard to patient safety and public confidence.
Which contract form?
1.6.6 A GMS contract can be used where the commissioner has terminated a contract of another provider of primary medical services, and as a result of that termination, it wishes to enter into a temporary contract for a period specified in the contract for the provision of services.
1.6.7 A time limited PMS agreement may not be attractive in this scenario as the PMS contractor, if providing essential services, can request a non-time limited GMS contract at any time.
1.6.8 It is common for APMS contracts to be used in such a scenario due to the flexibility of:
types of organisations that can enter into APMS contracts
flexibility of types of services and payment mechanism that can be agreed
flexibility around duration and termination provisions
1.6.9 The commissioner should therefore consider what services and duration is required and whether there are any restrictions on the proposed contractor entering into different contract types to meet local diverse health needs.
1.7 Primary care support services notifications
1.7.1 Commissioners should ensure that following any contract award or contract merger, GP performers are informed of their obligation to notify within 28 days Primary Care Support England using the forms issued by NHS England’ or preferably the online portal.
1.7.2 Additionally, and more generally, GP performers and indeed performers in all contractor groups are required to notify the primary care support services (PCSS) provider of any changes relevant to their entry on the national performers list. Further information is available on the NHS England website.
1.8 Working with Primary Care Support England (PCSE) (delivered on behalf of NHS England by Capita)
1.8.1 Brief introduction to PCSE.
1.8.2 In September 2015, PCSE took on responsibility for the delivery of NHS England’s primary care support services. PCSE provides support services to GP practices, pharmacies, dentists and opticians. For general practices they provide services covering:
- registrations and list maintenance (Exeter (and successor systems, eg Primary Care Registration Management (PCRM) system) and Personal Demographics Service (PDS)
- medical records – responsible for moving hard copy patient medical records and temporary patient records between practices and into storage
- supplies – providing NHS stationery, pre-printed forms, needles and syringes via an online portal
- GP payments and pensions – administrating monthly contracts and reimbursements to GP practices
- The National Performers List (NPL) – administering entry and changes to performers lists on behalf of NHS England
- Open Exeter – providing access control support for Open Exeter for cervical screening users
- practice mergers and closures – administering the mergers and closures of GP practices
2 Assurance framework for contract reviews
2.1 Introduction
2.1.1 Commissioners of primary medical services are responsible for the quality, safety and performance of services delivered by providers, within their area of responsibility. ICBs must have due regard to their obligations as set out within the delegation agreement which includes adherence with policies and guidance issued by NHS England, including this PGM.
2.1.2 Commissioners also have a statutory duty to conduct a routine annual review of every primary medical services contract it holds. This is covered through the General Practice Annual Electronic Self-declaration (eDec) collection which NHS England has established with providers (and is currently delivered by NHS England). Commissioners should ensure they review practice eDec returns following submission. NHS England produces subsequent national analysis to support commissioners identify variation or matters of declared non-compliance (eg NHS England’s eDec outlier report which will usually be made available 6-8 weeks following eDec closure).
2.1.3 This chapter outlines the approach to be taken by commissioners when overseeing primary medical services contracts to ensure compliance with quality and safety standards.
2.1.4 It is important to note that whilst exercising of the function has passed to ICBs, NHS England remains accountable. Assurance of ICBs commissioning of primary medical services will be covered outside of this PGM.
2.1.5 Commissioners are reminded that early engagement with LMCs presents the best opportunity to support practices in making effective and sustainable changes to support service improvement, should this be found to be appropriate and necessary.
2.1.6 This chapter provides an outline framework for assessing general practice services delivered through the normal contractual routes (ie GMS, PMS and APMS).
2.1.7 This chapter will not re-cover details of the various types of contracts or the contractual actions available as these are covered elsewhere within this PGM. It will aim to provide practical advice and guidance to support commissioners and contract managers.
2.2 Background
2.2.1 Whilst it is recognised that most health care professionals and providers of primary medical services operate to a very high standard, it is essential that commissioners have robust monitoring arrangements in place.
2.2.2 Monitoring arrangements should create a balance of support, oversight and intervention where necessary. Furthermore, it should create a culture of openness and transparency and a vehicle to promote peer to peer improvement.
2.2.3 Whilst practices as providers are accountable for the quality of services and are required to have their own quality monitoring processes in place, commissioners have a responsibility for quality assurance. Through the duty of candour and the contractual relationship with commissioners, practices are required to provide information and assurance to commissioners and engage in system wide approaches to improving quality.
2.3 Contract review
2.3.1 Through the publication of this guidance, NHS England introduced a requirement on commissioners to undertake a risk-based approach to reviewing contracts, along with a rolling programme of deep-dive contract reviews. Depending on the number of practices within the commissioning area and types of contracts, a rolling programme could span one to three years.
2.3.2 For APMS contracts this would need to be more frequent owing to the length of contract and the variable key performance indicators within them. It is recommended that if new information becomes available to the commissioner which suggests high levels of variation, a visit may be required and the contract reviewing further.
2.3.3 Commissioners will have varying resources available to effectively manage their range of contract. Nationally, there are (as of June 2021) 6,571 practices in England.
2019/20 data published by NHS England (table below) suggests that a breakdown of practices into the following contract types |
GMS |
PMS |
APMS |
Unconfirmed contract type |
All contract types |
Total number of practices |
4,917 (70%) |
1,794 (26%) |
180 (2%) |
110 (2%) |
7,001 |
2.3.4 However, these masks a range of GP practice numbers and contract types across ICBs.
2.3.5 Commissioners should maintain accurate records of all contract reviews and will be required to demonstrate if requested, evidence of compliance, or otherwise support oversight of primary care commissioning arrangements. This may be for example via NHS England’s assurance arrangements or internal and external audit functions.
2.4 Setting and monitoring key performance indicators
2.4.1 Commissioners should ensure key performance indicators (KPIs) are negotiated into relevant contracts. These should be specific, measurable, achievable, relevant and time-bound (SMART) and include relevant payment thresholds.
2.4.2 Primary medical services providers will then be required to submit evidence to the commissioner in relation to those KPIs, against which payment will be considered. The commissioner should be assured that the evidence submitted by the contractor is robust, relevant and proportionate.
2.5 Using data and information effectively
2.5.1 This section recognises that in a model for improvement, various data sets which are being used by commissioners to oversee the delivery of services provide only one part of a large picture and used in isolation presents not only a risk of inaccuracy, but anxiety amongst those providing services or those responsible for oversight of the delivery of those services. Data must be put into the context of the particular provider practice and used alongside other intelligence to gain a full understanding of any potential risk to quality and patient safety.
2.5.2 The use of measures and indicators to assess quality should not remove, diminish, or unduly influence sound evidence based clinical decisions and judgements. Commissioners should take steps to ensure that indicators are not abused as perverse incentives to change clinical practice or ways of working which are inconsistent with the delivery of high-quality patient centred care.
2.5.3 Whilst most health care professionals practise to a very high standard and it is recognised that there is excellence in general practice, it is essential that commissioners have in place a robust assurance management programme to identify and share best practice, recognise where additional management may be needed and to highlight when things are going wrong at an early stage in primary medical services provision.
2.5.4 Through transparent measurement across practices within the commissioning area, the practice-commissioner relationship provides a forum for collaborative and engaging discussions. Such engagement and collaboration recognise the contribution that each practice can make to both the quality of services to their registered patients and the wider impact to service delivery across the practice and wider ICB population.
2.5.5 The usage of measures and indicators is to act as a starting place for conversations, asking questions along the way as to why variation may be occurring and acknowledging that variation may be warranted or unwarranted depending on the context and wider supporting information available. A practice visit may be needed to support further understanding when high levels of variation are occurring.
2.5.6 If there are greater concerns about a practice, bordering on contractual failure, this will require a more formal conversation with the practice which should be led by the commissioner. The focus will be the same for all practices: support to improve, with market exit as a last resort.
2.5.7 Recognising that practice specific data alone is not conclusive evidence of poor service provision and needs to be considered within the context of the practice, the commissioner will use a collection of information including national data (clinical indicators, quality outcome standards, appraisals, complaints etc.) and local intelligence (including conferring with stakeholders) in order to assess and mitigate any potential risk to service provision and patient safety within a practice. Where a potential or actual risk is identified, the commissioner will be expected to take the necessary steps to assure itself that adequate and effective support is being provided to reduce the risk, identify any ongoing areas for improvement and be able to demonstrate and measure that improvement.
2.5.8 NHS England provides commissioners and GP practices with a centrally available set of pre-analysed data which the commissioner must use as part of its assessment of variation in the provision of primary medical services. This information has been developed and made available through a restricted access web interface available on the Primary Care Indicators website. Commissioners will be expected to use these sources of data and information to support contract monitoring.
Note: in response to the impact of covid-19 pandemic on the data (eg suspension of the Quality and Outcomes Framework (QOF) etc.) the banding terminology for primary care indicators was changed to refer only to the extent of benchmarked variation in a practice’s indicator value rather than assessment of performance (see table below). NHS England will continue to work with stakeholders on when it is appropriate to revert to the former terminology.
|
Pre-pandemic banding terminology |
Banding used during the pandemic (from April 2021) |
|
Review identified |
High variation |
|
Approaching review |
Medium variation |
|
Achieving |
Low variation |
|
Higher achieving |
No variation |
2.5.9 Recognising the commissioner retains contractual accountability and relying on the practice/commissioner /LMC relationship, supported by a centrally provided transparent and consistent suite of measures, in conjunction with robust, fair and consistent guidance for the management of service and performance improvement, will help to ensure risks to quality and patient safety are addressed in a timely and proportionate manner.
2.5.10 The approach described above provides for the commissioner to assure the quality, safety and performance of each practice.
2.5.11 The Care Quality Commission (CQC) is the independent regulator of health and adult social care in England. It seeks to ensure services are safe, effective, compassionate, and delivered to a high quality, encouraging services to improve. The inspection of general practice includes 5 key questions of services ie whether services are: safe, effective, caring, responsive to people’s needs and well-led. CQC rates each of the 5 questions to give an overall rating for a practice, the rating categories used include: outstanding, good, requires improvement and inadequate. These ratings and practice reports are available on the CQC website.
2.5.12 CQC’s report State of Care in General Practice 2014-2017 highlighted that one of the key determinants of GP practices providing high quality care was, a practice that is proactive in identifying the needs of their patient population as well as people’s health and care needs in the wider local population. Furthermore, practices that were good or outstanding proactively support people to live healthy lives, recognise social aspects such as employment, housing and finance and then target such support towards people who are vulnerable. As well as engaging with the needs of patients, meeting local needs also meant engaging with external agencies, and networks and including the voluntary sector. CQC rating data indicates that the majority of practices in England are rated as good or outstanding, with pockets of poor practice.
2.5.13 The standards set by the CQC describe the characteristics of ‘good’ quality primary medical services. These are available on the CQC website.
2.5.14 Other definitions of good quality primary care which may also provide the starting point for discussions between practices and the commissioner are outlined in the Health Foundation publication Improving quality in general practice.
2.5.15 As excellent service provision cannot be discerned from a single set of measures or indicators, NHS England primarily provide 3 sources of data and intelligence. Used alongside local knowledge, these may assist the commissioner in assessing risk to service provision and patient safety and therefore adherence to the contract. This intelligence is currently provided through the Primary Care website and through eDec which is collected by NHS England via the Strategic Data Collection Service (SDCS).
1. A practice profile which describes the characteristics of each practice, eg the demography of the population served. This information is updated regularly and whilst it is unlikely to change significantly over time, it may contain specific information which when presented alongside clinical indicators, would provide a more complete picture and potential impact on achievement of certain standards, eg the effect of student practices or those that serve more discreet populations (homeless, high ethnic minority, highly deprived etc).
2. The annual General Practice Electronic Self-Declaration (eDec). This includes information such as, operating policies, opening times and assurance of good workforce planning. This information will link with contractual requirements and may also contain responses to ‘reasonable requests for information’, eg from other governmental departments and bodies, parliamentary questions or freedom of information requests. The information declared will be shared with CQC, reducing the burden of separate information returns across organisations, eg as part of pre-inspection information requests.
3. A suite of general practice measures and indicators supporting quality improvement, assurance and enabling benchmarking as these are shared transparently with all practices. This indicator set applies to all GP practices in England, in order to allow for benchmarking comparisons to be made, within an ICB or wider regional areas, for example by grouping practices of other similar characteristics such index of multiple deprivation and list size, etc.
2.5.16 These data should be used by commissioners in the first instance, along with any new or emerging sources of intelligence to identify risk. These sources of data and information will direct commissioners to those areas where potential areas or pockets of highest risk exist.
2.5.17 It is acknowledged that these sources of data do not capture the full range of services provided by general practice, they are however an important starting point in helping individual practices, Commissioners, and other stakeholders to build a rounded view of performance with a focus on objective service improvement and outcomes.
2.5.18 There are very few circumstances where data alone will determine commissioner intervention. To ensure flexibility, commissioners should review these 3 primary sources of data and any future published sources of data and information in order to understand whether a practice requires support to improve or intervention, for example, if the commissioner considers there may be a risk to quality and patient safety. If necessary, the commissioner should provide additional appropriate and adequate support to be agreed with the practice. If despite that support a practice is unable to demonstrate improvement within a reasonable period, the commissioner must determine whether it considers there is an actual cause for concern. This will require scrutiny of any other relevant sources of intelligence or data for example:
- local intelligence
- CQC practice reports
- Public Health England GP practice profiles
- K041b complaints indicator set made by or on behalf of patients
- Friends and Family Test
- General Practice Patient Survey
- NHS Right Care future indicator sets for general practice
- performer performance/concerns (if appropriate)
- ICB engagement and relationship
- LMC intelligence
- practice phone call or visit
- Medicines optimisation dashboard
- GP workload tool
- GP appointments data
2.5.19 Data alone (whether derived from the above or the 3 key sources) is not however a panacea. The commissioner must consider the practice in the context of wider determining factors (eg social deprivation, health needs, population profile, resourcing, to name but a few).
2.5.20 There are numerous examples of data being used inappropriately and contrary to the purpose for which it was collected; one such non healthcare related example is provided below. The example below is intended to reinforce the concept of using data appropriately, in context and as part of a wider suite of factual intelligence to make informed decisions.
The Bhoomi Project was an ambitious effort by the southern Indian state of Karnataka to digitize some 20 million land titles, making them more accessible. It was supposed to be a shining example of governance and open data that would benefit everyone and bring new efficiencies to the world’s largest democracy. Instead, the portal proved a boon to corporations and the wealthy, who hired lawyers and predatory land agents to challenge titles, hunt for errors in documentation, exploit gaps in records, identify targets for bribery, and snap up property. An initiative that was intended to level the playing field for small landholders ended up penalising them and bribery costs and processing time actually increased.
2.5.21 Underlying this approach is the recognition that the best way of ensuring continued excellence lies in the consistent and proportionate application of an assurance framework which requires commissioners to consider multiple sources of reliable and accurate information and intelligence against relevant and specific criteria.
2.6 Practice visit – best practice
2.6.1 The commissioner remains accountable for contract management, a co-ordinated practice/commissioner/CQC/LMC relationship provides an opportunity for an engaging and collaborative discussion that covers each practice’s quality and achievement across a range of agreed standards, be that in respect of the service provided by a practice or a practices use of for example, secondary care services.
2.6.2 By way of an example and to provide clarity, a commissioner may have a conversation with a member practice, which from an initial view, appears to have a disproportionate number of emergency admissions for conditions usually managed in primary care. In itself, this may not necessarily indicate a problem but allows the commissioner to understand the implications in the wider commissioning arrangements.
2.6.3 The commissioner will not necessarily focus solely on the contractual requirements and may include quality improvement and health outcomes to ensure it is meeting its duties to improve quality and secure good public health in the population.
Understand the background
2.6.4 To align with the commitment to reduce burden and bureaucracy, commissioners should consider whether the visit can be managed remotely or whether other practice visits may be planned or recently undertaken to avoid unnecessary duplication. Such visits may be planned by CQC or NHS England in relation to regulation or educational standards.
2.6.5 Visits to practices may originate from many areas and may be formal or informal. The reasons for visiting a practice may be for:
- list closure application
- CQC report
- new contractor visits
- practice support
- investigation of concerns raised – see annex 3: a sample clinical governance and practice review
- annual review of provider
- contractual concerns, eg boundary changes
- practice mergers
- performer concerns that may be impacting on contract
Note: in addition, commissioners should still undertake a rolling programme of review as outlined at the start of this chapter, but this should include a random sample of practices not identified through other intelligence led approaches.
Gathering information
2.6.6 Before visiting the practice, collate all relevant and available data and information (examples provided below):
- CQC report if available, or discussion with CQC data and/or inspection team
- primary care web tool
- “soft” intelligence
- QOF scores
- complaints
- any local profiling tools or dashboards
- legal advice if required
- ask the practice to complete template which may save time during your visit.
- Primary Care Indicators Dashboard – see annex 1: to request access
Communications
2.6.7 Early communication is key to a successful visit. Always contact the practice to advise them that you will be visiting the practice and the reason why. The agreed date must be followed up in writing. Ensuring and confirming adherence to infection control procedures which may be in place, give plenty of notice unless there is a patient concern – see annex 2: a sample practice visit letter.
Informal visits
2.6.8 If an informal visit is planned, the practice has usually instigated it themselves and therefore are aware of the reason ie practice merger. Ensure you have the right information available for the matter to be discussed. For example, if the visit is to discuss a list closure, ensure you know the practice list size, list variations, surrounding practice closures etc.
Formal visits
2.6.9 Concerns about a practice can be raised to commissioners through various routes. Depending upon the issues raised the commissioners will need to make an informed decision on the extent to which it need to investigate.
2.6.10 Commissioners should:
- establish a task and finish group
- Establish terms of reference for task and finish group – see annex 5: sample terms of reference(ToR) for a task and finish group investigating concerns
- task and finish froup agree the actions required
- practice visit
- breach/remedial notices issued where appropriate
- contract termination
- referral to QSAG/Professional Advisory Group (PAG)
- agree clear and specific ToR for any visit, including a commitment to review/amend the ToR in light of any new/emerging evidence. Amendments should be agreed between parties
- Investigation team identified – to include, but inclusive of, GP, primary care nurse lead, safeguarding lead, nursing and quality lead, contract manager. Admin support where appropriate
- initiate formal contact with practice.
- communication with practice, with recommendation of inclusion of LMC
- practice visit with appropriate team
- report/action plan drafted – see annex 4: a sample overview of concerns – investigation plan
- report/action plan submitted to task and finish group
- report/action plan finalised
- report/action plan sent to practice for comment
- meeting with practice to discuss taking action plan forward
- monitoring meetings to ensure targets/deadlines are met
- final meeting with practice to close process
- final task and finish group to give assurance issue/concern is resolved
2.6.11 If issues are not resolved, then contract breach/termination notices may be served.
Consultation with and support from the Local Medical Committee (LMC)
2.6.12 If the commissioner is undertaking a targeted visit relating to concerns raised or known contractual underperformance, which may result in actions being imposed or considered, then it shall, whenever it is reasonably practical to do so, consult the Local Medical Committee.
2.6.13 The LMC has a role in supporting practices facing remedial, breach and termination notices or those undergoing performance investigations. The LMC can advise practices on how to complete actions required by remedial notices, how to address issues in order to avoid further contract breaches and appeal against termination notices if appropriate. The LMC can signpost practices to experts who can help, eg the practices’ Medical Defence Organisation or consultants who can advise on practical issues such as practice policies, etc. For those practices undergoing performance investigations, the LMC can support practices in preparatory meetings with the investigating officers and the commissioners, assist with drafting terms of reference, guide practices through the investigation process and sit in on interviews with clinicians and staff to ensure that due process is followed.
2.6.14 Commissioners are encouraged to advise practices in these circumstances to make contact with their LMC as early as possible to ensure they have access to expert help and advice.
3. Managing patient lists
3.1 Introduction
3.1.1 Practices operate either an open or a closed patient list. Patients have the ability to register with any local practice which operates an open list. Practices continue to have discretion over new patient registrations, although fair and reasonable grounds should be presented in the event of a refusal to accept a patient onto an open practice list.
3.1.2 Practices must ensure that they meet all general legal duties and must ensure that they are not directly or indirectly in breach of the public sector equality duty.
3.1.3 The commissioner has an obligation to prepare and keep up to date a list of patients accepted by the contractor or assigned to its list of patients and who have not been removed from that list. Primary Care Support England (PCSE) process new patient registrations and de-registrations and ensure that the national patient records database reflects what is shown in each practice’s patient list on behalf of commissioners.
3.1.4 As in 3.2 to 3.5 below, this policy sets out:
- the arrangements for managing patient assignments (part A)
- list maintenance for primary medical services including general list maintenance by PCSE (part B1) and targeted list cleansing by commissioners (part B2)
- managing closed lists (part C)
3.2 Part A: managing patient assignments
Scope
3.2.1 This part A sets out the processes the commissioner should follow in respect of patient assignment to practice lists. It also provides information regarding the grounds for practice refusal to register a new patient and potential difficulties that may arise following removal from a practice list and the procedures that must be followed in the event patient assignment to a practice list is required.
3.2.2 Where a practice list is open, a patient may apply for registration either in person or on behalf of another, whether or not they are resident in the practice area or are currently registered at another practice.
Refusing patient registration onto an open list
3.2.3 In most circumstances, practices operating an open list do so effectively, and in a reasonable manner, accepting applications for new registrations on a daily basis. There are, however, a number of circumstances when a patient may find it difficult to obtain registration with their local practice and in these circumstances, it is important that the commissioner is fully aware of the grounds under which a practice may refuse registration and the processes that must be followed in order to demonstrate that this refusal has not been on prejudicial grounds.
3.2.4 A practice may only refuse to accept a patient onto an open list where it has reasonable grounds for doing so. Reasonable grounds will not relate to the patient’s race, gender, social class, age, religion, sexual orientation, appearance, disability or medical condition. Where a practice refuses to register a patient, the reason for this refusal must be made in writing to the patient within 14 days of the request for inclusion being made. The contractor must keep a written record of applications and reasons for refusal. Reasonable grounds for refusal may include for example that the patient:
- does not live in the practice area
- is already registered with a special allocation scheme provider
3.2.5 The operation of a waiting list for registrations is not appropriate. Where a practice feels that it cannot accept new registrations at the time of the patients’ application to join the practice, they may need to consider whether the practice list should remain open and enter into discussions in this respect with the commissioner. See section C for more information.
3.2.6 In the event the commissioner is approached regarding any refusal of registration, it must contact the practice to confirm the situation and address the matter in line with the PMS regulations, GMS regulations or APMS directions (as appropriate).
Removing a patient from a practice list
3.2.7 Where a practice wishes to remove a patient from its practice list, the practice must normally provide the reason for removal in writing to the patient. Removal may normally only be requested if, within the period of 12 months prior to the date of the request, the practice has warned the patient in writing that they are at risk of removal and reasons for this have been stated.
It may be justified that a written warning was not possible/appropriate in the circumstances that:
- the reason for removal relates to a change of address outside of the practice area including where a patient has been registered as a temporary resident elsewhere and has exceeded the three-month temporary residency period
- the practice has reasonable grounds for believing that the issue of a warning would be harmful to the physical or mental health of the patient or put at risk one or more members of the practice team; or
- it is, in the opinion of the contractor, not otherwise reasonable or practical for a warning to be given. The practice must record in writing either the date of any warning given and the reasons for such a warning or the reason why no such warning was given
3.2.8 All patient removals must be recorded by the practice, including the reasons and circumstances of the removal and this record must be made available to the commissioner should it be requested.
3.2.9 Notifications by the contractor to the commissioner (via PCSE) should be made on removals from the contractors’ patient list. The commissioner must refer to the relevant regulations/directions (set out in schedule 3 part 3 of the GMS regulations; schedule 2 part 3 of the PMS regulations; the APMS direction do not require APMS contracts to have provisions relating to patient lists – the commissioner should refer to the wording of the relevant APMS contract).
3.2.10 Practices may remove a patient with immediate effect where the patient has committed an act of violence or behaved in such a way that the contractor, practice staff, other patients, or those present at the place the services were provided have feared for their safety. The incident leading to the request for immediate removal must have been reported to the police. It is highly likely that there are different ways in which violent patients are managed nationally as services were commissioned in different ways under a violent patient directed enhanced service scheme. For this reason, the commissioner must refer to the relevant regulations/directions and the special allocation scheme chapter.
3.2.11 Patients may experience difficulties in registering where they have been removed from a practice list, although, (other than on the grounds of violence or threatening behaviour), this should not ordinarily be a factor considered by practices when approached by new patients. It should also be noted that patients have the right to choose to move from one practice to another, even within the same locality, without providing grounds for doing so.
3.2.12 In any type of patient deduction, consideration must be given to any potential safeguarding concerns. Where a patient is at risk of being removed for example for missed appointments, that may reflect on parenting/caring capacity (eg mental health) and consideration must be given to safeguarding either for children or vulnerable/at risk adults. Advice should always be sought from local safeguarding leads and/or the commissioners’ designated professional.
3.2.13 With regard to the deduction of children (aged under 18) GP practices have the clinical expedient prerogative to retain children (under 18 years old) under the paramountcy of the child within The Children and Families Act 2014, until such time that they understand how the children might be cared for by another NHS or private GP, especially if vaccines or screening are still indicated.
3.2.14 It should also be noted that:
Children and young people (CYP) on a protection order or protection plan should not be de-registered on the grounds of behaviour including non-attendance.
CYP (not protected) and adults with a learning disability and/or autism, individuals with a mental health issue or with those with formal carer should not be de-registered on the grounds of behaviour including non-attendance.
3.2.15 These citizens may need to be referred to safeguarding leads since they might be at risk either through behavioural problems or non-attendance of their appointments.
3.2.16 These citizens should be allowed to sustain their GP registration for continuity of care until such times as it can be established how the children might be cared for by another NHS or private GP.
Therefore:
- Children of parents or carers, who have been removed from the list for any reason, must not be left without access to primary care service.
- Where parents or carers have been removed from the list due to aggressive and or violent behaviour a risk assessment should be completed to identify any risk to their children and the appropriate safeguarding referrals made.
Where patient assignment to a practice list is required
Assignment to an open list
3.2.17 The commissioner may assign a new patient to a practice whose list of patients is open and in making the assignment, the commissioner shall have regard to:
- the wishes and circumstances of the patient to be assigned
- the distance between the patient’s place of residence and the practice premises
- whether, during the 6 months ending on the date on which the application for assignment is received by the commissioner, the patient’s name has been removed from the list of patients of any practice in the area of the commissioner, at the request of the practice
- whether the patient’s name has previously been removed from the list of patients of any practice in the area of the commissioner owing to violent behaviour and, if so, whether the practice to which the patient is to be assigned has appropriate facilities to deal with such a patient
- other matters the commissioner considers relevant
3.2.18 A new patient is defined as a person who:
- has been refused inclusion in a contractor’s list of patients or has not been accepted as a temporary resident by a contractor, and
- would like to be included in the list of patients of a contractor in whose outer boundary area (as specified in accordance with regulation 20(1)(d)) that person
3.2.19 In making an assignment, the commissioner will contact the practice by telephone, to which the patient is to be assigned, to inform them that an assignment is being made. Following this telephone contact, the commissioner will send an assignment notification (example at annex 1) to both the receiving practice and PCSE for their information. A letter (annex 2) will also be sent to the patient informing them of their registration and provide details as to how they may access the service. In the majority of cases this letter will be issued by PCSE; however, the commissioner should ensure that this process is satisfied either through this mechanism or through its own local arrangements.
- PCSE are responsible for sending the standard patient letter in the case of allocations to open lists.
Annex 1: example assignment notification
Annex 2: example patient letter confirming registration
Assignment to a closed list
3.2.20 The commissioner may not assign a new patient to a practice that has closed its list of patients except in the following circumstances:
- most or all of the providers of essential services (or their equivalent) whose practice premises are within the commissioner’s area have closed their lists of patients
- the assessment panel (as detailed below) has determined that patients may be assigned to the practice in question, and that determination has not been overturned either by a determination of the Secretary of State or (where applicable) by a court
- the commissioner has entered discussions with the practice in question regarding the assignment of a patient, whereby additional support that the commissioner can offer to the practice may be required. The commissioner shall use its best endeavours to provide appropriate support and should discuss support in respect of the first assignment of a patient and any subsequent assignments made to that contractor during their list closure
- PCSE are responsible for sending the standard patient letter in the case of allocations to closed lists
Assignment based on the determination of a commissioner assessment panel
3.2.21 Where the commissioner has the need to assign a patient to a practice that has a closed list and most or all of the providers of essential services (or their equivalent) whose practice premises are within the locality of the commissioner have closed their lists of patients, the commissioner must:
- prepare a proposal to be considered by the assessment panel which must include details of those practices to which the commissioner wishes to assign patients
- ensure that the assessment panel is appointed to consider and determine its proposal and the members of the assessment panel must include:
- a commissioner director/officer
- a patient representative who is a member of the local health and wellbeing board (HWB) or local healthwatch organisation
- a member of a LMC but not a member of the LMC formed for the area in which the contractors who may be assigned patients as a consequence of the panel’s determination provide services
- notify in writing that it has referred the matter of patient assignment to the assessment panel to the following:
- the relevant LMC for the contractors in the area of the commissioner
- any contractors whose practice premises are within the commissioner’s jurisdiction that have closed their list of patients and may, in the opinion of the commissioner be affected by the determination of the assessment panel
3.2.22 In reaching its determination, the assessment panel shall have regard to relevant factors including:
- whether the commissioner has attempted to secure the provision of essential services (or their equivalent) for new patients other than by means of their assignment to contractors with closed lists of patients
- the workload of those contractors likely to be affected by any decision to assign such patients to their list of patients
3.2.23 The assessment panel shall reach a determination within the period of 28 days beginning with the date on which the panel was appointed.
3.2.24 The assessment panel shall determine whether the commissioner may assign patients to practices which have closed their lists of patients. If it determines that the commissioner may make such assignments, it shall also determine those practices to which patients may be assigned.
3.2.25 The assessment panel may determine that the commissioner may assign patients to practices other than those practices specified by the commissioner in its proposal, as long as the practices were notified during the preparation stages of the assessment panel being held.
The assessment panel’s determination must include the factors considered by the panel and be made in writing to:
- the LMC for the contractor(s) in area of the commissioner for whom the determination relates
- any contractors whose practice premises are within the commissioner’s jurisdiction that have closed their list of patients and may, in the opinion of the commissioner be affected by the determination of the assessment panel
NHS dispute resolution procedure relating to determinations of the Commissioner Assessment Panel
3.2.26 Where an assessment panel determines that the commissioner may assign new patients to contractors which have closed their lists of patients, any contractor specified in that determination may refer the matter to the Secretary of State to review the determination of the assessment panel. Please refer to the chapter on managing disputes.
Removal by a contractor of patients assigned to the practice
3.2.27 Historically, practices have often applied an unwritten agreement to the retention period of assigned patients. However, there are no formal arrangements in respect of timescales for patient retention in these circumstances. While the significant majority of practices continue to manage assigned patients in the same manner as an ordinarily registered patient, others may commence a formal removal process immediately following assignment. The commissioner has a responsibility to ensure that all requests to remove a patient at the request of the contractor must be managed in line with the relevant regulations/directions.
3.3 Part B1: general list maintenance for primary medical services
Scope
3.3.1 This part B sets out the processes for the commissioner to ensure list maintenance is appropriately managed. It details the list maintenance and data quality measures to be undertaken and suggests additional measures to be taken. Where references are made to actions to be followed by the commissioner, these actions should, where possible, be done together with the available support services or payment authority.
3.3.2 Medical service contracts are predominantly funded on a capitation basis. It follows, therefore, that if a patient list is overstated, the contractor will receive more funding than it is entitled to and this presents a significant financial burden on NHS resources.
3.3.3 While in most cases, contractors endeavour to maintain their registered lists in a current and accurate state, patients often fail to notify their registered practice when leaving the area and/or country resulting in potential duplicate registrations, ghost and gone away patients remaining registered on the national patient registration systems.
3.3.4 Some degree of list inflation is inevitable, but manageable if kept within reasonable bounds. Current trends of inflation are excessive and, in some regions, continue to rise. The commissioner and PCSE are expected to engage in regular proactive list maintenance with general practices.
3.3.5 Ongoing and effective maintenance of lists is essential to ensure they are accurate. However, even with the most effective list maintenance procedures in place, a practice list can hold 3% to 8% of inaccuracy due to patient turnover alone.
3.3.6 Practices with robust systems in place to verify and record patient details at the point of registration, as well as regular systematic checking of details when patients contact the practice, have more accurate lists.
3.3.7 The accuracy of a practice’s registration list is important for:
- the efficacy of ill-health prevention/screening programmes and total population capture
- the assessment of performance and clinical outcomes which are often compared on a ‘per patients’ denominator
- the appropriate use of public funds, as allocations are made on a £ per patient basis
Operating principles
3.3.8 List maintenance processes should be designed with the proactive engagement of the commissioner, patients (or their representatives), PCSE, and LMCs on behalf of GPs and practice managers. This should be through a continuous rolling programme, for example: working through the practice registers alphabetically over a 1 to 3-year period, or by targeting specific patient cohorts, for example, choosing a cohort that supports a screening programme, eg childhood immunisations, flu or cytology.
3.3.9 A ‘one-hit’ approach in which a single practice is targeted should be avoided except in exceptional circumstances. This might include due diligence when transferring a full list to a new contract, for example. In all cases this should be carried out in discussion with the LMC.
3.3.10 Contractors have a crucial role to play in ensuring their staff access relevant training, are familiar with the FP69 process and are proactive partners in the list maintenance process, responding to requests from PCSE.
3.3.11 When responding to an active FP69 (see annex 1 and annex 2) a practice declaration will be sufficient. The practice is responsible for ensuring all declarations made are accurate and should be made aware that these can be challenged where any inconsistencies are highlighted through a cluster-wide audit.
3.3.12 A list maintenance exercise is not designed to address performance failures. Where there are reasonable grounds for believing that list inflation is particularly high at an individual practice then concerns about this should be handled separately and in accordance with the performance management directions.
3.3.13 The commissioner should ensure that where the PCSE disputes the practice declaration, the practice is told why and is advised of any list actions that have been taken.
Minimising inconvenience to patients
3.3.14 Advance screening of the proposed cohort by practices means that fewer patients will be inconvenienced by having to respond to a letter. It will also reduce administrative costs and wasted resource associated with the exercise.
3.3.15 The commissioner should maximise awareness in the patient population of list maintenance procedures by ensuring that an effective patient communication strategy is in place. The strategy should be tailored to local needs and build upon examples of what has worked well. For example:
- Letters to be addressed to named patients and not the occupier – see annex 3: sample letter to patients.
- Branded NHS envelopes with a return address are more likely to be opened as they are clearly directly in relation to the patients’ health – see annex 4: standard envelope content.
- Contractor teams alerting patients to registration checks well in advance – as part of the registration conversation, through display notices in a practice.
- The commissioner and contractors making the process clear to patients through any letters and posters, for example – what the letter looks like, what to do when you get one, the steps in place to minimise deregistration errors, what to do if there is a de-registration error, what to do if a letter arrives for someone not living at that address.
- Communications must take into account the Accessible Information Standard which requires organisations to ensure that disabled patients receive information in formats that they can understand. For more information on the standard and guidance on its implementation, see the NHS England website.
- Communications must be tailored for different languages and consideration of other support for patients whose first language is not English.
3.3.16 List maintenance is also an opportunity to improve other aspects of patients’ registration including the accuracy of patient information held. The commissioner should ensure that contractors verify the details held on the practice system systematically as part of routine on-going maintenance.
Patient registration process
3.3.17 Appropriate and timely management of the patient registration process is essential in minimising the potential for list inflation.
3.3.18 The standard registration process requires all general practices to notify all registrations to the national primary care registration system (currently referred to as the National Health Application and Infrastructure Service (NHAIS) but to be replaced by a new Primary Care Registration Management (PCRM) system later in 2022. The NHAIS/PCRM user should then confirm the registration to the practice and take steps to arrange via PCSE for the transfer of medical records from the patient’s previous general practice. Electronic links are in place between NHAIS sites/PCRM and all general practices that enable this process.
3.3.19 GP practices are required to monitor that all their registrations and patient deductions are acknowledged by NHAIS/PCRM. This ensures that patients are correctly registered and will be included in NHS screening and immunisation programmes.
3.3.20 Practices should also check their list size of registered patients on a quarterly basis against the GP Payments and Pensions System by logging into PCSE online. This ensures that payments to the practice remain accurate and any issues with the registration process are identified.
3.3.21 The process of confirming the new patient registration by NHAIS/PCRM involves checking the patient details against the Personal Demographics Service (PDS) National Back Office (NBO) to confirm the patient’s NHS number, where NHS numbers cannot be traced, the system provides for the user to request the allocation of a new NHS number.
3.3.22 Where it is not possible to trace an NHS number for a patient, rather than request allocation of a new NHS number the registration should be kept pending and the previous general practice contacted to obtain further details.
3.3.23 If the practice cannot provide further information to enable the NHS number to be traced it should be asked to contact the patient to obtain this. By taking these steps, the user will ensure that allocation of new NHS numbers is kept to a minimum and therefore minimises the potential for list inflation.
3.3.24 Where a new NHS number has been allocated then additional checks are undertaken by the PDS NBO to help ensure a duplicate NHS number has not been created for a patient. Monthly reports, identifying the number of duplicate NHS numbers allocated by PCSE are produced by NHS England and these are split between those where the service provider should have been able to trace the correct number and those duplicates that are considered unavoidable.
3.3.25 It is essential that robust procedures are in place to prevent the creation of duplicate registrations at the time of registration. The figures available on the volumes of duplicate numbers created by each service provider should provide valuable benchmark data to monitor this.
3.3.26 The commissioner should ensure that the PCSE is processing routine registrations in a timely manner as this is also key to ensuring accuracy of practice lists.
Elements of a rolling list maintenance programme
3.3.27 Routine business processes that involve sending letters to patients help reduce list inflation, as any letters returned undelivered by Royal Mail result in general practices being given the statutory 6-month notice period to provide confirmation that the person is a patient to whom it is still responsible for providing essential services [The FP69 flag in these circumstances will affect a breast screening invitation]. Where confirmation is not provided then the patient is removed from the practice list. The only exception to this is patients aged under 18 who will remain registered under the paramountcy principle of protection (please also refer to the patient registration chapter for further information).
3.3.28 These letters to patients, using data sourced from the NHAIS/PCRM system, are inclusive of, but not limited to, the following:
- cervical screening invitation letters sent to all women aged 25-64
- cervical screening test results sent to all women attending for a test as part of the NHS Cervical Screening Programme
- flu vaccination invitation letters sent to patients aged 65 and over together with any patients identified by general practices as being in an ‘at risk’ group
- chlamydia screening invitations letters sent to patients on behalf of certain local authorities
- bowel screening invitation letters are sent to all patients aged 60 and 74 where the source data used to identify patients to be invited is taken from the NHAIS system
- letters sent to all patients registered with a specific general practice if there are any significant changes to practice arrangements
- medical cards or letters of confirmation of NHS number and registration
- verification by general practices of the vaccination status of all children aged 2 years and 5 years registered with the practice on the first day of each quarter
3.3.29 In maintaining the NHAIS/PCRM system, specific tasks need to be undertaken to reduce list inflation and help maintain the accuracy of practice lists. The annual programme of checks to be undertaken is shown below together with the standard procedure which should be adopted for each. NHS England may agree with PCSE to pause these checks in exceptional circumstances. The flow chart illustrated within annex 1 and annex 2 indicates the standard process to be followed.
Multiple occupancy (MO)
Frequency: after the initial month, PCSE will check the additional patients who appeared at MO addresses and reset.
Process: PCSE must:
- compare Office of National Statistics (ONS) and NHAIS/PCRM population figures at ward/super output area (SOA) level to enable prioritisation of work
- send the list of names to the relevant general practices. Each practice should confirm if patients have been seen in the last 15 months
- send letters to any patients that are recorded as being registered and have not been seen by their general practice in the past 15 months, taking into account the requirement to ensure that disabled patients receive information in a format that they can understand, and they receive support to help them communicate (as mandated in the Accessible Information Standard)
- send reminder letters if no reply received after four weeks
- activate an FP69 for the practices if any letters return undelivered or where no response is received within 2 months of the date of the original letter being sent
- remove the patient from the list if the general practice does not confirm patient contact within 6 months
University/college student/residential school
Frequency: annually October to December
Process: PCSE must:
- identify patients recorded on NHAIS/PCRM as being registered with a general practice for 4 or more years in respect of a college/university address
- send the lists of names to the relevant general practices asking them to confirm the patients are still registered and are still attending the surgery for treatment. Any patients found to be no longer resident should be removed from the practice lists
- send letters to patients asking them to confirm their address where practices are unable to confirm registration, taking into account the requirement to ensure that disabled patients receive information in a format that they can understand, and they receive support to help them communicate (as mandated in the Accessible Information Standard)
- send reminder letters if no reply received after 4 weeks
- activate an FP69 for the practices if any letters return undelivered or where no response is received within 2 months of the date of the original letter being sent
- remove patients from the list in any cases where the general practice does not confirm the address within 6 months
Patients aged 100 and over
Frequency: six monthly March and September checks
Process: PCSE must:
- check on NHAIS/PCRM for any patients aged over 100 years
- contact general practice to confirm patient still registered
- remove any patients no longer registered from practice lists
Transient checks
Frequency: Monthly
Process: PCSE must:
- send a letter to patients 12 months after their date of registration with a general practice, where at the time of registration they were recorded as having recently arrived from abroad, to ask the patient to confirm their current address. This sentence should be in several different languages depending on the reasonable needs of the practice’s patient, and should take into account the requirement to ensure that disabled patients receive information in a format that they can understand, and they receive support to help them communicate (as mandated in the Accessible Information Standard)
- send reminder letters if no reply received after 4 weeks
- if any letters are returned undelivered or where no response is received, remove patients from the list in any cases where the general practice does not confirm the address within 6 months
Notification of demolished addresses [the FP69 flag in these circumstances will affect a breast screening invitation]
Frequency: quarterly
Process:
- NHAIS/PCRM receive regular updates to the PAF information to enable the accurate maintenance of patient addresses. Included in the updates are notifications of properties which have been demolished
- PCSE should ensure that the correct address of patients registered regarding any of these addresses is checked with the registered general practices
Patients not seen by general practice in previous 5 years
Frequency: annually
Process: PCSE should:
- contact general practices to obtain a list of all those patients that have not had a consultation within the last 5 years
- send a letter to all those identified patients to confirm address and registration, taking into account the requirement to ensure that disabled patients receive information in a format that they can understand, and they receive support to help them communicate (as mandated in the Accessible Information Standard)
- send reminder letters if no reply is received after 4 weeks
- activate an FP69 for the practices if any letters return undelivered or where no response is received within 2 months of the date of the original letter being sent
- remove patients from the list in any cases where the general practice does not confirm the address within 6 months
Additional measures (see also part B2 below)
3.3.30 Despite initiating a rolling programme of list maintenance measures, figures comparing ONS mid-year populations with NHAIS/PCRM registered population may still show significant inflation. These inflation rates may also differ significantly for local areas.
3.3.31 If the commissioner has a particularly large variance it may wish to undertake a targeted campaign to reduce this in one large exercise. If so, the commissioner is strongly urged to engage their general practices and the relevant LMCs.
3.3.32 Suggested work that could be undertaken is:
- Comparison of ONS mid-year stats with NHAIS/PCRM figures at middle SOA level. This will identify localities within each area where inflation rates are highest and will therefore highlight specific areas to be targeted.
- Send mailshot to confirm residency to male patients aged 18-44 living in areas where inflation rates are highest. ONS and NHAIS/PCRM comparison at area level has previously shown that the highest inflation rates are related to male patients in this age group, possibly because there are no routine mailshots sent to this cohort.
- Undertake further immigrant checks 3 years after the date of first registration for persons who immediately before their current registration are recorded as having arrived from abroad.
- Issue guidance and clarification for general practices on the FP69 procedure. Greater awareness of the processes for removing patients within general practices could reduce the scale of list inflation. If guidance has not previously been given to practices on the FP69 process, then this should be undertaken. Once in place, this could become part of a standard rolling programme.
- Test the effectiveness of undertaking checks for duplicate registrations between NHAIS/PCRM systems. A check between several systems will confirm whether this type of check would identify duplicate registrations and if so, could be developed as a standard procedure to be carried out at agreed intervals.
3.3.33 It is essential that work is carried out to reduce list inflation and verify practice lists, but it is also important to recognise the resource implications of undertaking this work. It is equally essential that all work carried out is recorded and the outcomes monitored to evaluate the success of each initiative.
3.3.34 The commissioner should ensure that PCSE submits a monthly return to the commissioner detailing the work undertaken and the outcome. Pro forma is attached in annex 5 to be used to submit the monthly returns. To streamline this process, standard reports available from the NHAIS/PCRM could be used to populate this pro forma.
3.3.35 Given the requirement to allow a practice 6 months to confirm the address before patients can be removed from the practice list, it is recognised that any list maintenance exercise could take 6 to 9 months before benefits are realised. This needs to be considered when assessing the effectiveness of interventions.
3.4 Part B2: targeted list maintenance for primary medical services
Background
3.4.1 The Office for National Statistics regularly publishes mid-year population estimates (ONS CCG mid-year population estimates) middle super output area (ONS MSOA populations) and lower super output area (ONS LSOA populations). Using these population estimates alongside the numbers of patients registered at a GP practice (NHS England published GP registered populations) and other sources of local intelligence such as patient postcode list, can assist in determining at a local level, whether the difference could warrant further investigation.
Scope
3.4.2 Part B2 sets out some considerations and investigations that could be undertaken to determine whether a targeted list validation exercise may be beneficial within the commissioning area and what that could involve.
3.4.3 A key line of enquiry in national counter fraud exercises, often relates to list maintenance and so GP practices may welcome support in proactively reviewing their registered list.
Available data sources
3.4.4 Of the data sources listed below, not all will be available to all organisations (eg patient level data cannot be held by NHS England).
Data providers
3.4.5 NHS England
- number of patients registered at a GP practice
- number of patients registered at a GP practice (PCN/ICB level)
- number of patients registered at a GP practice (NHS england commissioning region)
- number of patients registered at a GP practice mapped to LSOA
- from April 2017, NHS England began publishing these data monthly, prior to this the publication were quarterly on the first day of April, July, October and January
- each of these data is available in both 5 year age groups and single year of age (by male, female and total). Files are available to download for onward analysis, but NHS England also provides an interactive platform called the General Practice Data Hub
3.4.6 Office for National Statistics
- mid-year population estimates
- middle super output area mid-year population estimates
- lower super output area mid-year population estimates
- the Office for National Statistics publish these data annually, usually at the end of October each year, for the previous year
3.4.7 Data.gov.uk
- postcode to output area to lower layer super output area to middle layer super output area to local authority district lookups for in England and Wales
What to consider, who and why?
3.4.8 Where a GP practice list contains records of people who should no longer be on the list this is known as list inflation. There can be many reasons for this and commissioners and GP practices can work together to minimise this through list maintenance.
3.4.9 In some GP practices there can often be high turnover (leaving and joining) of patients, which can be challenging to monitor but benefits from timely processing.
3.4.10 There are records that link to patients who do not de-register and there are 2 principal reasons why an individual may not de-register.
3.4.11 Some people may be slow to re-register at other GP practices, despite having moved away from the area, as they are relatively healthy and do not see re-registration as a priority.
3.4.12 People who live abroad (who are required to de-register from their GP practice) fail to do so either because they do not see it as a priority when moving abroad or because they wish to have continued access to the NHS (often referred to as “ghost patients” (this affects list inflation at both the local and national level).
3.4.13 ONS suggests that, typically the following groups tend to be quicker to register a change of address:
- mothers with young children
- those with ongoing health conditions
- the very elderly
3.4.14 Additionally, the following tend to be slower to register a change of address:
- young healthy adults, especially males – including students
- highly mobile individuals
- healthier persons, especially males
- males – in general
3.4.15 Parental home: mobile young adults may choose or default to remaining registered at their parental address; this is similar to the lags issue above.
3.4.16 Shared custody: there is potential for a range of issues where there is shared custody of children at different addresses. These can potentially include:
- split residence not reflected in the record
- duplicate registrations
- use of different names (particularly surnames)
3.4.17 Care homes (and similar institutions): Where a patient moves into a care home this may not be recorded as a change in address, particularly if the intended stay is short. These stays may become longer so that there has in effect been a change in residence, although the GP register has not been updated. By contrast a move may be intended as long-term (and the move recorded on the Patient Register) but the patient may die soon after the move.
3.4.18 Please note, a change of address should also not be considered where a patient attends a special residential school, boarding school, children’s homes, or other residential facility, unless this is a secure or specialist hospital setting or immigration centre.
3.4.19 There are 2 potential consequences for statistical use of data:
- a spell of residence away from the home address can be missed
- a death can be recorded with a place of residence given as different from that recorded on the Patient Register
3.4.20 Duplicate records: there are a number of occasions where duplicate records can occur. These can be classified as duplicates with the same NHS number, and duplicates with a different NHS number. Duplicate records with the same number could be:
- records for the same person, with the same number, held on 2 different lists – the Audit Commission said that the majority of these were temporary where a patient was in the process of transferring from one practice to another
- records for 2 different people with the same number – the Audit Commission said that these were rare and the cause was not known; potential reasons could include error by the patient in writing an NHS number (and where a check is not undertaken or is passed by chance – for example, the same date of birth), clerical (typing or legibility) error on NHS number input, mismatching a patient to another with similar details on registration and allocating the wrong number or fraud. (anecdotally there have been reports of people ‘sharing’ NHS numbers in certain communities)
3.4.21 Duplicates with different numbers could be because:
- on registration with a GP, a patient is incorrectly identified as a new entrant to the NHS (returning emigrant, exit from armed forces, return from private practice)
- on registration with a GP, no match is traced to previous records
- on registration with a GP, a patient gives insufficient details to allow a match (as above, patients do not legally have to provide proof of identity)
3.4.22 Snapshot: the data that we currently use from the Patient Register is based on a (typically annual) snapshot. This gives the position at that point in time, as it occurs on the register. This approach means there is no “history” between snapshots of changes. For example, where there are 2 or more changes of address in a year only the first and last of these addresses are captured (implying a single move). Moves before exiting from the system (including emigration and death) can also be missed, as can moves shortly after entry to the system (including immigration and birth).
3.4.23 Coverage: the Patient Register is a broad coverage source, but some groups are not included (under-coverage of the total population) and there are also some over-coverage issues. Evidence from ONS shows that over-coverage tends to be the larger issue, with the Patient Register having 4.3% more people registered than the 2011 Census estimate of population, whilst we are aware in NHS England the range can be 3% to 8%.
3.4.24 The following groups are not included in GP Practice Register, and may be the cause of statistical under-coverage:
- patients solely registered with private GPs
- babies that have yet to be registered at a GP practice
- migrants into the UK who have yet to register
- armed forces (though some remain on GP lists)
- some armed forces dependants
- prisoners (other than those with a sentence under 6 months)
- some prisoners with a short sentence who have received medical assistance in prison
- patients who have been removed through ‘no contact’ measures
- patients with a temporary NHS number, where no ‘permanent number exists or where their permanent number is not on a GP register
3.4.25 The following groups, for some statistical purposes, may be thought of as over-coverage:
- patients who are no longer resident in the UK (emigrants)
- patients who are staying in the UK for only a short period
- duplicate records
What local checks could be undertaken
3.4.26 Utilising the data sources and data listed section above and the intelligence from ONS in section, commissioners can determine where they may wish to focus attention and or support for the practice. Decisions should be made locally, and on a case-by-case basis. Commissioners may wish to undertake analysis internally, or work with a partner such as a commissioning support unit (CSU) who would work with their Data Services for Commissioners Regional Offices (DSCRO) should they wish to interrogate record level data that has been appropriately processed.
3.4.27 Comparing data sources and geographies
3.4.28 Trends in ICB resident population estimates compared to trends in GP registered populations.
3.4.29 Are the proportions similar?
3.4.30 Are all the GP practices within the ICB areas increasing/decreasing with similar proportions?
3.4.31 Are there any practices significantly variant in comparison to other practices and the ICB trend?
3.4.32 Have there been any practice mergers or closures resulting in list dispersal?
3.4.33 Have there been any new and large-scale property developments recently?
3.4.34 Trends in LSOA population (ONS estimates) compared to trends in GP registered populations (LSOA data from NHS England).
3.4.35 Are the proportions similar?
- Which LSOAs fall within the practice boundary? (this may require the support of a 3rd party. Can you map record level patient data to determine in which LSOAs the practice has the majority of its patients.
3.4.36 Are the LSOA populations (resident and registered) mapped to GP practices, increasing/decreasing in broadly the same proportions as the GP practice as a whole?
3.4.37 How do they compare to other neighbouring practices?
3.4.38 Have there been any practice mergers, or closures resulting in list dispersal?
3.4.39 Have there been any new and large-scale property developments recently?
3.4.40 Is there any in-depth work that could be undertaking by working with a partner (CSU) and record level record data?
3.4.41 These considerations provide a sample of checks that could be embarked on when undertaking a targeted list maintenance exercise.
3.5 Part C: managing closed patient lists
Scope
3.5.1 This part C sets out the processes to be implemented when managing applications to close patient lists and to extend a closure period.
3.5.2 At all stages throughout these processes, it is essential that the commissioner works with the contractor and the relevant LMC to ensure clear and transparent decision making and that all decisions are made in line with internal governance arrangements.
Applications to close a patient list
3.5.3 Sometimes a contractor may wish to close its list to new registrations, eg where there are internal capacity issues or premises refurbishments. The contractor must seek approval from the commissioner by a written application (the “application”) before this may happen. A template application for the contractor to complete is attached in annex 1. The contractor should use the template application to ensure it completes all the required information. The contractor may obtain the application itself (for example by accessing this policy) or it may be requested by the contractor. An example covering letter from the commissioner to the contractor enclosing an application form is in annex 2.
3.5.4 The commissioner must acknowledge receipt of the application within 7 days of its receipt and may request further information from the contractor to enable it to consider the application thoroughly.
3.5.5 With a view to possibly enabling the contractor to keep its list of patients open, the commissioner and the contractor must talk openly to establish:
- what support the commissioner may give the contractor
- changes the commissioner or contractor may make
3.5.6 The contractor or the commissioner may at any time throughout these discussions invite the appropriate LMC to be included in the dialogue about the application.
3.5.7 The commissioner should ensure compliance with the general duties of NHS England. Please refer to the chapter on general duties of NHS England for further information. The commissioner may consult affected parties – example letter provided at annex 3.
3.5.8 The contractor may withdraw the application at any time before the commissioner makes its decision on the proposed list closure.
3.5.9 The commissioner must determine, within a period of 21 days starting on the date of receipt of the application (or within a longer period as the parties may agree):
- to approve the application and determine the date the closure is to take effect and the date the list of patients is to reopen
- to reject the application
3.5.10 The commissioner must notify the contractor of its decision in writing as soon as possible after the 21 day period.
Approval of patient list closure: closure notice
3.5.11 Where the commissioner has granted approval for closure of the patient list, a closure notice must be issued to the contractor as soon as possible after the decision is reached, with a copy to the LMC for its area (if any) and to any person consulted in the decision-making process. The commissioner should use the template notice in annex 4 to ensure it responds to the contractor with all the required information.
3.5.12 The contractor must close the list on the date in the notice and the list should remain closed for the time specified unless the commissioner and the contractor agree that the list should be re-opened to patients before the expiry of the closure period.
Rejection of application for list closure
3.5.13 When the commissioner decides to reject an application to close a list of patients, it must as soon as possible:
- provide the contractor with a notification including the reasons why the application was rejected. The commissioner should use the template in annex 5 to ensure it responds to the contractor with all the required information; and
- at the same time, send a copy of the notification to any affected LMC for its area and to any person it consulted in the decision-making process
3.5.14 When the commissioner decides to reject a contractor’s application to close its list of patients, the contractor must not make a further application until:
- the end of the 3-month period, starting on the date of the decision of the commissioner to reject; or
- the end of the 3 months, starting on the date of the final determination regarding a dispute arising from the decision to reject the application made pursuant to the NHS dispute resolution procedure (or any court proceedings) (please refer to the chapter on managing disputes for further information on the NHS dispute resolution procedure), whichever is the later
3.5.15 A contractor may make a further application to close its list of patients where there has been a change in the circumstances of the contractor which affects its ability to deliver services under the contract.
Application to extend a closure period
3.5.16 A contractor wishing to extend an agreed closure period must apply to the commissioner no less than 8 weeks before the closure period is due to end.
3.5.17 A template for completion by the contractor is attached in annex 6. An example covering letter from the commissioner to the contractor enclosing an application form is in annex 7.
3.5.18 The commissioner must acknowledge receipt of the application within 7 days, then if necessary, discuss potential support that could be offered to the contractor, discuss with any affected LMC and consult other affected parties before reaching a decision on the application to extend within 14 days from receipt of the application. The commissioner should use the template consultation letter in annex 8.
3.5.19 If the decision is to accept the application the commissioner must issue an extended closure notice as soon as possible after the decision is reached to the contractor, with a copy to the LMC for its area (if any) and to any person it consulted in the decision-making process. The commissioner should use the template in annex 9 to ensure that the contractor receives all the relevant information.
3.5.20 If the decision is to reject the application, then the commissioner must provide the contractor with a notification, including the reasons for the rejection of the application, with a copy to the LMC for its area (if any) and to any person it consulted in the decision-making process. The commissioner should use the template in annex 10.
3.5.21 The contractor may re-open its list of patients before the closure period expires if commissioner and contractor agree.
3.5.22 Where an application for the extension of the closure period has been made in accordance with this policy, and that application has been rejected, the list of patients will remain closed until such time as any dispute arising from the application has been resolved through the NHS dispute resolution procedure (or any court proceedings) or until such time as the expiry of the original closure notice. Please refer to the chapter on managing disputes for further information on the NHS dispute resolution procedure.
4 GP patient registration standard operating principles for primary medical services
4.1 Policy statement
4.1.1 There has not been any change in national policy in respect of patient registration for primary medical services – this guidance clarifies the rights of patients and the responsibilities of providers in registering with a GP practice in particular issues in relation to:
- who can access free healthcare
- the provision of documentary evidence of identity or residence on registration (in particular affecting migrants, refugees and asylum seekers (including ‘failed’ asylum seeks) who may not have ID or documents such as household bills)
- the rights of patients who are temporarily resident in a specialist hospital away from their home address and access to their ‘usual’ GP practice
4.2 Aims
4.2.1 In issuing these patient registration operating principles we aim to:
- clarify the contractual rules in respect of patient registration for patients, practices and commissioners
- reduce the risk of worsening health inequalities for specific populations (eg asylum seekers or homeless people)
- simplify and standardise the patient registration process for patients and practices
- embed best practice approaches for patient registration
- ensure fairness, equity and transparency in the way general practice services are delivered across England
4.3 Context
4.3.1 The Health and Social Care Act 2012 places an obligation on NHS England to secure the provision of primary medical services for patients throughout England. In addition, the Health and Social Care Act 2012 introduced statutory duties on the NHS to “have regard to the need to reduce inequalities” in access to and outcomes achieved by services.
4.3.2 There are further duties imposed on NHS England under the Equality Act 2010 and NHS Act 2006 on equality and health inequalities.
4.3.3 NHS England wishes to establish operating principles for GP practices for patient registration that promote equality, human rights and public health and reduce health inequalities.
4.3.4 In addition, Care Quality Commission (CQC) guidance: GP myth buster 29; looking after homeless patients in general practice can be found on the CQC’s website as can GP myth buster 36: registration and treatment of asylum seekers, refugees and other migrants.
4.3.5 In 2014 homeless and health research provided by Homeless Link reported that 90% of the homeless people they surveyed were registered with a GP. However, many responded that they were not receiving the help they needed for their health problems, and 7% had been refused access to a GP or dentist in the previous 12 months. In some cases, these refusals were due to having missed a previous appointment or because of behaviour. Others reported that they were refused access if they did not have identification or proof of address.
4.3.6 Also the General Practitioners Committee (GPC) of the British Medical Association (BMA) has related guidance which can be found can be found on the BMA’s website.
4.4 Who can register for free primary care services?
4.4.1 A patient does not need to be ‘ordinarily resident’ in the country to be eligible for NHS primary medical services – this only applies to secondary (hospital) care. In effect, therefore, anybody in England may register and consult with a GP without charge.
4.4.2 Where a GP refers a patient for secondary services (hospital or other community services) they should do so on clinical grounds alone; eligibility for free care will be assessed by the receiving organisation.
4.4.3 The absence of any reciprocal arrangements between the nation-states, a patient’s nationality is therefore not relevant in giving people entitlement to register as NHS patients for primary medical services.
4.4.4 In October 2017, contractual requirements were introduced to help identify patients with a non-UK issued EHIC or S1 form or who may be subject to the NHS (charges to overseas visitors) regulations 2015.
4.4.5 For those patients who self-declare at the point of registration that they hold either a non-UK issued EHIC or a S1 form, the practice will be required to manually record that the patient holds either a non-UK issued EHIC or a S1 form in the patient’s medical record and then send the details of the non-UK issued EHIC to NHS England (nhsdigital.costrecovery@nhs.net) and send the S1 form to the Overseas Healthcare team via email (nhsbsa.faregistrationsohs@nhs.net) or post. If a registration form has been submitted online via the Register with a GP Surgery Service, then such forms do not need to be sent manually as they will automatically be sent to NHS England as part of the service.
4.4.6 The Department of Health has agreed to provide practices with hard copy patient leaflets which will explain the rules and entitlements of overseas patients accessing the NHS in England.
4.4.7 It is important to note that there is no set length of time that a patient must reside in the country in order to become eligible to receive NHS primary medical services.
4.4.8 Therefore, all asylum seekers and refugees, students, people on work visas and those who are homeless, overseas visitors, whether lawfully in the UK or not, are eligible to register with a GP practice even if those visitors are not eligible for secondary care (hospital care) services.
4.4.9 The length of time that a patient is intending to reside in an area dictates whether a patient is registered as a temporary or permanent patient. Patients should be offered the option of registering as a temporary resident if they are resident in the practice area for more than 24 hours but less than 3 months. In some cases, a prospective patient may not know how long they will reside in an area, for example, destitute asylum seekers housed in temporary Home Office commissioned ‘initial’ accommodation. Generally, in such cases where there is uncertainty over the length of time that a patient may be residing in an area, but this is likely to be months rather than weeks, NHS England advises that the patient should be registered as a permanent patient.
4.4.10 An immigration health charge (or ‘surcharge’) is now payable by non-UK nationals who apply for a visa to enter or remain in the UK for more than 6 months. People with indefinite leave to remain in the UK and those not subject to immigration control (eg diplomats posted to the UK) are not liable to pay the surcharge, but maybe ordinarily resident here and entitled to free NHS healthcare on that basis.
4.4.11 Payment of the health surcharge entitles the payer to NHS-funded healthcare on the same basis as someone who is ordinarily resident, from the date their visa is granted and for as long as it remains valid. They are entitled to free NHS services, including NHS hospital care, except for services for which a UK ordinary resident must also pay, such as dentistry and prescriptions in England.
4.4.12 Payment of the health surcharge is mandatory when making an immigration application, subject to exemptions for certain categories of people and the discretion of the Home Secretary to reduce, waive or refund all or part of a surcharge payment. Most of these groups also receive NHS-funded healthcare on the same basis as an ordinarily resident person.
4.4.13 Patients who have paid this surcharge as part of their visa application process should be registered as with any other patients.
4.5 Immediately necessary treatment
4.5.1 General practices are also under a duty to provide emergency or immediately necessary treatment, where clinically necessary, irrespective of nationality or immigration status.
4.5.2 The practice is required to provide 14 days of further cover following provision of immediate and necessary treatment.
4.6 Determining if the patient lives in the practice area or is registered on a Special Allocation Scheme
4.6.1 All practices are required to have agreed an ‘inner’ boundary with their commissioner. Anyone who resides within the practice’s inner boundary is entitled to apply to register for primary medical services and the practice boundary should be clearly advertised to patients on the GPs practice leaflet or website if they have one.
4.6.2 In addition, most practices have also agreed an ‘outer’ practice boundary.
4.6.3 Patients who move out of a practice’s inner boundary area but still reside in the outer boundary area may be able to remain registered with the practice if they wish and the practice agrees.
4.6.4 GP practices are able to register new patients who live outside the practice area without any obligation to provide home visits or services out of hours when the patient is unable to attend their registered practice. It is for a practice to decide, at the point of registration, whether it is clinically appropriate and practical to register the individual patient in that way.
4.6.5 Practices are reminded when considering new patients on the register to check GP links and email from PCSE which notifies the practice the registration should be declined for reasons patient is already registered on the Special Allocation Scheme.
4.7 Access to registration
4.7.1 Practices should ensure there is equitable access for all patients who wish to register with them. Registration should be available to all patients every day rather than on particular days and throughout the practice’s advertised opening hours.
4.7.2 Where possible, it is good practice for practices to provide pre-registration documentation in advance, eg to help patients understand the practice and the services they deliver.
4.7.3 It is It is possible for patients to register via paper form or digital/online and practices should make clear to patients the different ways in which they can register with their practice.
4.7.4 Updates to the GP contract in 2022/2023 removed the need for a patient to provide a wet signature for registration.
4.7.5 An online registration service and corresponding paper form, developed by NHS England is now available to all practices in England to use, further information on this service can be found on the Register with a GP surgery service resource hub.
4.7.6 Patients have the right to change practices if they wish. The grounds on which a practice can refuse a registration are limited – see section 4.9 for further detail.
4.8 New patient health checks
4.8.1 It is a contractual requirement that once registered all patients must be invited to participate in a new patient check however neither registration nor clinical appointments should be delayed because of the unavailability of a new patient check appointment.
4.9 Requesting documentary information from patients
4.9.1 Under the terms of their primary medical services contracts, GP practices cannot refuse an application to join its list of NHS patients on the grounds of race, gender, social class, age, religion, sexual orientation, appearance, disability or medical condition.
4.9.2 Practices can refuse an application to join a practice list if:
- the commissioner has agreed that they can close their list to new patients
- the patient lives outside the practice boundary
- if they have other reasonable grounds
4.9.3 In practice, this means that the GP practice’s discretion to refuse a patient is limited.
4.9.4 In addition, when patients seek to register there is no regulatory requirement for patients to prove identity, address, immigration status or the provision of an NHS number in order to register. However, there are practical reasons why a practice might need to be assured that people are who they say they are, or to check where they live. Seeing some form of documentation regarding the patient’s identity can help to ensure the correct matching of a patient to the NHS central patient registry, thereby ensuring any previous medical notes are passed onto a new practice. It is legitimate therefore for the practice to apply a consistent but non-discriminatory policy to ask for patient ID as part of their registration process.
4.9.5 Any practice that requests documentation regarding a patient’s identity or immigration status must apply the same process for all patients requesting registration equally. Acceptable exceptions to this are outlined in 4.9.6, 4.9.7. A practice policy should not routinely expect a patient to present a photograph as this could be discriminatory.
4.9.6 The majority of patients will not find it difficult to produce ID/residence documentation, however there will be some patients who do live in the practice area but are legitimately unable to produce any of the listed documentation. Examples of this may be:
- people fleeing domestic abuse staying with friends, family or in a shelter
- people living on a boat, in unstable accommodation or street homeless
- people staying long term with friends but who aren’t receiving bills
- people working in exploitative situations whose employer has taken their documents
- people who have submitted their documents to the Home Office as part of an application
- people trafficked into the country who had their documents taken on arrival
- children born in the UK to parents without documentation
4.9.7 Reasonable exceptions therefore need to be considered and the individual registered with sensitivity to their situation.
4.9.8 As there is no requirement under the regulations to produce identity or residence information, the patient must be registered on application unless the practice has reasonable grounds to decline. These circumstances would not be considered reasonable grounds to refuse to register a patient and neither should registration or access to appointments be withheld in these circumstances. If a patient cannot produce any supportive documentation but states that they reside within the practice boundary then practices should accept the registration
4.9.9 Where necessary, (eg homeless patients), the practice may use the practice address to register them if they wish. Further, they could use an address which the local authority has provided to the patient to use. If possible, practices should try to ensure they have a way of contacting the patient if they need to (for example with test results).
4.9.10 If a practice suspects a patient of fraud (such as using fake ID) then they should register and treat the patient but hand the matter over to the NHS Counter Fraud Authority (NHSCFA)
- NHS Counter Fraud Authority Reporting Line: 0800 028 4060
- report to the NHSCFA using the online NHS fraud reporting tool
- by post to the NHS Counter Fraud Authority, Skipton House, 80 London Road, London, SE1 6LH
4.10 Refusing registration
4.10.1 If a practice refuses any patient registration, then they must record the name, date and reason for the refusal and write to the patient explaining why they have been refused, within a period of 14 days of the refusal.
4.10.2 This information should be made available to commissioners on request. Commissioners may ask practices to submit the numbers of registration refusals, age, ethnicity, and reasons as part of their quality assurance process.
4.11 Patients who are temporarily resident in a specialist hospital away from home
There has been some confusion in respect of part 5, regulation 17 (4) of the GMS regulations.
4.11.1 This regulation is not considered ‘reasonable grounds’ to refuse registration according to legal advice. 17(4)(b) relates to patients who are already registered with the GP practice and cannot be used as a reason/justification for not registering certain patients. These only become relevant after a patient is registered it does not provide grounds for a refusal to register the patient in the first instance.
4.11.2 There are no legal grounds for refusing to register a patient because they are an inpatient in a hospital. Indeed, the gatekeeper’ role of the NHS GP for accessing secondary care services depends on patient registration.
4.11.3 Practices are not however expected to provide anything other than essential and minor surgery in these circumstances. If the resident requires any other services these must be arranged by the hospital or the commissioner. The commissioner who is responsible for securing specialist hospital services should ensure that all services over and above those normally associated with general practice are both agreed as part of the contract specification and actively monitored to ensure delivery against that specification.
4.11.4 A template memorandum of understanding (MOU) is provided to support GPs, commissioners and providers in clarifying the contractual requirements of primary care providers and those of the hospital, and the regulatory and professional obligations of the clinicians to ensure safe care and example MOUs are also provided that describe ‘shared care’ arrangements/responsibilities so that patients receive holistic care.
4.11.5 There are however instances where patients’ temporary residence is in a specialist hospital away from home. Where spells are for longer periods of time, commissioners should consider establishing integrated primary and specialist care offer for those patients to ensure essential and additional primary medical services are able to be met more effectively. In those instances, the commissioner when securing specialist hospital services will want to ensure those services normally associated with general practice are agreed as part of the contract specification and actively monitored to ensure delivery against that specification. This will require use of the APMS contract ‘bolt-on’ available to the NHS standard contract.
4.12 Registering children
4.12.1 As a minimum requirement the arrangements above in respect of the registration of any patient with a GP surgery should be followed when the person registering is a child. However, there are circumstances that practices should be aware of, in relation to safeguarding guidance.
4.12.2 The legal definition of a child is 0 to 18 years of age; however young people may be able to make independent decisions from as young as 13 years old, depending on their Gillick competency. Section 11 of the Children Act 2004 places a statutory duty on the NHS to safeguard and promote the welfare of all children up to the age of 18yrs. The Victoria Climbie Enquiry Report 2003 (9.104) stresses the importance of GP registration for every child. It sets out the importance of knowing the identity and name of those registering the child and their relationship to that child.
4.12.3 If a child under 16 attempts to register alone or with an adult that does not have parental responsibility, the practice child safeguarding lead should be alerted.
4.12.4 For purposes of safeguarding children, the following should be considered whilst recognising that patients must still be registered in the absence of documentation and policies must be applied in a non- discriminatory manner.
4.12.5 The practice should seek assurance through:
- proof of identity and address for every child, supported by official documentation such as a birth certificate (eg, this helps to identify children who may have been trafficked (Modern slavery: statutory guidance for England and Wales (under section 49 of the Modern Slavery Act 2015) and non-statutory guidance for Scotland and Northern Ireland or children who are privately fostered)
- an adult with parental responsibility should normally be registered at the practice with the child. There may be legitimate exceptions to this, such as where both parents are serving in the armed forces and are registered with an ‘armed forces’ GP or practical explanations, eg parents wishing for their child to be registered with a practice closer to school. The ID of the adult is essential as it can be matched to the birth certificate details. However, the practice should not refuse to register a child if there is no-one with parental responsibility who can register, as it is generally safer to register first and then seek advice from the practice child safeguarding lead, health visitor or practice manager. (This situation may alert you to a private fostering arrangement which will require notification to the local authority)
- offering each child, a new patient registration health check as soon as possible after registration
- proof of parental responsibility or relevant guardianship agreements
- seeking collaborative information (supported by official documentation) relating to:
- current carers and relationship to the child
- previous GP registration history
- whether the child is registered with a school and previous education history
- previous contact with other professionals such as health visitors and social workers
- children who have been temporarily registered with the practice should be reviewed regularly and proceed to permanent registration as soon as possible and ideally within 3 months of initial registration. Likely length of stay should be determined at initial registration and patient registered as temp/permanent as appropriate
- children of parents or carers, who have been removed from the list for any reason, must not be left without access to primary care services
- where parents or carers have been removed from the list due to aggressive and or violent behaviour a risk assessment should be completed to identify any risk to their children and the appropriate referrals safeguarding made. Please ensure you consult relevant safeguarding procedures and record any referral decision
- a ‘think family’ approach should be made when seeing either the adult(s) or child/children within the surgery. If you are aware that an adult has significant risk-taking behaviour, chronic mental health concerns or repeated episodes of stress and anxiety, safeguarding and support consideration should be made to the welfare and safety of the child/children being cared for by that adult
4.12.6 Practices should be alert to potential risks such as those described above when young people aged between 16-18 years of age register alone and dealt with in line with practice safeguarding procedures and escalated outside of the practice through the local procedures if appropriate,16 to 18-year-olds are still children by law of child protection but can also be parents and carers. It’s imperative that we consider the risks and vulnerabilities within this age group.
4.12.7 There is nothing to stop a parent deregistering their family and not registering again. It is not compulsory to be registered with a GP whether an adult or a child. To amend this there would need to be legislative change. Such legislation would encroach on areas of personal freedoms and patient and parental rights so would likely attract resistance. In addition, it is difficult to see how to enforce or police as there is no jurisdiction or levers to ensure that all children are registered.
4.12.8 If a practice is concerned about a family who is deregistering their children with no plan to register with another general practice, they need to consider whether this should be raised with the local authority as part of normal safeguarding processes.
4.13 Registration of those previously registered with defence medical services and priority NHS care for veterans
4.13.1 Defence medical services (DMS) have their own GP services that look after serving personnel, mobilised reservists, and some families. These specific primary care services are commissioned separately by the DMS of the Ministry of Defence. When servicemen and women leave the armed forces, their primary healthcare reverts to the responsibility of the local NHS. As a minimum requirement, the arrangements set out above in respect of the registration of any patient with a GP surgery should be followed when the person registering is a veteran. Prior service should be recorded on registration and allocated the correct read/SNOMED code. This should enable access to specialist or bespoke care or charity support as necessary for such patients and for the delivery of the armed forces covenant.
4.13.2 A veteran is an ex-service person or reservist who has served in the armed forces for at least 1 day. There are around 2.5 million of these veterans in England at the time of drafting.
4.13.3 All veterans are entitled to suffer no disadvantage from their service and to receive priority access to NHS hospital care for any condition as long as it’s related to their service (subject to clinical need), regardless of whether or not they receive a war pension.
4.13.4 All people leaving the armed forces are given a summary of their medical records, which they are advised to give to their new GP when they register. The practice will also normally be advised automatically of prior registration with defence medical services (with a summary of their in-service care).
4.13.5 More information on the duty of care owed to service personnel and specific services is contained in the Armed Forces covenant.
4.14 Persons released from prisons, immigration centres or children’s secure facilities.
4.14.1 We have introduced a contractual change in October 2017 to allow patients who do not have a registered GP or are being released to a different area ability to register with a practice before they leave the detained estate. This agreement includes the timely transfer of clinical information, with an emphasis on medication history and substance misuse management plans, to the practice from the detained estate healthcare service to enable better care when a new patient first presents at the practice.
4.14.2 Those in contact with the Criminal Justice System may get a letter from the Youth Offending Service, the Committee for the Right of the Child or the National Probation Service
4.15 Registering civil servants and their dependants, and the dependants of members of the Armed Forces, returning from overseas postings
4.15.1 Contractual changes in October 2021 enable civil servants who are posted overseas, and their relevant family members (see 4.15.9 for the definition of ‘relevant family member’) who have accompanied them on their posting, and relevant family members who have accompanied a member of the Armed Forces (a ‘service person’) posted overseas, to register with a GP practice more easily. This includes as a permanent patient or temporary resident, and in advance of (or upon) their return to the UK. This is because these individuals have faced challenges registering and accessing primary medical services in a timely way when returning to the UK from overseas postings.
Registration with a patient’s previous practice or its successor
4.15.2 Where an application is made to a contractor by one of the following individuals, the contractor must accept them, even if their patient list is closed. (The only exception to this is where the contractor has reasonable grounds to refuse the application; see 4.15.8):
- civil servants returning to the UK from an overseas posting (or former civil servants who were posted overseas and are returning to the UK for the first time since leaving the civil service) – provided they were registered with that contractor or a predecessor contractor immediately before that posting or the first of consecutive postings. A ‘predecessor contractor’ is a contractor (‘A’) whose obligations to provide services have been partly or fully assumed by the contractor to which the application for registration is made. This will cover practice mergers, as well as where, in relation to a general medical services contract, there has been a change of status from individual medical practitioner to partnership (or vice versa).
- relevant family members of a civil servant (or former civil servant) who are returning to the UK and immediately before their return are or were accompanying the civil servant (or former civil servant) on their overseas posting – provided the civil servant (or former civil servant) was registered with the contractor or a predecessor contractor immediately before that overseas posting or the first of consecutive postings
- relevant family members of a current or former service person who are returning to the UK, and who, immediately before their return to the UK, are or were accompanying the current or former service person on an overseas posting – provided the family member was registered with the contractor or a predecessor contractor immediately before accompanying the service person on that overseas posting or the first of consecutive postings
4.15.3 The application in 4.15.2 may be made up to, but not more than, 1 month before that individual’s planned date of return to the UK, and if the application is for permanent registration, it must be made no later than 3 months after the patient’s arrival in the UK. Applications for permanent registration made after the end of the 3-month period are to be dealt with in the same way as any other patient registration request.
Registration with a new practice
4.15.4 Where an application is made by one of the following individuals, the contractor must register them, if their patient list is open. (The only exception to this is where the contractor has reasonable grounds to refuse the application; see 4.15.8):
- civil servants (or former civil servants) returning to the UK from an overseas posting, who were not previously registered with the contractor or a predecessor contractor
- relevant family members who are returning to the UK and who: (a) are or were accompanying a civil servant (or former civil servant), or a service person (or former service person), on their overseas posting from which they are returning, and (b) are not required to be treated as previously registered with the contractor (see 4.15.2)
If the contractor’s list of patients is closed, it may register the individual if they are an immediate family member of a registered patient.
4.15.5 The application in 4.15.4 may be made up to 1 month before that individual’s planned date of return to the UK. If the application is for permanent registration, it must be made at least 24 hours before the planned return date. Applications for permanent registration which are made less than 24 hours before the planned return date, or after the individual returns to the UK, are to be dealt with in the same way as any other patient registration request.
4.15.6 Applications in 4.15.2 and 4.15.4 may be made in-person or remotely, for example via posting or emailing a signed printed or scanned GMS1 or GMS3 form (as relevant) to the contractor. The form should be sent to the contractor with the following additional information:
a) Confirmation the patient is seeking registration under the contract provisions for crown servants returning from overseas postings.
b) The patient’s planned date of arrival in the UK.
c) Anticipated length of stay in the UK (if not permanent and if known).
d) List all relevant family members (where applicable).
e) Proof of being, or having been, overseas in the circumstances defined in 4.15.2 and 4.15.4. This would normally be some documentary evidence or cover letter from the employer of the current or former civil servant/service person.
Should the practice need to validate that a patient was previously registered with them (or their predecessor contractor) immediately before they went overseas, the practice may confirm this through the PDS or National Health Application and Infrastructure Service(NHAIS)/Primary Care Registration Management (PCRM).
If the practice cannot confirm prior registration with them, it may request proof from the patient (eg letter, email, text message). If neither the practice or the patient are able to evidence prior registration, the practice may still choose to accept the individual’s application if it is nevertheless satisfied that they or the patient of which they are a relevant family member (as the case may be) was previously registered with the practice (or its predecessor contractor) – eg a practice may see proof of an individual being previously resident in that practice’s area as sufficient to accept their application.
Date of registration and duty to provide care
4.15.7 Where a contractor accepts an application in 4.15.2 or 4.15.4 for:
- temporary registration, it must confirm this with the individual or the appropriate person. The contractor’s responsibility for that individual begins on the later of: (a) the date on which the contractor accepts the application, and (b) the date on which the individual returns to the UK. The contractor must notify its commissioner that it accepted the individual as a temporary resident at the end of the contractor’s period of responsibility for that individual
- permanent registration, the contractor must give notice in writing to its commissioner of that acceptance as soon as possible. If the application is accepted before the individual’s planned return date, the contractor must notify the commissioner of that return date. The commissioner must add the individual to the contractor’s list of patients from the later of: (a) the date on which the commissioner receives the relevant notice from the contractor, and (b) the date on which the individual returns to the UK. The contractor is not required to provide primary medical services to that individual before their actual return to the UK
Once a contractor has accepted an application, regardless of whether the individual is still overseas, the contractor may book upon request appointment(s) for that individual which are only to take place once the individual has arrived in the UK. Individuals must not attend appointments (ie remote appointments) with the contractor while they are still overseas.
4.15.8 A contractor may only refuse to register individuals in 4.15.2 under the crown servant registration provisions where it has reasonable grounds for doing so. Such grounds must not relate to the patient’s race, gender or gender reassignment, marriage or civil partnership, pregnancy or maternity, social class, age, religion or belief, sexual orientation, appearance, disability or medical condition. Reasonable grounds may include, in the case of an application for permanent registration, that the patient does not live, or does not intend to live in, the contractor’s practice area or the outer boundary area. Where a contractor refuses to register a patient, this decision, and the reasons for it, must be communicated to the patient (or the person who made the application on their behalf) in writing within 14 days of that decision being made. The contractor must keep a written record of applications and reasons for refusal.
4.15.9 Under these specific regulations, the following are relevant family members of a current or former civil servant/service person [1]:
- their children (including adopted and stepchildren, as well as natural children), if:
- they are, or were, at the time of leaving the UK to accompany the civil servant or service person on their overseas posting, under 21 (or under 25 in the case of the child of a service person) and wholly or mainly financially dependent on the civil servant or service person whilst accompanying them, or
- they are or were wholly or mainly financially dependent on the civil servant or service person whilst accompanying them on their posting because of a disability [2]
- their spouse, civil partner, or individual whose relationship with the current or former civil servant or service person has the characteristics of a relationship between spouses or civil partners
- their former spouse, civil partner, or individual whose relationship with the current or former civil servant or service person has ended (for any reason) but had the characteristics of a relationship between spouses or civil partners
- their widow/widower or surviving civil partner if the civil servant or service person passed away while on their posting
Individuals who become relevant family members of a current or former civil servant/service person during an overseas posting and are returning to the UK are to be treated in the same way as those who were family members before the start of such a posting. This includes, for example, a child born, or adopted, during an overseas posting who remains with their civil service parent throughout that posting, or a person who marries a civil servant during their overseas posting and accompanies that person on their posting from that time.
[1] See the definition of “relevant family member” in paragraph 32A(7) of schedule 3 to the National Health Service (General Medical Services Contracts) Regulations 2015 and in paragraph 31A of schedule 2 to the National Health Service (Personal Medical Services Agreements) Regulations 2015. These provisions were inserted by the National Health Service (General Medical Services Contracts and Personal Medical Services Agreements) (Amendment) (No. 2) Regulations 2021.
[2] As defined in part 2, chapter 1, section 6 of the Equality Act 2010.
4.16 Armed Forces: dual registration and GP Contract
4.16.1 Under the terms of their primary medical services, general practitioners (GPs) have the ability to register members of the armed forces of the Crown for a period of up to 2 years. To be eligible for registration, the patient must obtain written authorisation from the defence medical services and must reside or work within the practice area during the specified time period mentioned in the authorisation.
4.16.2 The arrangements for including armed forces personnel on a contractor’s patient list are outlined in clause 13.5A of the GMS Contract. You can find the latest version of the contract, which includes this clause, on the NHS England website.
The same clause is included in the 2015/16 GMS Contract (page 67).
The corresponding regulations can be found in the GMS regulations 2015, schedule 3, paragraph 19.
4.17 Temporary residents
4.17.1 A contractor may, if the contractor’s list of patients is open, accept a person as a temporary resident. This is provided the contractor is satisfied that the person is temporarily resident away from their normal place of residence and is not being provided with essential services (or their equivalent) under any other arrangement in the locality where that person is temporarily residing; or moving from place to place and not for the time being resident in any place.
4.17.2 It is of note that a notification to the commissioner of the acceptance of temporary resident on to the contractor’s list only occurs at the end of the period of 3 months beginning with the date on which the contractor accepted that person as a temporary resident; or if the contractor’s responsibility for that person as a temporary resident came to an end earlier, at that point. Any clinical records relating to the TR period of care can/should be submitted via PCSE for repatriation to the registered GP practice or storage in archive.
4.17.3 As this type of registration does not get flagged with PCSE at the commencement of the temporary registration, there is potential for a contractor to accept as a temporary resident a patient who is actively registered with a Special Allocation Scheme (SAS). Should a contractor become aware that a patient is registered with a SAS, the contractor should contact their local commissioner who may seeks to secure temporary primary medical services for the patient with a local SAS.
4.18 Sensitive patient registrations
4.18.1 GP practices are required to work with PCSE and take actions on their clinical systems to ensure that the registration information for patients who undergo a change of identity is accurate and up to date. This is also the case for adoptions, gender transition and patients in witness protection schemes. This ensures data is kept up to date and held in line with information governance requirements on national demographics systems.
4.18.2 Commissioners must also work with PCSE in relation to managing escalations where there are potential blockages or delays in practices responding to PCSE requests.
5 Temporary suspension to patient registration
5.1 Formal list closure
5.1.1 The GMS and PMS contracts allow for a practice to request permission from its commissioner to close its list to new patients (paragraph 33 of schedule 3, part 2 of the NHS [GMS contracts] regulations 2015). This option exists to give practices a degree of workload control over the management of their services, particularly when there is unusual and sustained demand from patients or in situations of workforce or recruitment difficulties that affect a practices ability to provide services to an acceptable and safe standard.
5.1.2 As the commissioner also has a duty to ensure the availability of primary care services for the resident population it has certain powers with regard to these requests including agreeing to the length of the closure and the conditions that would need to exist to trigger a re-opening of the list. The commissioner will also need to consider the availability of alternative provision for new patients and any impact on neighbouring practices. Following changes to the formal list closure process in 2012, the commissioner does not have the power to halt practices’ delivery of additional and/or enhanced services as a means to reduce practice workload thereby keeping the patient list open. Therefore, list closure no longer carries such financial consequences for the practice as it was once thought to have and allows practices to continue to deliver holistic care to registered patients.
5.1.3 When a practice does formally close its list, the requirement is to close between 3 and 12 months; not less than 3 months. An approved closure notice must specify the time period.
5.2 ‘Informal’ or ‘temporary’ list closure
5.2.1 While the GMS and PMS contracts do not allow for a ‘temporary’ or ‘informal’ list closure they do allow for a practice to refuse individual patient applications for inclusion in a contractors list of patients providing there are reasonable non-discriminatory grounds to do so (GMS regulations: schedule 3, part 2, paragraph 21). In this guidance we distinguish a patient refusal on a case-by-case basis, based on the patient circumstances, from a refusal to allow a patient to join the list because of the circumstances surrounding the provider and so do not consider paragraph 17 to be appropriate in these circumstances.
5.2.2 Practices can, however, suffer unforeseen pressures that can reasonably be predicted to be short term. In these circumstances there may be a real or perceived risk to ‘safe patient care’ by accepting more new patients onto the list and action to address this by the practice should be received by the commissioner as a trigger for support and help.
5.2.3 NHS England has seen a significant rise in the number of practices suspending registration on a temporary basis causing a significant problem for patients, neighbouring practices and commissioners in some areas.
Practices do not exist in isolation so when a practice restricts new patient registration, this has an impact not only on patients but on neighbouring practices. It is for these types of circumstances that the formal list closure procedure exists; to allow for a considered and managed approach to list management across all practices.
5.2.4 Because of the potential impact of ‘temporary suspension’ NHS England encourages practices to open a dialogue with their commissioner as early as possible when considering temporary suspension
5.2.5 These guidelines for commissioners describe the circumstances where a temporary suspension by the contractor of patient registration may be appropriate and the conditions that should govern that decision such that the roles and responsibilities of both parties are not compromised.
5.3 Overview of current activity
5.3.1 The increase in a temporary suspension of patient registration is a symptom of rising pressure in primary care, which creates a risk to patients, neighbouring practices, and the commissioner; however, the risk to patients being registered with an oversubscribed practice should also be considered.
5.4 Facts/principles
5.4.1 Addressing practices seeking to ‘informally’ or ‘temporarily’ suspend patient registration onto their list should be in the context of the General Practice Forward View and NHS England’s commitment to supporting practices in difficulty.
5.4.2 However, NHS England has a duty to ensure that patients have access to primary care.
- Core services include operating an open list by the fact of regulation and is how NHS England ensures access to services; the NHS Act confers a duty on the commissioner to ensure the provision of services.
- Any actions considered by the commissioner should ensure, system-wide, safe, quality and accessible core services to patients and be proportionate and sensitive to the providers concerned.
- NHS England and commissioners have a responsibility to address health inequalities.
- Commissioners and providers must work together to ensure compliance with the Equality Act, ensuring the rights of those with protected characteristics are not directly or indirectly compromised.
- Good medical practice states that if a GP is aware that patient safety is being compromised, then they have a professional duty to act.
- The unintended impact of any action needs to be considered in relation to both registered patients and unregistered patients in the locality as well as the impact on other local providers both primary (GP and pharmacy) and secondary care.
5.4.3 The commissioner has the right to assign patients throughout the period that the list is not formally closed having due regard to the quality and safety of services and the reasons behind the list closure in the first place.
5.5 Issues to be taken into consideration
5.5.1 NHS England acknowledges that things can rapidly change within practices. These may include for example:
- an immediate and unpredicted shortfall in the availability of staff, eg through sickness or a delay to a staff appointment
- an unpredicted surge in demand
- an unexpected event affecting a practice’s ability in the short term to provide the full range of services normally available, eg a flood or a fire (see force majeure provisions of the standard GMS, PMS and APMS contracts)
- impact on a practice of an unfavourable CQC inspection where remedial action temporarily affects normal service provision
5.5.2 In some circumstances the action required to remedy a problem may take several months and in others just a few weeks, eg a planned short-term suspension of registration as part of a recovery plan through the Vulnerable Practice Programme. Alternatively, practice capacity may be temporarily compromised by premises development or IT upgrades. Under these circumstances, it would be usual to expect planning and communication with patients in advance with a specific start and end date and disruption measured in weeks not months.
5.5.3 In all but exceptional circumstances practices should approach the commissioner in advance so that an action plan that minimises the impact on patients can be considered jointly at the earliest opportunity and so that immediate support from the commissioner can be put into action. A request to temporarily suspend patient registration should be considered by the commissioner as a trigger for support as it should for a formal application to close the list.
5.5.4 This guidance does not prescribe what length of time approval of a temporary list suspension is appropriate as this will vary depending on the circumstances. The keywords are unpredictable and/or short term. In circumstances where there is a known history of difficulty in recruitment including the availability of locums or the circumstances affecting the practice can be predicted to last longer, eg a planned refurbishment or a rebuilding programme scheduled to last month’s say following a flood or a fire, the formal list closure procedure should be encouraged.
5.5.5 In both cases the practice’s eligibility for support through the Practice Resilience Programme should be considered by the commissioner.
5.5.6 Circumstances in which an ‘informal’ or ‘temporary’ list closure is not appropriate (list not exhaustive)
- When the practice considers its list is full (a formal application should be made).
- For long-term sickness absence (a formal application should be made).
- For issues expected to be longer term (eg over 3 months).
- Because a formal closure application has been declined.
5.6 Process to be adopted
5.6.1 All practices should be encouraged to contact their commissioner at the earliest possible opportunity, ie at the point that suspension to registration is being considered so that the provider and commissioner can work together to agree on what support is required.
5.6.2 At this point commissioners should:
- seek to understand the reasons behind the action
- engage the LMC at the time of a decision as the LMC also carries a responsibility for representing all their affected parties
- facilitate what action needs to take place by the practice and/or by the commissioner for the list to be re-opened. If actions can reasonably be expected to take longer than 3 months, the practice should be asked to make a formal application to close its list
5.6.3 Actions should trigger consideration of the practice resilience programme or use of section 96, e.g. a diagnostic/review of the difficulties faced and recommended action.
5.6.4 At the end of the agreed period where a temporary suspension of patient registration has occurred, the list would normally re-open. There are only 2 alternative outcomes:
- if the situation is almost resolved for example an appointment has been made but the post not yet filled (for example by a week or two later) an extension to the temporary arrangement can be negotiated
- despite support to deliver an action plan the practice continues to feel compromised. The commissioner should then consider an application for formal list closure, which will require wider consultation. The parties will need to agree on the status of the practice list during the formal process, whether, having regard to all local circumstances, the practice should continue to operate a temporary suspension to patient registration
5.6.5 These guidelines have been drafted in recognition of the immediate pressures facing some practices; they do not however sanction the term ‘open but full’. Where a practice is failing to engage with the commissioner, and unilaterally seeking to determine its own restrictions on patient access, without consideration of the impact on patient access generally or the implications for neighbouring practices, then contractual action may need to be considered.
6 Managing [non-violent] inappropriate and unacceptable patient behaviours, including protecting against discrimination, harassment or victimisation
Introduction
This chapter supplements and should be read alongside guidance provided under chapter 3: managing patient lists and chapter 7: managing violent patients – Special Allocation Scheme, to support the management of inappropriate and unacceptable patient behaviours, including to protect practice teams and other patients from discrimination, harassment or victimisation.
6.1 Key areas
Given the importance of the interests this guidance seeks to balance, ensuring that inappropriate and unacceptable patient behaviours are appropriately managed, while ensuring all patients are able to access primary medical services they need and are entitled to, this guidance covers the following key areas:
- the scope of inappropriate and unacceptable patient behaviours
- contract regulations and managing inappropriate and unacceptable patient behaviours
- the process for managing inappropriate and unacceptable behaviours
- considerations for ensuring ongoing access for patients removed from a practice patient list due in inappropriate and unacceptable patient behaviours
6.2 The scope of inappropriate and unacceptable patient behaviours
6.2.1 Many providers have and operate local policies to support positive patient behaviours they wish to encourage and outline those behaviours that will not and should not be tolerated, eg through patient charters, zero-tolerance or respect policies etc.
Inappropriate and unacceptable behaviours may include but are not limited to:
- using bad language or swearing at practice staff or other service users
- racial abuse
- sexual harassment
- unnecessarily persistent or unrealistic service demands that cause disruption
- causing damage to practice premises or to the property of staff or other service users
- stealing from practice premises, staff or other service users
- obtaining drugs and/or medical services fraudulently
Under usual circumstances, patients must not be immediately removed from a practice list for minor offences not reported to the police or behaviour that was not appropriate to report to the police, eg a patient who has never been aggressive before and/or who is clearly suffering mental or physical distress. In such circumstances, it might be more appropriate to use the standard procedure for a breakdown in practice/patient relationship, usually this is undertaken by writing to the patient requesting an explanation or apology and warning that a continuation of such behaviour could result in them being removed from the practice’s list. Practices may also choose to use or agree on a good behaviour contract with the patient to support their continued registration.
6.2.2 Violence and threatening abuse is dealt with separately in chapter 7 but it is acknowledged the behaviours above can escalate to include or happen alongside violence and abuse.
6.2.3 Common to all such policies should be the underlying set of principles and values that are set out in the NHS Constitution which bind together the communities and patients the NHS serves and the people who work in it. Everyone has a right to be treated fairly and equally, with dignity and respect, and free from discrimination and harassment, and violence and abuse. There are extensive legal rights, embodied in general employment and discrimination law.
6.2.4 The protection and safety of the providers teams’ (and other service users) mental health is as important as the protection and safety of their physical health. NHS England supports and requests that providers practice policies addressing inappropriate and unacceptable patient behaviours also explicitly include positions on not tolerating any form of discrimination, harassment or victimisation. The following definitions may be useful:
- Discrimination: the act of being treated unfairly because of who they are or because they possess certain characteristics. Within the Equality Act 2010 the following are protected characteristics:
- age
- gender reassignment
- being married or in a civil partnership
- being pregnant or on maternity leave
- disability
- race including colour, nationality, ethnic or national origin
- religion or belief
- sex
- sexual orientation
- Harassment: the act of being subject to unwanted behaviour, which is offensive, intimidating or humiliating. Harassment can happen on its own or alongside other forms of discrimination.
- Victimisation: the action of being singled out for cruel or unjust treatment.
- Microaggressions: verbal, non-verbal, and environmental slights, snubs and insults which communicate hostile, derogatory, or negative messages and behaviours that target a person based on their protected characteristic or belonging to a marginalised group. These can be intentional and unintentional and are based on biases (either conscious or unconscious).
6.3 Contract regulations and managing inappropriate and unacceptable patient behaviours
6.3.1 Where a provider wishes to remove a patient from its practice patient list, removal may normally only be requested if, within the period of 12 months prior to the date of the request, the provider has warned the patient in writing that they are at risk of removal and reasons for this have been stated. However, the contract regulations also acknowledge that it may be justified that a written warning was not possible/appropriate in the circumstances that such a warning would be:
a) harmful to the person’s physical or mental health
b) would put at risk the safety of one or more relevant person(s)
c) the contractor considers that it is not otherwise reasonable or practical for a warning to be given
6.3.2 The General Medical Council states in Good Medical Practice that: “In rare circumstances, the trust between you and a patient may break down, and you may find it necessary to end the professional relationship. For example, this may occur if a patient has been violent to you or a colleague, has stolen from the premises, or has persistently acted inconsiderately or unreasonably”.
6.3.3 Removing a patient from the practice patient list, including without prior written notice under reasonable grounds or grounds of irrevocable breakdown in the relationship, is though expected to be an exceptional event.
6.3.4 Providers will also recognise incidents of patient inappropriate and unacceptable behaviours will need to take into account that service user’s mental health, clinical presentation, neurodiversity and any other health conditions which may influence their behaviour and ensure that patient’s own protected characteristics take no bearing in the consideration process.
6.4 The process for managing inappropriate and unacceptable behaviours
6.4.1 Where a patient has acted inappropriately or unacceptably, the provider will need to carefully consider (taking account of the nature and severity of the incident/behaviour, the impact on practice services, staff or other service users and the patient’s own circumstances) if the incident:
a) meets the relevant criteria for removal from the practice patient list; and, if so, if it is nevertheless willing to continue to manage its relationship with the patient or proceed with the removal; or,
b) does not meet the relevant criteria for removal from the practice patient list, how it will manage its continuing relationship with the patient.
6.4.2 The stated consequence of stepping outside the providers practice polices of expected patient behaviours need to be things that the practice can and will carry out. The process for removing patients from the practice list on reasonable grounds is described in chapter 3. The process for removing violent patients is described in chapter 7.
6.4.3 British Medical Association General Practitioner Committee advice on removing patients from the practice acknowledges “many patients who are misusing services can change their behaviour if it is brought to their attention”.
6.4.4 A warning letter provides such an opportunity and where used should indicate continued registration will cease if the inappropriate or unacceptable behaviour continues or reoccurs and therefore formally documents and evidence reasonable grounds for future removal should it do so.
6.4.5 Acceptable behaviour guidance agreements (or otherwise known as practice-patient or doctor-patient contracts) can also be a useful tool to modify behaviour and should be considered as either a follow up to or used alongside a warning letter. The demands imposed by the agreement need to be reasonable in line with the providers practice policies and any specific demands linked to the individual case (eg requests for personal apology, use of ‘cooling off’ periods) should be fair and not excessively burdensome or disproportionate to the risk.
6.5 Considerations for ensuring ongoing access for patients removed from a practice patient list due in inappropriate and unacceptable patient behaviours
6.5.1 Other than on the grounds of violence or threatening behaviour, the grounds a patient has been removed from a practice patient list should not ordinarily be a factor to be considered by practices when approached by new patients.
6.5.2 Additionally, where a patient has been removed from a practice list but has subsequently been unable to register with a new practice, commissioners may need to assign the patient to a practice whose list of patients is open. Chapter 3, section 3.2.4 ‘where patient assignment to a practice list is required’, is clear on the considerations that should be taken into account by commissioners.
6.5.3 It is recognised some patients can fall into routine cycles of being removed and reregistered. Commissioners should consider how the needs of such patients may be best met and the support providers may need locally to ensure such cycles are broken in the interests of both providers and such patients.
7. Managing violent patients – Special Allocation Scheme
Please note and for information only: other terminology previously used in relation to special allocations of this type have been included but are not limited to, Violent Patient Scheme (VPS) or Zero Tolerance Scheme (ZTS).
7.1 Executive summary and key messages
This chapter provides guidance to commissioners and providers of essential primary medical services in relation to the removal of patients who are violent from their practice list. Special Allocation Schemes (SAS) intends to ensure such patients can continue to receive primary medical services. Provision for SAS is set out in the National Health Service (General Medical Services Contracts) Regulations 2015 and the National Health Service (Personal Medical Services Agreements) Regulations 2015 (together, the regulations).
This guidance focuses on several key themes (which are intended to support the implementation of, and commissioning and monitoring of a SAS:
- introduction
- commissioning a robust SAS
- provider and service requirements and monitoring
- the scope of/eligibility criteria for a SAS
- the process for requesting immediate removal of a patient
- what happens after removal, including returning choice to patient
Given the importance of the interests that SAS seeks to balance, 2 key messages are emphasised at the outset.
The first relates to the scope of SAS. The regulations regarding the removal of patients who are violent is specific in terminology and the regulations require that GMS and PMS contracts provide for “removal from the list of patients who are violent”.
However, within the regulations it is further specified that the grounds on which a contractor may request that a person be removed from its list of patients with immediate effect are that “the person has committed an act of violence against any of the persons specified in subparagraph (2) or has behaved in such a way that any of those persons has feared for their safety“.
The commissioner should therefore be clear that violence does not have to be physical or actual. It can be perceived, threatened or indeed a perceived threat of violence. A person’s fear for their safety can also be actual or perceived. In these circumstances, the regulations specify that a practice can request the immediate removal of that patient from its list. Commissioners should also consider the need to place patients on the SAS.
In the case of requests for the immediate removal of patients whose behaviour is disruptive but falling short of the above grounds, Commissioners should discuss with the practice if the patient should instead be removed from the practice on the alternative ground of irrevocable breakdown in the relationship between the person and the contractor see paragraph 24, schedule 3, part 2 of the GMS regulations and paragraph 23, schedule 2, part 2 of the PMS regulations.
Refer to chapter 3: managing patient lists, section 3.2.3: removing a patient from a practice list and chapter 6: managing [non-violent] inappropriate and unacceptable patient behaviours, including protecting against discrimination, harassment, or victimisation.
The second key message is that we want all providers to be fully aware of and understand the process for immediate removal of a patient. In summary, where a patient’s behaviour is deemed within the scope of this SAS chapter.
The regulations require that, for a patient to be immediately removed from a practice list, the practice must report the incident to the police. The following 14-point process is designed to work in all but very exceptional circumstances. Those infrequent and exceptional cases relate solely to commissioner instigated allocations (eg a patient that falls within the remit of a SAS allocation, but with no recent removal from a GP practice) and must be discussed and agreed with the commissioner in advance.
1. The practice calls the police to report the incident (which is required under the regulation), obtain a response (if required) and police incident number. Where possible the police incident number should be provided at the time of reporting the incident but must be included within the written report provided by the practice within 7 days (a contractual requirement under ‘reasonable requests for information’). **Practice action **
Note: practices should be reminded of the statutory requirement to notify the Care Quality Commission (CQC) about any incident related to their service that is reported to or investigated by the police.
Furthermore, where appropriate the practice should consider if the incident and subsequent removal from its list warrants notification to any other agency (eg local authority) where there may be concern for welfare or safeguarding concern because of the incident (ie the deducted patient has children or is a carer for another vulnerable person including elderly relatives).
2. Having assured itself that the removal is not as a result of the patients protected characteristics and key past medical history including mental health, learning disability and neurodiversity, the practice requests an immediate removal from NHS England’s Primary Care Support England (PCSE) Service provided by Capita. Ideally this request should be made by emailing patientremovals@nhs.net completing and attaching annex 1 – Primary Care Support England Request for removal of patient from practice list form or by telephone, visit the PCSE website for PCSE contact details. PCSE will request the police incident number [note: this is different from a crime reference number, which can only be allocated by the police once it has been established that a crime has been committed. The police will however record an incident number on police systems for all incidents according to Home Office counting rules (HOCR). If the practice does not have a police incident number at this point (which should be in exceptional circumstances only), the practice will be asked to provide details of the date, time and mechanism (eg 999, 111, local number) via which the incident was reported to the police. The absence of an incident number will not delay the immediate removal of a patient. ** Practice and PCSE actions **
3. PCSE removes the patient from the practice list and informs the appropriate commissioner. ** PCSE action **
4. The regulations require the practice notifies the patient in writing that a request for removal has been made, unless to do so would harm the patient’s physical or mental health or put others on the practice premises at risk. ** Practice action **
5. PCSE allocates the patient to an appropriate SAS provider. Commissioners are responsible for commissioning SAS either from GPs or another provider. ** PCSE action **
6. PCSE notifies the patient in writing (annex 7: standard patient communication from PCSE) that they have been removed from the practice list (as per the regulations (general medical services, schedule 3, part 2 patients: general, regulation 25(7) or personal medical services, schedule 2 other required terms, part 2 patients: general, regulation 24(7) removal from the list of patients who are violent) and allocated to the SAS provider. ** PCSE action **
7. The practice provides a follow up report in writing to the commissioner (refer to number 2 above (annex 1 primary care support england request for removal of patient from practice list form) within 24 hours where possible but before the end of a period of 7 days beginning with the date on which notice was given. Where the practice was unable to provide a police incident number initially; the practice will be asked to include this in the report (under the contractual requirement for reasonable requests for information). ** Practice action **
8. Following 7 days from the incident, the commissioner and PCSE will liaise to ensure an incident number has been received (either by PCSE or via the written practice report to the commissioner). In the event an incident number has not been provided, the commissioner will contact the practice to ensure one has been obtained and provided. ** Commissioner action **
9. The SAS provider will provide all new allocated patients with a welcome letter. ** SAS provider action **
10. As part of new patient assessment, SAS provider must be commissioned to undertake and embed initial appropriate assessment, referring to the commissioner any case where the SAS provider believes the referral may be inappropriate. The commissioner should discuss the referral with the referring provider and support patients to find an alternative primary medical service provider in cases where the patient has not been accepted onto SAS. [note: initial appropriateness assessments should be part of all newly commissioned SAS services and where possible commissioners should seek to make arrangements (eg as part of contract review processes) to be add to existing service contracts)].
11. The SAS provider will ensure risk assessment and regular monitoring including rehabilitation of the patient’s behaviour which triggered the removal and allocation to the SAS, together with any other behaviours or areas of concern identified through risk assessments and regular monitoring. This is to enable the patient to be repatriated back into mainstream GP practice (primary care) as soon as is reasonable to do so. ** SAS provider action ** – sample risk assessment (annex 5).
Note: commissioners should ensure the SAS providers initial risk assessment of a new patient includes: a) a level of security and safety measures required, b) patient care plan, c) assessment of the patient’s rehabilitation needs to enable discharge from the SAS, d) travel needs of the patient and e) safeguarding considerations.
Depending on the needs of the patient examples of rehabilitation options could include counselling, anger management, drug and alcohol interventions and other local initiatives or pilot programmes on rehabilitation. A recent course has been made available to support staff to handling difficult conversations with compassion, the following links may be useful:
- Handling difficult situations with compassion – e-learning programme
- Handling difficult situations – caring for yourself and others with compassion – e-learning
The patient’s risk assessment should be continually reviewed and updated after each patient encounter by the SAS Provider with an aim of returning choice back to the patient where safe to do so.
12. The SAS provider will notify PCSE when choice has been returned to the patient and they have been removed from the SAS. This will ensure the patient’s records are amended accordingly by PCSE (ie flag removed from patient record) allowing the patient to re-register at their chosen practice. ** SAS provider and PCSE action **
13. Where a commissioner considers that its existing SAS provider(s) is unable to meet the exceptional needs of a patient allocated to it, it may be necessary to commission a bespoke service for the patient.
14. Where a patient on the SAS moves address and between commissioners and a change in SAS provider is required, the previous SAS provider must ensure a safe transfer (eg by secure email) of an electronic summary of the patient record to the new SAS provider as soon as possible but not later than 5 days following deduction, to ensure continuity of care while the new provider awaits the transfer of the patient’s full medical records.
7.2 Introduction
Purpose of this document
7.2.1 In response to concerns of increasing abuse towards primary care staff following the second wave of the covid-19 pandemic, the NHS England primary medical services policy and guidance manual (PGM) has been updated to support further consistency of service delivery.
7.2.2 There will undoubtedly be instances when practices have to deal with patients who are difficult, challenging, aggressive and abusive, as well as in some cases, violent. In order to protect GP’s and practice staff and to allow them to carry out their roles, commissioners, in collaboration with the wider stakeholders, have developed this guidance.
7.2.3 Under the SAS, designated GP practices or another provider will provide services to patients by prior appointment and at specific locations and times as detailed in individually agreed contracts. Patients are allocated to SAS following a process of immediate removal because of an incident that was reported to the police.
7.2.4 The purpose of this document is to provide commissioners with consistent national guidance to support good commissioning of SAS. It aims to provide a steer on the implementation of SAS in practice and how to work with Primary Care Support England (PCSE), which is delivered on behalf of NHS England, by Capita Plc. Refer to section 7.3 – commissioning a robust SAS, below.
Background to this work
7.2.5 The Special Allocation Scheme (SAS) (originally known as the Violent Patient Scheme [VPS]) was introduced as a Directed Enhanced Service in 2004 and is still referred to in the directions as VPS. The aim to provide a secure environment to patients who have been removed from their GP practice and allocated to the SAS scheme so they can continue to receive primary medical services. The SAS cannot be used in any other circumstances without express and prior agreement of the commissioner.
7.2.6 This SAS allows commissioners to balance the rights of patients to receive primary medical services from the SAS provider to ensure that specified persons, including GPs, their staff, patients, and others on the premises, deliver and receive those services without actual or threatened violence or other reasonable fear for their safety.
7.2.7 Removing a patient under the regulations is considered to be a rare event and should only be used as set out in this section. Refer to part B, chapter 3: managing patient lists and chapter 6: managing [non-violent] inappropriate and unacceptable patient behaviours, including protecting against discrimination, harassment, or victimisation.
Existing arrangements
7.2.8 The administrative arrangements of the existing SAS across England have been disparate and varied. This has created challenges when trying to apply the regulations consistently and the practical application of SAS through a single delivery partner (Primary Care Support England).
Particular issues are as follows.
7.2.9 First, the regulations provide for immediate removal of a patient from a practice list following a phone call from the practice, yet some SAS services require commissioner intervention of some sort before a removal is actioned. This is outside the provisions as set out in the regulations.
7.2.10 Secondly, the regulations require a practice to report an incident to the police but do not mandate the acquisition of a police incident number or crime number before a removal is actioned. NHS England’s stakeholders (including General Practitioners Committee [GPC] England) acknowledge that the provision of an incident number (but not a crime number) is a ‘reasonable request for information’ in accordance with the contract. However, an incident number should not be a prerequisite to the immediate removal of a patient whose behaviour is such that they meet the criteria for removal.
7.3 Commissioning a robust SAS
7.3.1 Commissioners should ensure all commissioned SAS services (new and existing) has:
7.3.2 An equality and health inequality impact assessment (EHIA) undertaken for all commissioned SAS services, which include consideration to increased travel distances and that potential mitigations have been considered. Mitigations may include contribution to travel cost, patient transport and/or mobile outreach services (safety risk assessment supporting). The key point is that the commissioner can show (through documentation, principally an EHIA) that the impact a decision will have on health inequalities has been considered, and that its decision is based on some relevant data and evidence. Refer to part A, chapter 4: general duties of NHS England (including addressing health inequalities) for more information.
7.3.3 Access to services including by telephone, online and face to face.
7.3.4 Pathways to support equitable access needs when patients are managed by a SAS provider out of area, eg access to PCN services, referral to diagnostic services, maternity, district nursing etc.
7.3.5 A comprehensive discharge summary in place and completed at the end after a final risk assessment with the patient. This should be saved in the patients’ medical record, ensuring that it is made available to the receiving practice. The discharge summary should include information on any outstanding referrals in progress and the PCN consideration to the provision of prescription medication to cover the interval of time prior to registering with a mainstream GP practice (normally 3-4 weeks supply).
7.3.6 Arrangements requiring SAS provider to have access to or arrange enhanced security if risk assessment identifies the need.
7.3.7 Arrangements requiring SAS provider to have local information sharing in place where a risk assessment identifies a risk to other staff, ie out of hours, community pharmacy.
7.3.8 Annex 11 provides guidance on commissioning a robust SAS.
7.4 When to request a removal of this type under the regulations (information on eligibility for commissioners and providers)
7.4.1 It is important that these regulations are not misused or used lightly but that it is only reserved for those patients who meet the criteria for removal and resulting in an incident being reported to the police, or for patients who are deemed a future safety risk to themselves or others within the primary care setting.
7.4.2 It is not the intention to encourage a situation where patients are immediately removed for comparatively minor offences (eg that have not been reported to the police) or for behaviour that could be ascribed to a health condition, and which is capable of being alleviated through careful management, care, and treatment. Refer to chapter 6: managing [non-violent] inappropriate and unacceptable patient behaviours, including protecting against discrimination, harassment, or victimisation.
7.4.3 We therefore provide the following comprehensive guidance that outlines circumstances deemed appropriate to remove a patient from the patient list (only intended to be used as a guide and therefore not exhaustive) and emphasises the importance of applying this procedure when strictly necessary. The overarching objective behind an SAS is to ensure any patient removed under the regulations has access to essential services and commissioned enhanced services. Also, to communicate behavioural expectations to patients and educate them to behave responsibly wherever possible, while at the same time minimising the risks to the safety of health professionals and others. Refer to annex 3: SAS sample good conduct guide.
7.4.4 Commissioners should consider how additional support and resources to SAS providers (current and prospective) could be enhanced or put in place.
Increasing local support could include a range of options such as: establishing a community of practice, professional support networks and collaborative working, developing specialist training, learning and development opportunities on key items such as: continuous risk assessment, personal safety and clinical training on trauma informed practice, substance misuse, mental health.
Where an appropriate need for staff training is identified support is also available e.g. handling difficult conversations with compassion, the following links may be useful:
- Handling difficult situations with compassion – e-learning programme
- Handling difficult situations – caring for yourself and others with compassion – e-learning
Types of behaviour covered by this guidance?
7.4.5 The Health Circular 2000/01 defined violence in the primary care context as:
“Any incident where a GP, or his or her staff, are abused, threatened or assaulted in circumstances related to their work, involving an explicit, or implicit, challenge to their safety, wellbeing, or health”.
7.4.6 The main kinds of behaviour which are considered to bring a patient within the regulations covered by this guidance are (these are only intended to be used as a guide and therefore the list is not exhaustive):
Assault
7.4.7 For an assault to fall within the scope of removal from the list, it should involve a person intentionally or recklessly causing another to apprehend the immediate infliction of unlawful force on an individual in a manner which either results in injury or causes that individual to fear injury or some other immediate threat to their safety.
Threatening behaviour
7.4.8 Any verbally threatened harm towards others, with or without accompanying gestures, will fall within the scope of a removal. Threats of nonviolent acts are unlikely to do so (eg use of offensive language without threats).
Behaviour resulting in damage to property
7.4.9 Any behaviour resulting in damage to property, whether accompanied by verbal threats or not and whether that damage is intentional or not, is likely to be within the scope of the scheme if the behaviour was intended to terrorise or intimidate individuals or is seen as a precursor to a personal assault.
Further considerations in relation to 7.4.7 – 7.4.9
7.4.10 Examples of the cases referred to above would include any incident in which the patient has:
- struck, grabbed or punched a GP, member of staff or other individuals, either within the practice premises or elsewhere in a targeted attack
- thrown an inanimate object at a GP, member of staff either within the practice premises or elsewhere in a targeted attack
- struck, grabbed, punched or thrown an inanimate object at other patient(s) within the practice premises
- wielded a weapon, or used an object as one, in an actual or intended assault or in a manner intended to intimidate or terrorise staff, patients or other persons on the practice premises
- threatened to assault or physically harm a primary care worker
- threatened to damage property or to ‘seek revenge’ in a menacing way
- caused damage to property with an intention to intimidate or cause harm
This list is not exhaustive.
What behaviour this scheme does not ordinarily cover?
7.4.11 Below are some examples of the types of behaviours that would not ordinarily fall within the scope of the regulations covered by this guidance. These are only intended to be used as a guide and therefore the list is not exhaustive. Any person felt threatened or fearful of their own safety, should still report the incident. These removal regulations cover all persons on the practice premises.
- invasion of another person’s personal space, which can be considered threatening
- shouting or banging the reception desk
7.4.12 In such circumstances, it might be more appropriate to use the standard procedure for a breakdown in practice/patient relationship, usually this is undertaken by writing to them after the event, requesting an explanation or apology and warning that a continuation of such behaviour could result in them being removed from the practice’s list. Practices may also choose to use or agree on a good behaviour contract with the patient to support their continued registration.
7.4.13 Patients must not be immediately removed for minor incidents not reported to the police.
7.4.14 Consideration should be given as to the history and circumstances of a patient including:
- wherever the behaviour can be ascribed to a condition capable of being rapidly alleviated by treatment, eg mental health illness or medical/acute conditions with known behavioural changes (eg head injury)
- whether it relates to a patient who has never been aggressive before and/or who is clearly suffering mental or physical distress
- careful consideration of any mitigating circumstances must be given as to whether a referral to the scheme is in the best interests of the patient
7.4.15 Incidents that occur outside of the primary care setting and have no connection with the practice, such as community or hospital-based incidents. These would ordinarily default to and dealt with by that specific settings policy.
a. It is important to recognise that the SAS does not usually provide for the ongoing treatment of the families of those patients allocated to the scheme for incidences which have been reported to the police and an incident number provided. A practice must not unilaterally remove all family members unless they have also behaved in a way as to require allocation to a SAS and each patient must be referred separately. On a case-by-case basis, as part of their considerations SAS providers should consider the support which may also be needed by other vulnerable dependent family members of the patient who may also need to be registered with the SAS provider and as part of safeguarding considerations. For instance, assessment of child dependants and whether the patient being diverted to SAS is the sole parental carer to take any child to their GP where:
i. the child is aged 16-18 years old, then this might not be an issue since children of this age can often consent to treatment
ii. the child is aged 14-16 years old; they may require another responsible and trusted adult to attend, including older sibling or kinship carer
iii. the child is under 14 years old then they should always have a parent, kinship carer or guardian present
Safeguarding: registering children
7.4.16 Section 11 of the Children Act 2004 places a statutory duty on the NHS to safeguard and promote the welfare of all children up to the age of 18 years. The Victoria Climbie Enquiry Report 2003 (9.104) stresses the importance of GP registration for every child. It sets out the importance of knowing the identity and name of those registering the child and their relationship to that child.
The legal definition of a child is 0 to 18 years of age; however, 16 to 18 years of age are still children by law of child protection but can also be parents and carers, therefore it is important risks and vulnerabilities within this age group are considered.
Where parents or carers have been removed from the list due to aggressive and or violent behaviour a risk assessment should be completed to identify any risk to their children and the appropriate referrals safeguarding made. Please ensure you consult relevant safeguarding procedures and record any referral decision.
In any type of patient deduction consideration must be given to any potential safeguarding concerns. Where a patient is at risk of being removed that may impact on parenting/caring capacity (eg mental health) consideration must be given to safeguarding for children or vulnerable/at risk adults. Advice should always be sought from local safeguarding leads and/or the commissioners’ designated professional.
With regards to the deduction of children (aged under 18) GP practices have the clinical expedient prerogative to retain children (under 18 years old) under the paramountcy of the child within The Children’s Act 2014, until such time that they understand how the children might be cared for by another NHS or private GP, especially if vaccines or screening are still indicated.
It should also be noted that:
- children and young people (CYP) on a protection order or protection plan should not be de-registered on the grounds of behaviour including non-attendance
- CYP (not protected) and adults with learning disabilities and/or autism, individuals with a mental health issue, or with those with a formal carer should not be de-registered on the grounds of behaviour including non-attendance
These individuals may need to be referred to safeguarding leads since they might be at risk either through behavioural problems or non-attendance of their appointments.
These individuals should be allowed to sustain their GP registration for continuity of care until such times as it can be established how the children might be cared for by another NHS or private GP.
Therefore:
- children of parents or carers, who have been removed from the list for any reason, must not be left without access to primary care service
- where parents or carers have been removed from the list due to aggressive and or violent behaviour a risk assessment should be completed to identify any risk to their children and the appropriate safeguarding referrals made Please ensure you consult relevant safeguarding procedures and record any referral decision.
A ‘think family’ approach should be made when seeing either the adult(s) or child/children within the surgery. If healthcare professionals are aware that an adult has significant risk-taking behaviour, chronic mental health concerns or repeated episodes of stress and anxiety, safeguarding and support consideration should be made to the welfare and safety of the child/children being cared for by that adult.
Refer to chapter 3: managing patient lists and chapter 4: GP patient registration standard operating principles for primary medical care for further information on safeguarding.
7.4.17 Where a breakdown in relationship had occurred with non-dependant family members as a result of one family member being placed on the SAS, then they should be removed using a more relevant process e.g. eight day removal. Refer to chapter 3: managing patient lists, section 3.2.3: removing a patient from a practice list.
Note: where a practice is unsure how to proceed having read these examples, they can contact their commissioner for support, advice and guidance. The practice may also choose to seek guidance from their local medical committee (LMC).
7.4.18 Please note that within the managing patient lists chapter there is sub section: removing a patient from a practice list which describes a route to be taken in the event of an irrevocable breakdown in GP/patient relationship, which can be the more appropriate route, however, a patient must usually be sent a warning letter within the proceeding rolling 12-month period and given the opportunity to moderate their behaviour. Removal can only normally be affected if the behaviour is repeated and then the patient can be given 8 days’ notice to find a new GP. Less serious circumstances are suitable for this method of removal by the contractor. Patients must not be removed using the ’immediate removal’ process unless the matter has resulted in the incident being reported to the police.
In circumstances where a patient displays inappropriate or unacceptable behaviour towards staff or other service users short of violence and threatening abuse (eg discrimination, harassment or victimisation) refer to chapter 6: managing [non-violent] inappropriate and unacceptable patient behaviours, including protecting against discrimination, harassment or victimisation.
7.4.19 Under the regulations, once satisfied that a patient’s behaviour warrants removal from the practice list, in order to remove a patient immediately, the practice is required to:
Notify the police
7.4.20 In order to remove a patient immediately for cases of assault, threat or damage, the incident has to be serious enough to justify reporting the incident to the police in an appropriate timeframe, due to the incident having left the person(s) feeling sufficiently threatened for their own safety, or that of another.
7.4.21 The practice, where appropriate, should dial 999 on the day of the incident and if necessary, summon police assistance/attendance. When contacting the police, it is important that the practice makes it clear that an incident has occurred, that the practice wants to make a formal statement as soon as possible, to support the immediate removal of the patient from the practice list.
7.4.22 Due to the nature of incidents requiring an immediate removal under the regulations, it would not be expected that the practice notify the police days after the incident. A further contact to the police within 7 days may be required if the incident number for the call wasn’t recorded, retained or provided at the time of the call. The SAS policy is in place for urgent incidences and as such, this information and evidence may be used for local audit purposes.
Notify the commissioner (via PCSE)
7.4.23 The practice is required to notify the commissioner via PCSE by using the online forms via the PCSE website at Contact us – Primary Care Support England as set out in 7.1: executive summary and key messages. The practice will need to confirm that prior to removing the patient from their patient list they have carefully considered patients protected characteristics and key past medical history, learning disability and neurodiversity and the practice has completed any safeguarding considerations where applicable. At this point there will be a reasonable expectation that practices will be able to evidence contact with the police by passing on details of an incident number or detail why this has not been possible. The practice will be required to follow up the call by emailing a written report of the incident (including police incident number), preferably within 24 hours but no more than 7 days after the incident occurring and via email to the commissioner. A sample reporting form for recording the incident can be found in annex 1.
7.4.24 The practice must notify the patient that it has requested their removal from the patient list, as set out in the regulations unless an exception applies.
7.4.25 PCSE will ensure the patient removal process commences. Following the removal and in conjunction with the commissioners as necessary, PCSE will decide on the best arrangement to ensure continuity in primary medical services for the patient. This may include allocation to the SAS. A flag is placed on the patient record which prevents the patient from registering at other GP practices.
7.4.26 PCSE will write to the patient to notify them of the removal and ongoing management arrangements. Refer to annex 7: standardised patient communications from PCSE. It is expected that this process will be completed within a 24-hour working period from the initial notification.
NHS England is committed to working with its partners, patients and patient representative groups to refine and improve this standardised letter further. We are also committed to making this communication available in alternative languages.
Note: following removal, all patients must be allocated to and accepted by the SAS provider commissioned by the ICB. Subsequently, all patients allocated to SAS should have an assessment of appropriateness to be accepted in the scheme by the SAS provider (subject to services being commissioned to do so where not already in place). The patient’s risk assessment should be continually reviewed and updated after each patient encounter by the SAS provider. The SAS panel will monitor ongoing appropriateness of the patient’s continued registration with the SAS and their rehabilitation. This is with a view to safely returning choice to the patient in timely way and reintegration to mainstream GP practice.
7.4.27 Registered providers and managers of NHS GP and other primary medical services must also comply with their regulatory obligations. For example, to notify CQC about certain incidents that took place “while an activity is actually being provided or as “a consequence of its being provided” (CQC, 2013) and when an incident is reported to or investigated by the police. Further information is available on the CQC website.
7.4.28 For further information relating to the process, please refer to annex 2: what happens to the patient following allocation?
7.4.29 The practice must notify the patient that it has requested their removal from the patient list, as set out in the regulations unless an exception applies.
7.5 Patient appeals process
7.5.1 The appeals process must recognise that a practice has already fulfilled its obligation under the regulations by reporting the incident to the police and notifying the commissioner.
7.5.2 Patient referred to the SAS have a right of appeal and should they wish to do so, can appeal against the decision by putting this in writing within 28 days of the notification of the referral, addressing it to the commissioner’s SAS Liaison team. The commissioner will contact the practice to notify them of the appeal and invite them to provide any supplementary information in relation to the removal.
The appeals process does not delay the immediate removal of a patient following an incident that has been reported to the police and the commissioner (via PCSE).
7.5.3 The appeal should be reviewed by a panel convened by the commissioner (a ‘SAS panel’) within 28 days of receipt of the patient’s appeal. The panel should include appropriate representations (including LMCs and if appropriate, a patient representative or patient representative group, (when requested by or agreed with the patient). Refer to annex 8: a sample terms of reference for an appeal panel.
7.5.4 It is the responsibility of the SAS panel to review the evidence provided by the patient in support of their appeal. The SAS panel will uphold or reject the appeal where it has reasonably considered if a removal under the regulations was made in error, or inappropriately.
7.5.5 Pending the outcome of any appeals process, should the patient need to access primary medical services, this would have to be provided by the SAS to which the patient had been allocated.
7.5.6 The commissioner will notify the patient of the decision in writing within 14 days of the SAS panel decision, having first discussed the outcome with the practice from which the patient was removed.
Patient appeals – additional information
7.5.7 To support appeal panels in their reaching a determination the following annexes may be useful and some sample considerations are provided below (list not exhaustive):
- Annex 3: SAS sample good conduct guide
- Annex 4: sample data sharing agreement
- Annex 5: risk assessment approach
7.5.8 The panel should be assured that:
- the identity of the removed patient and that of the patient that was involved in the incident should be confirmed as the same and be without any doubt
- where the reported incident occurred during a clinical consultation, the removed patient had an appointment at the practice on the same day
- a police incident number has been provided, either at the time of the removal or within 7 days as part of the written report
- a written report has been submitted to the commissioner (usually via PCSE). See annex 1 – patient removal request form
- the information provided in the report is consistent with the requirements for immediate removal, as set out in the GMS/PMS regulations
- the content and strength of any evidence provided by the removed patient does not wholly support their claim that they should not have been removed (eg clear and incontrovertible evidence that they were out of the country at the time of the incident or at another location, eg in-patient in a hospital)
7.5.9 The panel should also:
- invite the patient to submit any further relevant information or a statement in relation to the alleged incident. This will ensure all parties are considered to have been treated fairly and equally should the matter be escalated to the Parliamentary and Health Service Ombudsman (PHSO) or through a legal route
- seek confirmation from the GP practice, which member of staff was involved in the incident
- seek confirmation from the practice which member of staff requested the deduction
- discuss the incident with the practice
- re-confirm with the practice, the details of the patient involved in the incident and cross-check this with the details of the patient making the appeal
7.5.10 In reaching a determination the panel may conclude that the patient appeal should be upheld. In this case, the SAS flag on the patient records should be removed (by the commissioner notifying PCSE) and choice returned to the patient. This presents several options to the panel and the commissioner and will depend entirely on the reason for upholding the appeal.
7.5.11 If, for example, a case of mistaken identity is confirmed, the panel in consultation with the commissioner may (if agreed in advance with the removing GP practice) seek to return the patient to the GP practice they were removed from.
7.5.12 Return choice to the patient enabling them to choose another GP practice in the area where they live. This could be an option where the GP practice that removed the patient under the immediate removal process considers there has also been an irrevocable breakdown in relationship. Refer to chapter 3: managing patient lists.
7.5.13 In reaching a determination that the patient appeal should be rejected, the patient should remain on the SAS and be reviewed in accordance with policy.
7.5.14 In all cases the patient must be notified within 14 days of the appeal hearing; sample patient letters can be found at:
- Annex 9: sample patient letter: appeal upheld
- Annex 10: sample patient letter: appeal rejected
7.5.15 Each commissioner’s SAS panel should consider any patient appeal. The panel’s decision with regard to the removal and SAS allocation does not affect the patient’s right to escalate the matter to the Commissioner or the Parliamentary and Health Service Ombudsman (PHSO).
Note: if a patient’s appeal is upheld, the Commissioner must notify PCSE via pcse.patientremovals@nhs.net
7.5.16 The SAS allocation and appeals flow chart (annex 11 – see below) may be useful:
Annex 11: SAS allocation and appeals flow chart
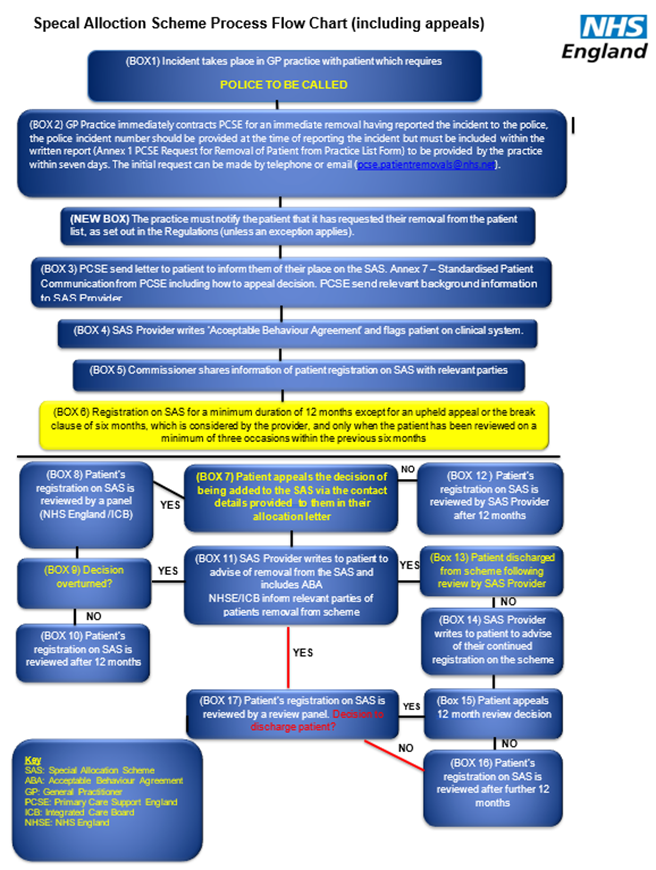
8 Contract variations (templates available)
8.1 Introduction
8.1.1 This policy describes the process to determine any contract variation, whether by mutual agreement or required by regulatory amendments, to ensure that any changes reflect and comply with legislation so as to maintain robust contracts.
8.2 Types of contract variation
8.2.1 Variations to contracts fall broadly within 4 categories:
- changes due to legislation or regulatory change
- changes to the contracting party
- changes to services
- changes to the payment arrangements
8.2.2 Where a GMS contract or PMS agreement is varied, the commissioner is required by the regulations to notify relevant patients where such variation:
- changes the range of services provided to the contractor’s registered patients; or
- where patients who are on the contractor’s list of patients are to be removed from that list
8.2.3 The commissioner must inform those patients of the steps they can take to obtain elsewhere the services in question or register elsewhere for the provision of essential services (or their equivalent).
8.2.4 The commissioner should consider whether any such provision is contained within any APMS contracts it holds.
8.3 Legislation/regulatory changes
8.3.1 Usually both parties to a primary medical contract must agree on a variation in order for it to take effect. The commissioner may, however, vary the contract without the contractor’s consent where it is reasonably satisfied that it is necessary to do so to comply with the NHS Act, any regulatory changes pursuant to the NHS Act or any direction given by the Secretary of State pursuant to the NHS Act. This right is contained within all GMS, PMS and APMS and contracts.
8.3.2 The commissioner must notify the contractor in writing of the wording of the variation and the date it will take effect. Where it is reasonably practicable to do so, the date the variation will take effect must not be less than 14 days after the notice is served.
8.3.3 There is no need for the commissioner to seek agreement or require a signature of acceptance for this type of variation, as there is no right of refusal or negotiation.
8.3.4 The process for issuing a variation notice due to legislation/regulatory changes is:
- a regulatory amendment to existing regulations or new directions are issued under statutory instrument. Commissioners should ensure arrangements are in place to take the appropriate action as quickly as possible after the issue of an amendment
- where the GMS regulations, PMS regulations and/or APMS directions are amended, there may be centrally issued GMS, PMS and APMS variation notices. These should be used to update the relevant contracts and ensure contractors are informed of the changes
- the commissioner must notify contractors of the variation and its effective date. A template variation notices are provided below in annex 1 for GMS contracts and annex 2 for PMS/APMS contracts.
- for GMS contractors, the notification should include the GMS variation and the relevant pages of the amended contract document for completeness. For PMS and APMS contractors, the commissioner will be required to ensure the regulatory amendments become a contractual amendment, citing the correct clause numbers affected within the individually held contracts and including the relevant pages of the document for completeness
- all electronically held contracts should be updated with the variations at this stage to ensure that the centrally held documents remain up to date with current legislation. Commissioners should retain a copy of the notice on file for completeness. Each contract file should contain a variation log and commissioners should ensure that this is updated accordingly
8.4 Changes to the contracting party
8.4.1 Changes to the contracting party may be due to:
- partnership changes
- company changes
- retirement (including 24-hour retirement)
- novation, mergers and splits; and/or
- death of a contractor
8.4.2 There are specific processes to follow on the death of a contractor. Please refer to the chapter on the death of a contractor for further information.
8.4.3 The GMS regulations and PMS regulations and the APMS directions contain provisions relating to the remaining scenarios listed above which are considered in more detail below.
8.5 Partnership changes
8.5.1 Changes to the composition of a partnership will require variation to the contract and may require a variation to the standard registration conditions with the CQC.
8.5.2 In some circumstances, the admittance of a new contracting party may be caught by the provisions of the PSR. Commissioners should refer to the published statutory guidance on PSR and should take appropriate advice at an early stage.
8.5.3 The GMS regulations, the PMS regulations and the APMS directions place restrictions on the organisational structures that are eligible to enter into different types of primary medical contracts. Please refer to the contracts described chapter for details on the eligibility criteria.
8.5.4 Contracts may be varied in a number of ways with relation to partnership matters, including the following which are looked at in more detail below:
- individual contractors changing to more than 1 individual (which may be a partnership which requires a different process depending on whether it is a GMS contract or not); and
- changes to the parties of contracts with more than 1 individual (which may be from a partnership to an individual contractor or changes to the composition of partnerships)
8.5.5 There may be many reasons for partnership changes including disputes between parties which are considered further below.
Individual to partnership – GMS contracts
8.5.6 If a GMS contractor is currently an individual medical practitioner who wishes to enter into partnership with one or more individuals under that contract, the contractor is required to notify the commissioner in writing and provide the following information:
- the name of the individual or individuals with whom the contractor proposes to practice in partnership
- confirmation that the individual or individuals are either a medical practitioner or a person who satisfy the conditions specified in section 86(2)(b) of the NHS Act
- confirmation that the individual or individuals satisfy the conditions imposed by regulations 4 and 5 of the GMS regulations (please refer to the contracts described chapter for further information)
- whether or not the partnership is to be a limited partnership and if so, who is a limited and who is a general partner
- the date on which the contractor wishes to change its status (which shall not be less than 28 days from the date on which the notice was served on the commissioner)
8.5.7 The notice must be signed by the individual contractor and by the individual or individuals with whom the individual contractor is proposing to practise in partnership. Where the contractor contacts the commissioner about such a change, the Commissioner should send annex 3A: request for information relating to change from individual to partnership – GMS contracts.
8.5.8 The commissioner must ensure the accuracy of the information provided. This may be achieved, for example, by checking the registration status of the proposed partner(s) and that the proposed partner(s) meet the eligibility criteria for holding a GMS contract.
8.5.9 Where the change is agreed, the commissioner will confirm in writing that the contract will continue with the partnership and issue a variation notice accordingly to amend the relevant sections of the contract. The commissioner must specify in the notice the date on which the contract will continue as a partnership. Where reasonably practicable this should be the date requested by the contractor, or the nearest date to it (annex 3B: acknowledgement of information relating to changes from individual to partnership – GMS contracts).
8.5.10 A variation notice must include the wording of the proposed variation and the date upon which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.11 If the new partner is not accepted as eligible the commissioner should advise the contractor in writing of the reasons they believe the proposed partner(s) to be ineligible and confirm that the contract status will remain with an individual medical practitioner until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible partner.
Individual to more than one individual – PMS agreement
8.5.12 The PMS regulations do not allow PMS agreements to be treated as made with a partnership. Where individuals are practising in partnership, the PMS agreement will be entered into with each person (which may or may not be in partnership). The persons comprising the signatories to the PMS agreement collectively form the contractor.
8.5.13 The PMS regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
8.5.14 If the contractor is currently an individual medical practitioner and they wish to have one or more persons join them under that agreement, then they must seek the commissioner’s consent in writing for any such variation to the contract. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 4A: request for information relating to change from individual to more than one individual – PMS contracts. The commissioner must have consideration of any provisions of the PSR that may apply, along with other influencing factors, when considering such an application. Commissioners must also act in accordance with the published statutory guidance on PSR.
8.5.15 The commissioner must ensure the proposed person(s) meet the eligibility criteria for holding a PMS agreement (please refer to the contracts described chapter for further information).
8.5.16 The commissioner should confirm its decision on the variation in writing to the contractor detailing the reasons for the decision and details of any information that they have relied upon in the process (annex 4B: acknowledgement of information relating to change from individual to more than one individual – PMS contracts).
8.5.17 If the decision is to consent to the variation, then the commissioner shall issue a variation notice accordingly to amend the relevant sections of the contract. A variation notice should include the wording of the proposed variation and the date upon which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.18 If the contractor does not return a signed copy of the variation notice, then no amendment to the agreement can take place.
8.5.19 If the new person is not accepted as eligible the commissioner should advise the contractor in writing of the reasons, they believe the proposed person(s) to be ineligible and confirm that the contract status will remain as it was until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible person.
Individual to more than one individual – APMS contract
8.5.20 APMS contracts can be entered into with a partnership and the commissioner should consider the wording of the relevant contract to determine whether there are any specific provisions covering a request from the contractor to have one or more persons join them under the contract. Where there are no such provisions, a similar process to PMS agreements could be followed.
Changes to contracts with more than one individual – GMS contracts
8.5.21 Changes to the contracting parties may occur where a partnership dissolves or terminates or where the composition of the partnership changes. Both scenarios are explained below.
8.5.22 Where a partnership is dissolved or terminated and the contractor consists of 2 or more individuals practising in partnership, the contract may continue with one of the former partners if the following conditions apply:
- the former partner must be nominated by the contractor; and
- the former partner must be a medical practitioner that meets the condition in regulation 4(2)(a) of the GMS regulations
8.5.23 The nomination of the former partner by the contractor must:
- be in writing and signed by all the individuals who are practising in partnership. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 5A: request for information relating to change from partnership to individual – GMS contracts
- specify the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- be provided to the commissioner at least 28 days in advance of the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- specify the name of the medical practitioner with whom the contract will continue, which must be one of the partners
8.5.24 Where the commissioner receives such a nomination, it must acknowledge receipt in writing before the date specified in the nomination as the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner.
8.5.25 Where the commissioner agrees the nomination, the commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date upon which that variation is to take effect.
8.5.26 A template notice is provided in annex 5B. A variation notice will need to be included with this letter.
8.5.27 The commissioner should be satisfied that the arrangements in place for continuity of service provision to the contracts’ registered patients are robust.
8.5.28 In circumstances where the commissioner is not satisfied that the nominated partner is eligible to hold the contract as an individual, they should enter into dialogue with all of the partners, to explore potential solutions.
8.5.29 These might include the partners nominating an alternative partner to continue with the contract, in which circumstances a new notice should be issued to the commissioner to include these details and propose a new date on which the changes will occur.
8.5.30 Where the contractor consists of 2 or more individuals practising in partnership and the composition of the partnership changes, either by a partner leaving (but without the partnership terminating) or a new partner joining, the contract will need to be amended to recognise the new partnership composition. For the variation to have effect, it must be in writing and signed by all parties to the contract.
Changes to contracts with more than one individual – PMS agreements
8.5.31 As stated in paragraph 8.5.13, the PMS regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
8.5.32 If the contractor is currently 2 or more persons and wish to change to an individual contractor, then they must seek the commissioner’s consent in writing for any such variation to the contract. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 6A: request for information relating to change from more than 1 individual to an individual – PMS contracts. The commissioner must consider any provisions of the PSR that might apply, along with other influencing factors, when considering such an application. Commissioners must also follow the published statutory guidance on PSR.
8.5.33 The commissioner must ensure that the proposed person(s) meets the eligibility criteria for holding a PMS agreement (please refer to the contracts described chapter for further information).
8.5.34 The commissioner should confirm its decision on the variation in writing to the contractor detailing the reasons for the decision and details of any information that they have relied upon in the process (annex 6B: acknowledgement of information relating to change from more than one individual to an individual – PMS agreements).
8.5.35 If the decision is to consent to the variation, the commissioner shall issue a variation notice accordingly to amend the relevant sections of the contract. A variation notice should include the wording of the proposed variation and the date upon which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.36 If the contractor does not return a signed copy of the variation notice, then no amendment to the agreement can take place.
8.5.37 If the new person is not accepted as eligible the commissioner should advise the contractor in writing of the reasons, they believe the person is ineligible and confirm that the contract status will remain as it was until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible person.
8.5.38 The principles outlined in paragraphs 8.5.31 to 8.5.37 will also apply where the contractor consists of 2 or more persons and the composition of the contractor changes, either by a person wishing to leave the agreement or a new person joining the agreement. The contract will need to be varied to recognise the new contractor composition.
8.5.39 The commissioner should ensure that it is satisfied that the contractor will remain eligible to hold the agreement after the variation. For the variation to have effect, it must be in writing and signed by all existing (and new) persons to the contract.
8.5.40 The commissioner should also be satisfied that the arrangements for continuity of service provision to the registered population covered within the contract are robust and may wish to seek written assurances of the post-variation contractor’s ability and capacity to fulfil the obligations of the contract and their proposals for the future of the service.
8.5.41 APMS or PMS contracts are not required to contain a right of termination where 1 or more persons have left the practice during the existence of the contract. The commissioner should review the relevant contract to determine whether any such provisions have been included.
Changes to contracts with more than one individual – APMS contracts
8.5.42 The commissioner should consider the wording of the relevant APMS contract to determine whether there are any specific provisions relating to changes to the composition of the contractor. Where there are no such provisions, a similar process to PMS agreements could be followed.
Partnership splits/members dispute – GMS and PMS
8.5.43 Where the contractor to a GMS contract is a partnership and the partnership dissolves due to an internal partnership dispute, the parties may agree for the contract to continue with 1 partner (see paragraph 8.5.22 of this policy). If the partnership dissolves and there is no agreement between all partners who will continue the contract, commissioners should refer to annex 6C: managing circumstances where partnership dissolves with no clear successor – GMS contracts for further advice.
8.5.43 It is, desirable that the partners of a GMS contract can resolve disputes internally where possible, with the support of the LMC and/or mediation services.
8.5.44 If the partnership holding a GMS contract does not dissolve or terminate but the partnership no longer wishes to be a party to the contract, then the contractor will need to terminate on notice, which must not be less than 6 months unless agreed by the commissioner. Failure to give 6 months’ notice of termination is a breach of contract and the appropriate action will be taken in line with the chapter on contract breaches, sanctions, and terminations.
8.5.45 Under PMS agreements, subject to the terms of the individual agreements, partnership matters (including dissolution or termination of the partnership) do not affect the continuation of the agreement. This is because where the agreement is with 2 or more persons that are practising in partnership, the agreement is not entered into with the partnership but instead with those persons (who collectively make up the contractor).
8.5.46 If a PMS contractor is practising in partnership and, following termination of a partnership, the contractor no longer wishes to be a party to the contract, the contractor will need to give notice to terminate the contract, such notice being a minimum of 6 months unless agreed with the contractor.
8.5.47 Where partnerships or membership are formalised through a partnership agreement, it is very helpful if the parties are able to rely on the detail of these agreements to support the early resolution of internal disputes and to ensure that such agreements are reviewed and maintained to be current with associated legislation.
8.5.48 Unfortunately, many partnership organisations do not have agreements in place or have insufficient or outdated documents which can often lead to very protracted and acrimonious disputes between the partners.
8.5.49 The commissioner should not get involved in endeavouring to resolve the dispute between the partners, instead insisting that the parties notify the commissioner of their final decision when it is reached.
8.5.50 It is likely that the commissioner will have numerous contacts from different partners and their staff about the dispute, but the commissioner should try to maintain a detached position in this respect. Any accusations of inappropriate behaviour or concerns should be considered; however, this should not be used as a means to endeavour to resolve the dispute.
8.5.51 Throughout the dispute the commissioners should maintain open dialogue with the LMC and implement contract performance management protocols if and when necessary.
8.6 Retirement of a contractor – single handed
8.6.1 There is no specific reference to retirement in the GMS regulations, the PMS regulations, or the APMS directions. The commissioner should deal with a request to retire as a request to terminate the contract by the contractor on notice.
8.6.2 The contractor must provide the commissioner with a written notification of the intended retirement date which will be the termination date of the contract. This notice period must not be less than 3 months for GMS contracts held by an individual medical practitioner or less than 6 months for GMS contracts that are not held by an individual and for PMS/APMS contracts.
8.6.3 For GMS contracts, if the termination date is not the last calendar day of a month, the contract shall instead terminate on the last calendar day of the month in which the termination date falls.
8.6.4 For PMS/APMS contracts, there is no such requirement. The commissioner must calculate the date of termination, based on the terms in the individual contract and from the date of the notice.
8.6.5 In exceptional circumstances, such as ill health, the commissioner may wish to waive its right to the full notice period, but it remains its right alone to do so. Consideration should be given, amongst other matters, to the effect that holding a contractor who is unwell to the full notice term may have on the contractor, the practice’s patients, and colleagues.
8.6.6 In either case the commissioner should confirm receipt and acceptance of the retirement/termination notice in writing, the date on which the contract will terminate and any consequences and actions that the contractor must take as a result of the notice.
8.6.7 Although not required by the GMS regulations, the Standard GMS Contract clearly sets out the arrangements that must be made on termination of a contract, which include (but are not limited to) the contractor having to:
- cease performing any work or carrying out any obligations under the contract
- co-operate with the commissioner to enable any outstanding matters under the contract to be dealt with or concluded satisfactorily
- co-operate with the commissioner to enable the contractor’s patients to be transferred to 1 or more other contractors or providers of essential services (or their equivalent)
- deliver up to the commissioner all property belonging to NHS including all documents, forms, computer hardware and software, drugs, appliances or medical equipment which may be in the contractor’s possession or control
8.6.8 The commissioner shall have in place arrangements for collecting any property owned by the NHS on or immediately after the termination date, which should be included on a log of collection, and against any the commissioner held asset list, and where possible the contractor should be asked to sign to confirm the property that has been removed, accepting that it is owned by the NHS.
8.6.9 On termination of the contract, the commissioner shall perform a reconciliation of the payments made by the commissioner to the contractor and the value of the work undertaken by the contractor under the contract. The commissioner must then serve the contractor with written details of the reconciliation as soon as reasonably practicable, and in any event no later than 28 days after the termination of the contract.
8.6.10 Each party shall pay the other any monies due within 3 months of the date on which the commissioner served the contractor with written details of the reconciliation, or the conclusion of any NHS dispute resolution procedure, or court action as appropriate as the case may be.
8.6.11 PMS/APMS contracts must make suitable provision for arrangements on termination, including the consequences (whether financial or otherwise) of the contract ending, subject to any specific requirements in the regulations. While these terms are likely to mirror those set out in GMS contracts, the individual contracts must be checked by the commissioner to ensure that no additional or alternative terms were included. This is especially important when considering termination of an APMS contract, which may include very specific additional terms in this respect.
8.6.12 The key elements for consideration leading up to a termination remain the same in respect of patients, property and transfer of records and confidential information.
8.6.13 For a list of considerations relating to termination, please refer to the chapter on contract breaches, sanctions and terminations.
8.7 Retirement of a contractor – two or more partners/individuals
8.7.1 Where a partner wishes to retire from a GMS partnership, as constituted from time to time, the contractor will need to notify the commissioner that it wishes to vary the contract. The commissioner should follow the process in paragraphs 8.5.21 to 8.5.30 of this policy.
8.7.2 Where an individual wishes to retire from a PMS agreement, where that agreement is also held by one of more persons, the contractor will need to notify the commissioner that it wishes to vary the agreement. The commissioner should follow the process in paragraphs 8.5.31 to 8.5.40 of this policy.
8.7.3 Where a partner of a partnership holding an APMS contract wishes to retire, the commissioner should follow any process defined within the contract, or in the absence of any defined process, the consent of the commissioner must be sought through a contract variation.
8.7.4 The commissioner should always keep in mind the provisions of the PSR and consult the published statutory guidance on PSR when applying the guidance in this policy.
8.7.5 Any changes to the partners within a contract may require a new registration with the CQC.
8.8 24-hour retirement
8.8.1 24-hour retirement is a process by which members of the NHS pension scheme seek to qualify for their retirement benefits whilst continuing to work (albeit with a break).
8.8.2 24-hour retirement usually involves resigning from all involvement in an NHS contract, not returning to the NHS in any capacity for at least 24 hours and not working for more than 16 hours a week in the first month of retirement. The commissioner should ensure that it is aware of the current conditions around 24-hour retirement.
8.8.3 If the commissioner is approached by a contractor wishing to take 24-hour retirement, it must not offer advice relating to pension arrangements.
8.8.4 Where a contractor confirms that 24-hour retirement requires ‘resignation’ from the contract, steps will need to be taken to ensure that the contractor is removed from the contract, either by:
- termination on notice in the case of a single-handed contractor; or
- variation of the contracting party in the case of a partnership
8.8.5 The commissioner may wish to suggest single-handed practitioners take independent advice, as 24-hour retirement using the method described above would necessitate the termination of the contract as set out in paragraphs 8.6.1 to 8.6.13.
8.8.6 The commissioner must make clear to the contractor that there is no guarantee that the commissioner would commission services from that individual following termination.
8.8.7 Commissioners should defer to the published statutory guidance on PSR to consider the provisions that may apply and should seek legal advice locally as appropriate.
8.9 Variation provisions specific to a contract with a company limited by shares (GMS) or a qualifying body (PMS)
8.9.1 A GMS contract may be held by a company limited by shares (subject to certain conditions). PMS agreements may be held by a qualifying body (a company limited by shares, all of which are legally and beneficially owned by persons who may enter into a PMS agreement).
8.9.2 APMS contracts, in principle, have fewer restrictions on the types of organisations that may enter into the contracts and therefore the commissioner can enter into APMS contracts with any individual or organisation that meets the provider conditions detailed in the APMS directions.
8.9.3 For further information on what types of organisations can enter into the different types of contracts (please refer to the contracts described chapter for further information).
8.10 Contracts and incorporation/dis-incorporation
8.10.1 It is possible for individual GPs or partnerships holding a GMS, PMS or APMS contract to seek commissioner approval to operate and deliver services through a company limited by shares (called a ‘qualifying body’ in PMS) – this process is known as ‘incorporation’. A change from a single-handed or partnership contract to a limited company is a complete change of the identity of the contracting party, regardless of whether the company is owned and/or run by the original contractors.
8.10.2 Dis-incorporation is the same process in reverse.
8.10.3 There is no right for a contractor to incorporate or dis-incorporate. They need agreement from the commissioner, which does not have to be given. In reaching their approval or rejection decision, a commissioner should consider carefully the proposal including assessing the application for its benefits, for example to patients, but also the opportunities including strategic alignment with local priorities to transform services and improve care quality. A commissioner should also consider the risks.
8.10.4 There are a range of incorporation scenarios that commissioners may be asked to consider. The most straightforward scenario is a request for the existing individual contractor(s) to form a company and continue to run the business themselves as the shareholders and directors of that company (or vice versa on dis-incorporation). There are also scenarios that might seek to change the nature of the contractor:
- a request to form or become part of a company in which one or more existing contractor(s) will hold some shares but they may not have overall control of that company – this should be carefully assessed against the provisions of the PSR as risks may apply. Other risks may also be identified); and
- a request to transfer the contract to an existing or new company controlled by completely separate third parties in which the existing contractor(s) hold no interest – this is a request to transfer the contract to an apparently completely unrelated third party and should be carefully assessed against the provisions of the PSR. Other risks may also be identified
Note: in scenarios that include a plan to merge practices there are a further set of considerations as set out in paragraph 8.11.
8.10.5 A commissioner may conclude that a proposal, and the associated benefits, is worth supporting provided that there is alignment with local strategic priorities and identified risk can be mitigated and/or minimised. If so, the contract will need to transfer from the old to the new contractor. A legal document called a novation agreement is used – its primary function is to change the parties to the contract. In practice, it ends the contractual relationship between the commissioner and old contractor and creates a contractual relationship between the commissioner and new contractor. The agreement must be signed by each of the 3 parties. (To note: signing a novation agreement counts as the award of a new contract – as such there may be implications in applying the provisions of the PSR. Commissioners should defer to the published statutory guidance on PSR and should seek legal advice locally as appropriate. A contract variation cannot be used in place of a novation agreement.
8.10.6 The novation agreement can also capture what has been agreed at the point of novation including the nature of any controls, including pre-conditions to be satisfied, that have been placed upon the contractor. Likely to require legal advice, any such provisions can be added to the template novation agreement (see 8.10.33).
8.10.7 In some incorporation scenarios, it may involve a contractor selling its business and as part of the sale it is transferring its contracts, including its list of registered patients, to the buyer. In the event the request is approved, and the contract is novated, the buyer is agreeing to take over the seller’s responsibilities for performing the contract, along with any associated debts and obligations.
8.10.8 It is anticipated that GP practices operating on a PCN footprint may seek to incorporate. The drivers for this may include strengthening their collaboration with their PCN partners to deliver primary medical services, the ‘network’ contract, and potentially other locally commissioned services.
8.10.9 Scenarios involving ‘at scale’ providers of primary medical services would create systemically important companies if those requests are approved.
Incorporation toolkit
8.10.10 To support effective decision making in these scenarios, NHS England has, in collaboration with regional and local commissioning colleagues, co-developed a toolkit that includes a standardised approach for assessing the requirements and considerations set out in this chapter. The toolkit includes:
- a standardised assessment framework to support commissioner decision making processes
- a supporting guidance document to help commissioners apply the framework and consider essential checks and risk mitigations including for the ‘at scale’ provider of primary medical services scenarios. At scale in this context can be defined in a number of ways: a) by the size of the population served, for example, on PCN footprint, b) by the number of contracts held and c) by the extent to which they operate across multiple commissioner areas. Only 1 of these needs to be present but, in some cases, one or more may be present
- an application template for providers aligned to this framework
- an example due diligence procedure that commissioners can adapt and tailor according to local arrangements
8.10.11 The objective of that toolkit is to support commissioners to:
- undertake their due diligence in a structured and consistent way including a standardised approach for assessing the requirements and considerations set out in this chapter
- reach an approval or rejection decision based on assessed levels of risk
- apply approval conditions as necessary to mitigate identified risks and issues
8.10.12 The assessment framework has been designed to be comprehensive in scope and to support commissioners to assess all incorporation scenarios. The framework should be applied in full when assessing ‘complex’ or novel incorporation proposals, for example, those involving ‘at scale’ providers of primary medical services. For more straightforward incorporation applications, commissioners should use their discretion as to whether the assessment framework should be applied in full. For all applications, commissioners should be able to audit and justify their approval or rejection decision.
8.10.14 The toolkit is intended to supplement, not replace, the considerations and guidance set out further in the remainder of this chapter.
Toolkit annexes
- Annex 1: the common assessment framework for incorporation requests: support and guide
- Annex 2: acknowledgement of requests to incorporate and incorporation application – template and guide
- Annex 3: assessment framework
Procurement considerations
Please note: now that PSR has been published, this section should be read in tandem with the statutory guidance.
8.10.15 Managing a request for incorporation or dis-incorporation
8.10.16 On receipt of a request from a contractor to incorporate or dis-incorporate, the process below should be followed:
- the commissioner should acknowledge the request and send the contractor an assessment template. A letter and the assessment template for incorporation are provided in annex 7 with a form for internal commissioner use provided in annex 8. A letter and assessment template for dis-incorporation is provided in annex 9
- the commissioner should make the contractor aware of the potential implications of the incorporation or dis-incorporation
- on receipt of the information, the commissioner should review the application using the toolkit and decide whether or not to agree the request
8.10.17 The commissioner should first consider whether the proposed new contractor is eligible to enter into the contract. If it is not eligible, the commissioner must refuse the request. A template letter of refusal of a request to incorporate is provided in annex 10 and in respect of dis-incorporation in annex 11.
8.10.18 Where the proposed contractor is eligible, the commissioner should undertake further essential checks (including that they are satisfying their own statutory duties) and undertake a risk-based assessment when assessing any request.
8.10.19 These matters are outlined further in this section and detailed in the incorporation toolkit. In considering these matters, the Commissioner is required to act reasonably and in accordance with public law principles. Matter to consider include:
- the commissioner’s obligations under the provisions of the PSR and compliance with published statutory guidance to determine whether there is a risk of challenge in agreeing the request and whether a competitive tender process should be carried out to select any new contractor (see also procurement section above)
- the effect of the proposal on the statutory duties of NHS England, particularly the involvement duty under section 13Q (note: in the coming months, supplementary information and guidance will be will be made available to commissioners in the form of frequently asked questions) of the NHS Act 2006 (although this is not usually triggered by a change solely to the identity of the contractor), duty under section 13K (duty to promote innovation) and section 13P (duty as respects variation in provision of health services) (see chapter 4: general duties)
- the value of the contract – both in terms of whether it represents value for money and whether it would a contract of interest to others
- the likely level of market interest in the contract
- the potential for innovation
- the need to protect services in the core contract – commissioners should ensure that if novation goes ahead, it will not result in any reduction in services to patients
- whether the commissioner is satisfied that there will be continuity of patient care
- the extent to which the original contractor(s) will be controlling and giving instructions to the proposed contractor to comply with contractual obligations
- the extent of change to the terms of the existing contract (eg contract value or services) – this is important in assessing both the provisions of the PSR (see procurement section above) and whether there is a service change requiring patient and public involvement
- payments under the existing contract and value for money
- benefits to patients of the proposal – these should be outlined by the contractor and, as a minimum, there should be no detrimental impact on patients or reduction in services
- opening hours (including evening and weekend) required – note that any reduction may trigger the patient and public involvement duty (see general duties, section 13Q) and in any case, is unlikely to be acceptable unless there are exceptional reasons justifying such a change
- sustainability – the commissioner should be assured that the proposed novation will ensure ongoing sustainability of the practice and patient services in the area going forward
- any impact on patient choice
- whether the commissioner requires that the existing contractor guarantees the performance of the proposed contractor (for example, this may be appropriate where on incorporation the new company will not have any assets) – any such requirement must be proportionate to the risks associated with the novation and reasonable with a clear rationale for placing such a responsibility on the existing contractor – legal advice should be sought
- whether the commissioner has any concerns about the proposed contractor’s financial standing and financial stability – serious concerns are likely to suggest they are unsuitable as a contractor, whereas minor concerns could for example be a factor in deciding to seek a guarantee
- whether the commissioner is satisfied with the proposed contractor’s plans for managing and operating the practice, including any proposed changes from current arrangements
8.10.20 Whether the proposed contractor is a company:
- but is not registered with Companies House (the contractor may take the view that this cannot be finalised until agreement in principle has been given by the commissioner)
- and any director of the company has been disqualified from another registered company (check Insolvency Website and Companies House Disqualified Directors)
8.10.21 An unsatisfactory Disclosure and Barring Scheme.
8.10.22 Whether the existing contractor has outstanding debts and whether novation is made conditional on repayment being made.
8.10.23 Whether the existing contractor has received any breach or remedial notices or contract sanctions and whether novation is made conditional on the proposed contractor taking on the consequences of the notices, eg action the remedial activity; and/or
8.10.24 Whether the existing contractor has outstanding issues regarding CQC inspection or practice inspection by the commissioner and whether the novation should be made conditional on those issues being resolved – or in some circumstances it may not be appropriate to agree to a novation until those issues are resolved.
Making a decision
8.10.25 Each of the above factors, along with any other relevant information about the particular request, should be carefully considered in deciding whether or not the commissioner will consent to the incorporation or dis-incorporation request. If there are concerns about the level of risk of challenge, legal advice should be sought.
8.10.26 Requests for incorporation or dis-incorporation should be agreed with or without conditions unless there are concerns that the request will not benefit patients or will create a significant risk of successful legal challenge.
8.10.27 In practice, if the commissioner does not agree to novate the contract, the existing contractor may decide not to incorporate/dis-incorporate but to keep the existing contract in place. Where this happens, there will be no new contract to arrange.
Agreeing the request
8.10.28 Where the commissioner agrees the request, the original contract will be novated. A template letter is provided in annex 12 and a template novation agreement in annex 17.
8.10.29 As a contract novation is technically termination of the original contract and replacing it with a new contract, the commissioner must make appropriate arrangements for termination of the contractual relationship with the outgoing contractor including:
- carrying out a financial reconciliation; and
- any other requirements in the contract relating to termination
8.10.30 The novation process, and the discretion commissioners have in approving the request, provides an opportunity for commissioners to negotiate and agree a range of controls with the contractor. Those controls can take the following forms (these are not mutually exclusive):
- contractual requirements: there is some, although limited, scope to agree local contract variations that would bind contractors into a course of action and be enforceable using the core contractual levers
- non-contractual requirements: these are declarative statements of intent that describe expected behaviours and/or actions but are not enforceable through the core contract
8.10.31 There are opportunities and limitations in implementing both type of controls. The supporting guidance that forms part of the toolkit set out further advice on how the contract novation process can be used by the commissioner to address identified risks and issues should they wish to approve the request.
8.10.32 Contractual requirements are the most binding form of control that can be placed on a contractor. They must be agreed between, and signed by, both parties in line with local contractual variation processes.
8.10.33 As the contractor has to agree to them, negotiating local contract variations at the same time as considering novation puts the commissioner in a good negotiating position. The value of documenting them in the novation agreement is to confirm and emphasise what has been agreed contractually at the point of novation.
8.10.34 However, there are rigid national rules and processes governing the core GP (GMS/PMS) contractual framework that limit the scale and nature of what local contractual variations are implementable outside of the national requirements (which cannot be changed).
8.10.35 The nature of what is permissible when seeking to vary the contract needs to be considered on a case-by-case basis. In summary, the following broad principles act as parameters as to what might be suitable:
- variations are targeted, proportionate, and can be justified on reasonable grounds – these can be linked to either contractor performance, their capabilities and contractual management arrangements
8.10.36 Variations must not seek to alter or extend the agreed core GMS service provision requirements – these are negotiated nationally with the BMA and are reflected in the relevant GMS/PMS contract regulations and statement of financial entitlements (SFE).
8.10.37 There are a practical set of local contract variations that are pre-cautionary, support provider sustainability and can help mitigate for the occurrence and consequences of provider failure in line with good practice. For example, as the new contractor will be a body corporate, it will be appropriate to require that the new contract contains a change of control clause. Such a clause requires the contractor to notify the commissioner where there is a change in ownership or control of the contractor and can include a requirement to obtain the commissioner’s consent. If the commissioner does not consent to the change but the contractor proceeds anyway, the commissioner may issue a remedial notice.
8.10.38 The supporting guidance that forms part of the toolkit describes the different types of controls in more detail including the circumstances in which they might apply.
Commencement of the new contract must be made conditional on the new contractor being CQC registered. The CQC cannot provide the notification of decision until the date of commencement is agreed. The contractor should, however, provide the commissioner with written confirmation from the CQC that the CQC does not intend to impose any restrictions on registration of the new contractor.
Disputes
8.10.39 Where the contractor does not agree with the commissioner’s decision, the contractor may appeal the decision. Please refer to the chapter on managing disputes for further information.
Payment system requirements
8.10.40 Following the commissioner’s decision, any changes to the contracts must be made on the relevant payment and contract management systems.
8.11 Practice mergers and/or contractual mergers
Please note: Now that PSR has been published, this section should be read in tandem with the statutory guidance.
8.11.1 A GP or partnership may hold more than 1 form of primary care contract with a commissioner. For example, a GMS contractor can also be a party under a PMS agreement and vice versa and/or a company may, for example, hold several GMS contracts.
8.11.2 This flexibility has enabled GP practices to come together in varying ways to provide support for each other, expand on the services available and/or resolve premises issues and achieve economies of scale, though each will have their own reasons for coming together.
8.11.3 The overarching issues for the commissioner to consider when any such proposal is made are the benefits to patients and the financial implications of the practice merger.
Note: where a proposed merger involves one or more dispensing practices, contract managers should also refer to the Pharmacy manual.
Note: When considering a proposed merger that involves practices spanning multiple ICB boundaries, commissioners should continue to follow this guidance. A GP practice merger across ICB boundaries will not automatically trigger an ICB boundary change. However, if patient flows are likely to be significantly affected and commissioners wish to explore the possibility of requesting a change, they should refer to ICS boundary changes and mergers procedure.
Practice merger models
8.11.4 There are many ways in which practices may seek to come together. The most common are listed below but commissioners should recognise that a proposed practice merger may fall into 1 or more of the models below or may propose a different approach:
- Model 1: GP providers agree loose arrangements such as sharing back-office functions or management staff or may even create a new legal entity to manage and oversee the delivery of services under the GP contracts. This is not a formal merger and the contracts with the commissioner will not change (this model is often referred to as a contractual joint venture).
- Model 2: The GP partners from practice A may join the partnership of practice B and vice versa. The new partnership may continue to hold the 2 separate contracts but will have merged at an operational level.
- Model 3: GP partners from practice A join the partnership of practice B and practice A ceases trading. The commissioner terminates practice A’s contract and varies practice B’s contract to include the services originally provided by practice A. This may happen with more than 2 practices so that the larger partnership holds one larger contract for services originally provided by several practices under separate contracts. The parties are likely to enter into a business transfer agreement for the transfer of assets and staff.
- Model 4: GP providers come together to create a new legal entity (eg, the GP partners become shareholders of a new company limited by shares). This may involve:
- novating the existing GP contracts to the new entity (see also 8.10 [incorporation])
- terminating the majority of the existing GP contracts and varying one to include all existing services; or
- terminating the existing GP contracts and directly awarding a new contract to the new entity.
8.11.5 Practice mergers can be complex matters which should not be approached lightly by either the contractors or the commissioner. Where a practice merger requires amendments to the practice contracts, the final commissioning decision on whether contracts should be amended to effect the proposed merger, lies with the commissioner. The commissioner does not have to agree to change the existing contracts and there are a number of important issues that would need to be considered, prior to giving consent. An overview of the potential issues is set out below. This is by no means an exhaustive list and the commissioner should refer to and seek appropriate guidance in each case to ensure that all relevant matters are considered. Some of the factors set out in 8.10 in deciding on whether to agree to a novation are likely to be relevant here too, so please refer to that section for more information.
Benefits to patients
8.11.6 The commissioner should consider the following matters in relation to the effect of the proposed practice merger on patients:
- how patients would access a single service
- what would the practice boundary be (inner and outer)
- assurances that all patients will access a single service with consistency across provision, ie home visits, booking appointments, essential and minor surgery, opening hours, extended hours, and so on, single IT and phone system
- premises arrangements and accessibility of those premises to patients
- proposed arrangements for involving the patients about the proposed changes, communicating the change to patients and ensuring patient choice throughout
- the impact on patient choice
- how the proposed merger is intended to benefit patients
Costs/value for money
8.11.7 A contract merger is likely to merge two contracts with differing values, this would have an ‘averaging’ effect, possibly resulting in a higher cost per head of population under a single contract than the commissioner would have expected. For example:
- practice A attracts £120 per patient with a list size is 1,400
- practice B attracts only £90 per patient but has a list size of 5,000
- practice A’s contract value by registered population = £168,000
- practice B’s contract value by registered population = £450,000
- total cost to the commissioner = £618,000
- a merger would result in a list size of 6,400 patients and as result the per patient cost would require renegotiation. From a procurement perspective, the commissioner should not usually enter into a new contract at a higher value than that covering the existing contracts
8.11.8 There may be other financial arrangements that need to be considered including but not limited to:
- the impact of directions under the statement of financial entitlements, or any specific terms included in the individual contracts
- QOF – merging contracts midway through a financial year in respect of QOF achievements and payments is enormously complex and requires significant safeguards to be built in to ensure there is no duplication of payments at year-end. There will also be an averaging of the arrangements and achievements in this respect too. For example:
- practice A has always achieved highly against each indicator of QOF
- practice B has struggled to meet the criteria under several of the indicators
- the results of a merger might be a single practice with mediocre achievement against aspirations and this would affect the aspirational payment that the single contract would attract; and
- premises reimbursements
General duties of NHS England
8.11.9 The general duties of NHS England/the commissioner are likely to be relevant to a decision by the commissioner to approve a practice merger that results in changes to the way services are delivered.
8.11.10 As set out in chapter 4 on NHS England’s general duties, section 13Q of the NHS Act 2006 requires NHS England to make arrangements to involve the public in the commissioning of services (see the box at the end of this section in relation to commissioner duties). The requirements are triggered if there are proposals that mean that patients would experience a change to the range of services available or the manner in which they are delivered (eg if a practice is closed following a practice merger).
8.11.11 As set out in the chapter on NHS England’s general duties, NHS England has published guidance on section 13Q in the form of ‘The statement of arrangements and guidance on patient and public participation in commissioning’ (the ‘statement’).
8.11.12 The statement sets out that a change in the GP delivering the service is not usually enough to trigger the duty, but that care must be taken if a change in personnel makes services less accessible to patient groups (eg because patients wish to be treated by someone of the same religion and gender as them). Where a practice merger may result in a change of the personnel delivering the service, the commissioner should be alert to this.
8.11.13 In practice, what will be sufficient in terms of patient involvement is very context specific. The extent of the patient engagement activities required will depend on a number of factors including the extent of the impact any changes will have. As a general rule, the greater the extent of changes and number of people affected, the greater the level of activity that is likely to be necessary to achieve an appropriate level of public involvement.
8.11.14 Generally speaking, to meet the section 13Q duty, involvement needs to apply to and inform the whole decision-making process, but this does not mean that patients need to be actively involved at every moment. Provided involvement is suitably built into the overall process, its timing can be arranged at stages to suit the commissioner’s decision-making processes. In particular, it is not necessary to involve patients immediately at the outset of any planning/consideration/decision making process in relation to any proposals of the commissioning of new services, provided patient involvement is planned for some early stage in the process. The plans for patient involvement should be clearly documented from the outset and the commissioner should consider liaising with patient representative groups, such as local healthwatch or the practices’ patient participation group.
8.11.15 The timing of public involvement is again a matter of broad discretion for the commissioner. However, any involvement should be meaningful. As such, the commissioner should involve patients at the time proposals are developed and considered. Overall, it is helpful to bear in mind the ‘gunning’ principles (these are used to judge whether or not a consultation exercise has been ‘fair’ but are useful when making arrangements for patient and public involvement), as follows:
8.11.16 Involvement should take place when the proposal is still at a formative stage.
8.11.17 Sufficient information regarding the proposals should be provided, to allow meaningful involvement.
8.11.18 Adequate time should be given for consideration of the information provided and for response.
8.11.19 The product of the involvement should be conscientiously taken into account by the decision-maker.
8.11.20 Separately, bearing in mind the commissioner’s equalities responsibilities, the commissioner should consider carrying out an equality impact assessment, to check whether any specific groups of people require specific or enhanced forms of involvement.
Procurement
Please note: now that PSR has been published, this section should be read in tandem with the statutory guidance.
8.11.21 Practice mergers often require the commissioner to either:
- mutually agree the termination of existing contracts and directly award a new contract to a new legal entity; or
- terminate existing contracts and then significantly vary one contract to add all of the terminated services
8.11.22 The commissioner’s consent is required to vary any terms (eg the services, performance standards or pricing etc.) of any GP contract.
8.11.23 Statutory guidance on the provisions of the PSR are clear mergers may involve major modifications to contracts and ICBs may need to decide whether to continue with an existing contract or to create a new contract. Mergers that result in the same services continuing, albeit with different groups or individuals, under 1 of the previously existing contracts, may be a permitted modification under the regime. However, mergers that result in material modifications to the contract, such as a material change to the services, require a new contract to be awarded. The most suitable provider process or the competitive process must be applied because the relevant authority is in effect commissioning a new service.
Other matters
8.11.24 This may include but is not limited to the effect of the practice merger on:
- the provision and/or contracting out of minor surgery, enhanced and locally commissioned services; and
- out of hours opt-outs
Mergers generally
8.11.25 In general terms contractual mergers should only be considered in cases of like-for-like contracts, ie GMS with GMS and PMS with PMS because of the differences in terms and financial arrangements. However, this does not remove the ability of a PMS provider to request to merge its business with a GMS provider and eventually work under one form of contractual terms.
8.11.26 Commissioners should advise contractors to seek guidance from their representative bodies in this instance to ensure they follow due process and are fully aware of the implications.
8.11.27 It is essential that patients from the terminating contract are included under the remaining contract through bulk transfer where possible to avoid additional cost pressure.
8.11.28 The commissioner must bear in mind that even avoiding this additional cost, once patients are under the new contract, the Carr-Hill formula will be applied and may even then increase the cost of the transferring patients based on one of the other factors, such as rurality, when it may not have applied to the terminating contract.
8.11.29 The Carr-Hill allocation formula is used to adjust the global sum payment for a number of local demographic and other factors, which may affect a practice workload. For example, a practice with a large number of elderly patients may have a higher workload than one that primarily cares for commuters.
8.11.30 The factors included in the Carr-Hill formula are:
- patient age and gender (used to reflect frequency of home and surgery visits)
- additional needs: standardised mortality ratio and standardised long-standing Illness for patients under the age of 65 years
- number of newly registered patients (generate 40% of work in first year)
- rurality
- costs of living in some geographical areas
- patient age/gender for nursing/residential consultations
8.11.31 The commissioner may request that practices proposing to merge collectively submit a business case (a sample business case is provided in annex 12A) which the commissioner can use to base its decisions on whether to approve the merger and the consequential contract variations. A template mobilisation plan for practices to tailor and submit with their business case is provided in annex 12B.
Annex 12A – template business case for practice merger
8.11.32 The Commissioner will need to amend the template business case to ensure it requests all the relevant information in respect of the merger. The Commissioner should therefore seek to engage with the practices early in the development process to shape the business case and to liaise with the practices on any amendments or updates to the business case to enable the business case to be as comprehensive as possible prior to the Commissioner making its decision.
‘Super-practices’
8.11.33 Some mergers involve the creation of so-called ‘super-practices’. Where such a merger is approved by the commissioner in accordance with this chapter 8.11, it may be that the merger is bringing together the partners of multiple practices by adding them as partners to each other’s existing contracts. This will result in a large group of partners holding a number of primary medical contracts. For this specific scenario, and provided that partners are only being added (with none leaving any of the contracts), commissioners may use the super-practice template variation agreement. This allows the various partners to sign a single document so as to affect the addition of all of the partners to all of the contracts. It can also be used to designate a small number of the partners as authorised signatories in relation to contractual matters going forward. The document is not for use in any other scenario.
8.11.34 In addition, this variation agreement includes agreement for future changes to the partnership to take effect via a single notification to the commissioner for all of the contracts. This applies only where the simplified variation agreement for super-practices is used and in all other cases a change of partners must be dealt with in accordance with section 7.5 of this Primary medical services policy and guidance manual.
8.11.35 The simplified super-practice template variation agreement [annex 16] is only for use where multiple contracts will be held by a partnership. Whilst there is no definition or criteria of a super-practice/partnership, to avoid inappropriate use, NHS England require that this variation agreement should only be used where a super-partnership is being formed, usually to cover a large geographical area and registered patient population (minimum 30,000), a minimum of 3 contracts (at least 1 must be GMS) and at least 10 – partners. For the avoidance of doubt this variation agreement should not be used for example, when merging 2 PMS contracts, regardless of the number of partners.
Delegated commissioning arrangements
An ICB that has delegated commissioning arrangements will have entered into a delegation agreement with NHS England setting out the scope of those arrangements.
The delegation agreement includes a section on approving GP practice mergers and closures. When carrying out such actions, the ICB is required to act in accordance with the delegation agreement which includes but is not limited to:
- undertaking all necessary consultation when taking any decision in relation to GP practice mergers or GP practice closures, including those set out under section 14Z2 of the NHS Act (duty for public involvement and consultation). The consultation undertaken must be appropriate and proportionate in the circumstances and should include consulting with the LMC
- prior to making any decision, clearly demonstrating the grounds for such a decision and fully considering any impact on the GP practice’s registered population and that of surrounding practices. The ICB must be able to clearly demonstrate that it has considered other options and has entered dialogue with the GP contractor as to how any closure or merger will be managed; and
- in making any decisions, taking account of the ICB’s obligations as set out in the delegation agreement in relation to procurement, where applicable
8.12 Changes to services
8.12.1 Commissioners will need to consider changes to local service provision as a consequence of a health needs assessment of the local community with particular regard to the diverse nature of the community and reducing health inequalities in access and outcomes.
8.12.2 The commissioner and the contractor shall only agree to any change to the delivery of services after all legal obligations in respect of consultation, engagement or involvement of the public, patients and other organisations have been fulfilled.
8.12.3 The paragraphs below outline the principles and steps required to process the most commonly occurring service changes.
8.13 Open and closed lists
8.13.1 There are circumstances where a contractor may wish to close their list to new registrations, eg internal capacity issues or premises refurbishments. A contractor may also seek to extend a closed list period or open their list again before the end of an agreed period.
8.13.2 Further details on how to manage patient lists are set out in the chapter on managing patient lists.
8.14 Boundary changes
8.14.1 There may be circumstances when a contractor wishes to change their main practice boundary to either expand or contract the practice area for new registrations due to new redevelopment, local authority compulsory purchase schemes and/or road developments.
8.14.2 Most practices will also have within their contracts a defined outer boundary to allow those patients, who move home a relatively short distance outside of the main boundary and who would prefer to stay with their existing practice with whom they may have a well-established relationship, to remain registered.
8.14.3 For the purposes of service provision, the full range of contractual services must be made available to those patients registered with the practice within the outer boundary and the outer boundary area must be treated as part of the practice’s contracted area.
8.14.4 Any changes to the practice area (main and outer boundary) must be considered a variation to the contract and the definitions of these areas amended under a variation notice. The contractor must notify the commissioner of its intent to vary its area in writing setting out the reasons for the change and full details of the proposed practice area, with any additional supporting evidence that may assist the commissioner in reaching its decision (a template application notice is set out in annex 13A).
8.14.5 The contractor and the commissioner must engage in open dialogue concerning the circumstances that have led to the request to change their boundary and discuss the possible implications of the action, ie a reducing patient register, an expanding patient register, the financial implications of both and any possible alternative actions that may be taken by either party to enable the practice to maintain its existing practice area.
8.14.6 Commissioners must consider the application having regard to other practices’ boundaries, patient access to other local services and other health service coverage within a location and may seek to involve the public to seek their views.
8.14.7 Once a decision is reached on whether to accept or reject the application, the commissioner should notify the contractor of its decision in writing (a template letter is provided in annex 13B).
8.14.8 If the commissioner accepts the proposed changes to the practice area, the contractor should be notified, as soon as possible, in writing of:
- the acceptance
- the date upon which the changes will take effect
- a requirement of the contractor to publish the details of the new practice area within their patient information leaflet and on their website (if they have one)
8.14.9 If the commissioner declines the proposed changes to the practice area, the contractor should be notified, as soon as possible, in writing of that decision and to include:
- the reasons for the decision
- the right of the contractor to appeal and the process for doing so
- specify any period within which the commissioner would not consider a further application from this contractor to vary its practice area
8.14.10 Practices who are intending to reduce their practice area must be advised that registered patients who subsequently fall outside of the new agreed area, but who are within the original practice area (main and outer boundary) can only be removed from the list if one or more of the provisions of the relevant regulations/directions that relate to removal of patients from the practice’s patient list apply.
8.15 Premises
8.15.1 A contractor may wish to make changes to its contracted practice premises (including branch surgeries – for further information, see paragraphs 8.15.10 to 8.10.30 below) from which services are provided.
8.15.2 This would likely be a significant change to services for the registered population and as such, the commissioner and the contractor must engage in open dialogue in the first instance to consider the consequences and implications of the proposed change and discuss any possible alternatives that may be agreed between them.
8.15.3 The commissioner and contractor, through their dialogue, may establish that there is a need to retain medical service provision in the locality and must seek to find a solution, which could include tendering for a new provider within that locality, though not necessarily within the same premises.
8.15.4 Once, and if, the final date for closure is confirmed, the commissioner will issue a variation agreement notice to remove the registered address from the contract, and as in other variations under this policy, include the wording of the variation and the date on which it will take effect. The commissioner must also inform PCSE for changes to the main site location.
8.15.5 The contractor will be fully responsible for the cessation or assignment of the lease for any rented premises and any disposal of owner-occupied premises.
8.15.6 While it is likely that a PMS/APMS contract would reflect the terms as laid out in the GMS contract example above, it is essential that the commissioner reviews the individual contract for relevant provisions that relate to removing the closing premises and any rights associated with that premises.
8.15.7 Where the premises relocation is in relation to a dispensing doctor’s practice, contract managers should also refer to the Pharmacy manual, as moving the site may have significant implications for which patients are eligible to be dispensed to by the practice.
8.15.8 The practice should also apply separately for permission to relocate the dispensing rights of the practice elsewhere, and the timeframes involved in getting approval for that relocation may influence the broader relocation plans and timetable.
Branch surgeries
8.15.9 It is important to note that unless there are specific reasons for variation, branch surgeries should be held to the same standard of service level as a ‘main surgery’, unless there is specific reason for a lesser service provision. An example of this may be in rural areas, where the principle is ensuring local access and this would be for local commissioning determination.
Branch closure
8.15.10 The closure of a branch surgery may be as a result of an application made by the contractor to the commissioner or due to the commissioner instigating the closure following full consideration of the impact of such a closure.
8.15.11 In the circumstances that the commissioner is instigating a branch closure, the commissioner must be able to clearly demonstrate the grounds for such a closure and fully considered any impact on the contractors registered population and any financial impact on the actual contractor. The commissioner will be expected to demonstrate that they have considered any other options available prior to instigating a branch closure and entering a dialogue with the contractor as to how the closure is to be managed. The commissioner will need to have complied with the duty (under section 13Q of the NHS Act) to involve patients in decision-making before any final decision to close a branch is made.
8.15.12 Where a contractor wishes to close a branch surgery, the contractor should have preliminary discussions with the commissioner to determine appropriate and proportionate patient involvement requirements prior to the consideration of such a service provision change. Even though the closure is being instigated by the contractor, the commissioner will still need to comply with the section 13Q duty to involve patients in decision-making before any final decision is made.
8.15.13 The closure of a branch surgery would be a significant change to services for the registered population and as such the commissioner and the contractor should engage in open dialogue in the first instance to consider the consequences and implications of the proposed change and discuss any possible alternatives that may be agreed between them. At this stage, the duty to involve the public in proposals for change is triggered and the commissioner and contractor should work together on fair and proportionate ways to achieve this. The commissioner should ensure clarity on what involvement activities are required by the contractor.
Contractor and commissioner discussions resulting ultimately in a decision about a branch closure will often include consideration of (but not be limited to):
- financial viability
- registered list size and patient demographics
- condition, accessibility and compliance to required standards of the premises
- accessibility of the main surgery premises including transport implications
- the commissioner’s strategic plans for the area
- other primary health care provision within the locality (including other providers and their current list provision, accessibility, dispensaries and rural issues)
- dispensing implications (if a dispensing practice)
- whether the contractor is currently in receipt of premises costs for the relevant premises
- other payment amendments
- possible co-location of services
- rurality issues
- patient feedback
- any impact on groups protected by the Equality Act 2010 (for further detail see chapter 4: general duties of NHS England)
- the impact on health and health inequalities
- any other relevant duties under part 2 of the NHS Act (for further detail see chapter 4: general duties of NHS England)
8.15.14 The commissioner and contractor, through their dialogue, may establish that there is a need to retain medical service provision in the locality and must find a solution, which could include tendering for a new provider within that locality though not necessarily within the same premises. Note that most changes in premises will trigger the commissioner’s duties to involve patients in decision-making.
8.15.15 The commissioner should confirm any such arrangements and agreements in writing to the contractor as soon as is practicably possible after the agreement is reached and must notify PCSE of any branch closures, so that PCSE can update the record of the GP practice. Please note, PCSE do not provide services connected to a branch site closure. If the practice or commissioner wish to use to PCSE to inform patients or to move paper medical records, this will need to be commissioned separately with PCSE.
8.15.16 If the commissioner and the contractor are unable to reach an agreement to keep the branch surgery open, then the contractor, based upon their previous discussions with the commissioner regarding appropriate and proportionate involvement, will continue to involve patients in the proposed changes.
8.15.17 The contractor is required to follow:
- The patient and public participation policy
- The statement of arrangements and guidance on patient and public participation in commissioning
- The framework for patient and public participation in primary care commissioning
8.15.18 Process as appropriate to the arrangements agreed with the commissioner, with support and advice as appropriate from the commissioner. Adherence to the patient and public participation (PPP) involvement process will help ensure that an appropriate involvement exercise is carried out, that meets the legal obligations on the commissioner.
8.15.19 Once this involvement exercise has been undertaken and the results provided to the commissioner, the contractor would then submit a formal application to close the branch surgery to the commissioner for consideration (annex 14A: template application to close branch premises).
8.15.20 The commissioner will then assess the application regarding the closure and the outcome of the patient involvement exercise with a view to either accepting or refusing the proposal. These assessments will need to again consider all the relevant factors, including those listed in paragraph 8.15.13. The commissioner should document how it has taken the various factors into account.
8.15.21 Either the contractor or the commissioner may invite the LMC to be a party to these discussions at any time.
8.15.22 Where the commissioner refuses the branch closure through its internal assessment procedure, the contractor shall be notified in writing within 28 days following the internal assessment and the contractor may then follow the relevant resolution process as referenced in the contract. Please refer to annex 14B: acknowledgment of application to close branch premises.
8.15.23 Where the commissioner approves the branch closure, the commissioner will need to ensure that it retrieves all NHS owned assets from the premises.
8.15.24 The contractor remains responsible for ensuring the transfer of patient records (electronic and paper Lloyd George notes) and confidential information to the main surgery, having full regard to confidentiality and data protection requirements, records management: NHS code of practice guidance and any relevant guidance from the NHS England or the Information Commissioner’s Office. Where a third-party contractor is being used to handle records, they must be vetted and appropriate contractual arrangements put in place.
8.15.25 The contractor remains responsible for carrying out public involvement in accordance with the instructions given by the commissioner and informing the registered patients of the proposed changes. However, ultimately it is the commissioner’s responsibility to ensure that involvement activities have met legal requirements, even if carried out by the contractor. Further guidance can be found in the NHS England documents The patient and public participation policy, The statement of arrangements and guidance on patient and public participation in commissioning, and The framework for patient and public participation in primary care commissioning
8.15.26 Once the final date for closure is confirmed, the commissioner will issue a standard variation notice to remove the registered address of the branch surgery from the contract, including the amended sections of the contract for completeness.
8.15.27 Where the contractor has previously been granted premises consent to dispense, and these rights are only associated with the closing premises in question (that is listed on the relevant dispensing contractor list), the contractor’s consent to dispense will cease.
8.15.28 The commissioner shall update its records and ensure that the relevant dispensing contractor list is updated appropriately to reflect the removal of the premises.
8.15.29 It is possible that a PMS or APMS contract will reflect the terms as set out above. It is however essential that the commissioner reviews the individual contract for these or any other relevant provisions to allow a variation to effectively remove the closing premises and any rights associated with that premises alone.
8.15.30 Where the commissioner is operating under delegated authority and is considering a branch closure, the commissioner must have regard to the matters set out in the delegation agreement as indicated in section 11.14 of this policy.
8.16 Opt-outs
8.16.1 Services under primary medical contracts are categorised as:
8.16.2 Essential services – these are the services described in regulation 15 of the GMS regulations which a GMS contractor must provide. Essential services are not mandatory for PMS or APMS contractors.
8.16.3 Minor surgery and out of hours – these are specific services that are additional to essential services. It is not mandatory for contractors to provide these services but where GMS and PMS contractors provide such services, the contracts must contain terms relating to the procedure for opting out of those services. It is not a requirement that APMS contracts contain such opt out provisions but the commissioner should review the relevant APMS contract to determine whether any such provisions have been included; or
8.16.4 Enhanced services – these are any services that go beyond essential, minor surgery or out-of-hours services that the contractor may have agreed to be included.
8.16.5 Where a contractor has opted out of delivering minor surgery or out of hours services, the commissioner must commission these services from an alternative source for the registered patients under that contract.
8.16.6 Prior to any opt out taking effect, the commissioner and the contractor shall discuss how to inform the contractor’s patients of the proposed opt out. The commissioner can request the contractor to inform its registered patients of an opt out and the arrangements made for them to receive minor surgery or out of hours services by either placing a notice in the practice’s waiting rooms; or including the information in the practice leaflet.
8.16.7 The regulations do not refer to opt-ins, ie where a contractor wishes to provide services which it previously opted out of providing. If the commissioner receives a request to opt-in, it should refer to their legal team (england.legal@nhs.net) for consideration of the procurement implications.
Opt-out of minor surgery
8.16.8 Where a contract wants to opt out of providing minor surgery services, the contractor must notify the commissioner in writing stating the reasons for wishing to opt out. This notice is referred to as a preliminary opt-out notice.
8.16.9 As a next step, the commissioner must discuss with the contractor what support the commissioner may give the contractor to enable the contractor to continue to provide minor surgery. The parties must also discuss other changes which with party could make to enable the contractor to continue providing the service. These discussions must be started as soon as is reasonably practicable and in any event within 7 days beginning with the receipt of the preliminary opt-out notice. The commissioner and the contractor must use reasonable endeavours to achieve this aim of enabling the contractor to continue to provide minor surgery.
8.16.10 The discussions must be completed within 10 days beginning with the date of the receipt of the preliminary opt-out notice or as soon as reasonably practicable after the 10 days.
8.16.11 If, after the discussions, the contractor still wishes to opt out of minor surgery, the contractor must send an opt-out notice to the commissioner which must include:
- whether the contractor wishes to temporarily or permanently opt out
- the reasons for wishing to opt out
- the date from which the contractor would like the opt out to commence, which must:
- in the case of a temporary opt out, be at least 14 days after the date of service of the opt-out notice
- in the case of a permanent opt out, must be the day either 3 or 6 months after the date of service of the opt-out notice
- in the case of a temporary opt out, the desired duration of the opt out
8.16.12 The contract regulations do not allow contractors to temporarily opt out of providing minor surgery more than twice. Where a contractor has given 2 previous temporary opt-out notices within the period of 3 years ending with the date of the service of the latest opt-out notice, the commissioner must treat the latest opt-out notice as a permanent opt out (even if the notice says that it wishes to temporarily opt out).
Temporary opt-out of minor surgery
8.16.13 Where the contractor has provided a temporary opt-out notice, the commissioner must follow the process below:
- the commissioner must, as soon as is reasonably practicable and in any event within the period of 7 days beginning with the date of receipt of a temporary opt-out notice, either:
- approve the opt-out notice and specify both the date on which the temporary opt out is to commence (which wherever reasonably practicable must be the date requested by the contractor in its opt out notice) and the date that it is to come to an end (“the end date”); or
- reject the opt-out notice on the ground that the contractor:
- is providing minor surgery to patients other than its own registered patients or enhanced services, or
- has no reasonable need temporarily to opt out having regard to its ability to deliver minor surgery
- the commissioner must notify the contractor whether it has approved or rejected the opt-out notice as soon as possible, including reasons for its decision
8.16.14 The commissioner or the contractor may have concerns about the ability of the contractor to provide the services at the end of the temporary opt out. If the commissioner considers that the contractor will be unable to satisfactorily provide minor surgery at the end of the temporary opt out, the commissioner can agree with the contractor to extend the end date. If such extension is not possible, the commissioner may notify the contractor in writing at least 28 days before the end date that a permanent opt out shall immediately follow the temporary opt out. Similarly, a contractor who has temporarily opted out may, at least 3 months prior to the end date, notify the commissioner in writing that it wishes to permanently opt out of minor surgery.
Permanent opt out of minor surgery
8.16.15 Where the contractor has provided a permanent opt-out notice, the commissioner must approve or reject it. The commissioner must do so as soon as is reasonably practicable and in any event within the period of 28 days beginning with the date of receipt of a permanent opt-out notice. The only ground on which the commissioner may reject the notice is that the contractor is providing minor surgery to patients other than its registered patients or enhanced services. The commissioner must notify the contractor of its decision as soon as possible, including reasons for its decision where its decision is to reject the opt-out notice.
8.16.16 If, after the commissioner approves a permanent opt-out, the contractor wishes to withdraw the notice, it can only do so if the commissioner agrees. This is because after approving the opt-out, the commissioner must use reasonable to make arrangements for the contractor’s registered patients to receive minor surgery from an alternative provider.
8.16.17 It may be difficult for the commissioner to find an alternative provider to deliver minor surgery from the date on which the contractor proposed to opt out. Where this is the case, the commissioner must notify the contractor 1 month before the proposed opt out date requiring the contractor to continue to provide minor surgery for a certain period as set out below.
8.16.18 Where the proposed opt out date is 3 months after service of the opt-out notice (if 6 months, see paragraph 8.16.20), the contractor shall continue to provide minor surgery until the day 6 months after the service of the opt-out notice. If, during this period, the commissioner, despite using its reasonable endeavours, is still unable to find an alternative provider, it can provide a further notice to the contractor requiring the contractor to provide minor surgery until the day 9 months after the date of service of the permanent opt-out notice.
8.16.19 The contractor may find it difficult to continue providing minor surgery for a further 9 months. Therefore, as soon as is reasonably practicable and in any event within 7 days of the commissioner serving a further notice to the contractor to continue providing minor surgery until 9 months after the date of service of the permanent opt-out notice, the commissioner must enter discussions with the contractor. These discussions must consider what support the commissioner may give to the contractor or other changes which either party may make in relation to the provision of minor surgery until the actual opt out date. The requirement to enter discussions only arises where the commissioner requires the contractor to provide minor surgery until the date 9 months after service of the opt out notice. It does not apply where the commissioner requires the contractor to provide minor surgery until the day 6 months after service of the opt-out notice.
8.16.20 Where the proposed opt out date is 6 months after service of the opt-out notice, the contractor shall continue to provide minor surgery until the day 9 months after the service of the opt-out notice.
Opt-out of out of hours
8.16.21 If a contractor wishes to terminate its obligation to provide out of hours services, it must provide the commissioner with an out of hours opt-out notice specifying the date from which the contractor would like the opt out to take effect, which must be either three or 6 months after the date of service of the out of hours opt-out notice.
8.16.22 As soon as is reasonably practicable and in any event within 28 days of receiving the out of hours opt-out notice, the commissioner shall approve the notice and confirm the date on which the out of hours opt out is to commence. The commissioner cannot reject an out of hours opt-out notice.
8.16.23 If, after the commissioner approves an out of hours opt-out notice, the contractor wishes to withdraw the notice, it can only do so if the commissioner agrees. This is because after approving the opt-out, the commissioner may have made arrangements for the contractor’s registered patients to receive the out-of-hours service from an alternative provider.
8.16.24 If the commissioner cannot find an alternative provider, paragraphs 8.16.17 to 8.16.20 will apply as if the reference to minor surgery was a reference to the out-of-hours service.
8.16.25 Once the terms of any permanent or temporary opt out are agreed, a variation notice must be issued in accordance with the principles laid out in this policy to amend the relevant section of the contract.
8.16.26 The commissioner should follow the same process for PMS contractors. For APMS arrangements, the commissioner should review the contract to determine whether it contains any relevant provisions.
8.17 Financial changes – statement of financial entitlements (SFE)
8.17.1 The contract will contain the terms of any payments due. Any change to those terms will require a notice of variation which should be provided no less than 28 days before the proposed variation takes effect.
8.17.2 For GMS contracts, the financial terms must reflect those set out in the GMS SFE. There is no such requirement under PMS or APMS contracts which have been locally agreed. NHS England does however have a policy of equitable funding for the core services expected of all GP practices. Any changes under the GMS SFE should be reviewed against the terms of each of the individual contracts to ascertain what, if any, affect those changes have on local financial terms.
8.18 Annex 4 primary care support services notifications
8.18.1 Commissioners should ensure that following any contractual merger, GP performers are informed of their obligation to notify Primary Care Support England (PCSE) using the relevant online portal or forms issued by NHS England within 28 days.
8.18.2 Additionally, and more generally, GP performers and indeed performers in all contractor groups are required to notify PCSE of any changes relevant to their entry on the national performers list. Further information is available on the PCSE website.
9 Managing a PMS contractor’s right to a GMS contract
9.1 Introduction
9.1.1 The aim of this policy is to ensure that all parties to the contract understand the process and procedures that must be followed when a contractor requests a transfer from a PMS agreement to a GMS contract.
9.1.2 Subject to the contractor’s eligibility to hold a GMS contract and the requirement to provide essential services, then there should be no variation in the application of this policy.
9.2 Roles and responsibilities
9.2.1 Commissioners will need to ensure that the finance department and relevant persons are made aware of the change to the contracting arrangements as there will be long term financial implications. A GMS contract is not time limited and exists in perpetuity. Anyone with delegated authority can sign off the transfer.
9.2.2 The payment and contract management system must be updated by the officer managing the transfer.
9.3 Background
9.3.1 A contractor holding a PMS agreement which is providing essential services, has the right to a GMS contract in accordance with regulation 32 of the PMS regulations which states:
9.3.2 “A contractor which is providing essential services and which wishes a general medical services contract to be entered into pursuant to this regulation shall notify [the commissioner] in writing at least 3 months before the date on which it wishes the general medical services contract to be entered into”.
9.3.3 This policy sets out the decision-making process that the commissioner will follow, together with refusal (where eligibility is not satisfied), appeal processes and discussions regarding any actions that are required.
9.4 Notification from a contractor
9.4.1 The commissioner should receive at least 3 months’ notice in writing from the contractor requesting a GMS contract.
9.4.2 The contractor’s notice must:
- state that the contractor wishes to terminate the PMS agreement
- state the date on which the contractor wishes the PMS agreement to terminate which must be at least 3 months after the date of service of the notice
- give the name of the person(s) with whom the contractor wishes the commissioner to enter into a GMS contract (a person’s name may only be given in a notice if that person is a party to the PMS agreement)
- confirm that the person(s) named meet the conditions set out in section 86 of the NHS Act (persons eligible to enter into GMS contracts) and regulations 4 and 5 (where applicable) of the GMS regulations or, where the contractor is not able to confirm, the reason why it is not able to do so and confirmation that the person(s) immediately prior to entering into the GMS contract will meet those conditions
9.5 Process for PMS agreements
9.5.1 The commissioner must acknowledge receipt of the notice within 7 days beginning on the day it received the notice.
9.5.2 While it is not a requirement of the PMS regulations, when the commissioner receives such a notice it should discuss the full implications of this action with the contractor to ensure the contractor has fully understood the necessary changes to the contractual income streams (see paragraph 9.5.4) and should advise the contractor to seek their own independent advice.
9.5.3 The commissioner will check that all necessary information has been provided in the contractor’s notice and undertake a review of the PMS agreement to establish if the contractor provides essential services; and if they are eligible to hold a GMS contract (as set out in section 86 of the NHS Act (persons eligible to enter into GMS contracts) and regulations 4 and 5 of the GMS regulations. This information is referenced in the contracts described chapter.
9.5.4 The commissioner must apply the GMS SFE on first setting up a GMS contract and calculating the global sum monthly payment. Whilst a PMS contractor has the right to a GMS contract, there is no entitlement for the contractor to carry the same funding arrangements it had under the PMS agreement into that GMS contract. GMS contracts are funded according to terms set out in the GMS SFE while PMS agreements are funded through local agreement. There is the discretion to agree additional payments under GMS arrangements out with the GMS SFE which are not necessarily payable under the GMS SFE. It is essential that the commissioner has ascertained the financial impact of this decision of the contractor to move to a GMS contract.
9.5.5 If the contractor does not provide essential services, the commissioner must notify the contractor that they are not entitled to transfer to a GMS contract. A template letter is provided in annex 1.
9.5.6 If the contractor is not eligible to hold a GMS contract the commissioner must refuse to enter into a GMS contract. A template letter is provided in annex 2.
9.5.7 If the commissioner confirms that the contractor provides essential services and is eligible to hold a GMS contract under section 86 of the NHS Act and regulations 4 and 5 of the GMS regulations, the commissioner will acknowledge receipt of the notice and outline the next steps within seven days of receipt of the notice. A template letter is provided in annex 3.
9.5.8 The GMS contract will start immediately after the termination of the PMS agreement. The GMS contract start date should be the date set out in the notice to the commissioner unless a different date is agreed by the parties. The GMS contract will include all the terms required by the GMS regulations.
9.5.9 The new GMS contract must require the provision of the same services that were commissioned under the PMS agreement and were provided by the contractor immediately prior to the PMS agreement terminating unless the parties otherwise agree.
9.5.10 The names of the patients included in the contractor’s list of patients immediately before the PMS agreement termination must be included in the first list of patients prepared and maintained by the commissioner.
9.5.11 The out-of-hours services must be the same as were provided under the PMS agreement before it terminated.
9.5.12 The commissioner must use the current standard GMS contract ensuring that it is amended to the specific contractor.
9.5.13 Once a GMS contract is agreed and entered into and the PMS agreement has terminated, the commissioner must ensure all nationally held records of the contractor’s status are adjusted appropriately. This must include, but not be limited to, changing the contractor’s status on Calculating Quality Reporting Service, from PMS to GMS, to ensure that the correct quality and outcomes framework calculations are completed at year end and any contractual payment systems used, (ie Exeter).
9.5.14 The calculation of the contractor’s first initial global sum monthly payment must be made in accordance with part 1 of the GMS SFE.
9.6 Disputes
9.6.1 Where there is a dispute about whether or not a person satisfies the conditions set out in section 86 of the NHS Act or regulations 4, 5 and 6 of the GMS regulations, the contractor may appeal to the First-Tier Tribunal.
9.6.2 Any other dispute about the GMS contract shall be determined by the Secretary of State (NHS Resolution (NHSR) – Primary Care Appeals (PCA)) in accordance with regulation 9(2) and (3) of the GMS regulations (pre-contract disputes).
9.6.3 The commissioner can identify whether the contract is an NHS contract or not by reviewing the agreement. This will enable the commissioner to identify whether they can apply for NHS dispute resolution (with or without the need for the written consent of the contractor) if appropriate.
10 Practice closedown (planned/scheduled)
10.1 Introduction
10.1.1 This policy outlines the approach to be taken when a time-limited primary medical services contract is coming to an end. Where an urgent contract needs to be put in place (please refer to the contracts described chapter for further information).
10.2 Scope
10.2.1 Time-limited contracts can be in place regarding GMS, PMS and APMS contract types. GMS contracts, however, do not usually have an end date but a temporary GMS contract can be put in place for a period not exceeding 12 months, for the provision of services to the former patients of a contractor following the termination of that contractor’s contract.
10.2.2 PMS agreements may be in perpetuity or for a time limited period. Commissioners should review the relevant PMS agreement to establish if there is a defined end-date.
10.2.3 APMS contracts must be for a fixed-term period the duration of which is governed by standing financial instructions (e NHS England currently require all clinical contracts of 10 years or more (or a lifetime contract value of £500 million or higher) to be submitted for commercial business case approval). The main purpose of time limiting these contracts was to provide commissioners the scope for testing the market and ensuring value for money as well as providing the opportunity to review service needs.
10.2.4 In each of the cases above there are generic principles that will apply and individual circumstances that will need to be considered. This policy covers the steps to be taken in advance of the end of any contract and will support the commissioner in planning procurement cycles and future service provision.
10.2.5 The commissioner must consider whether the expiring contract contains provisions relating to the end of the contract that impacts on any practice closedown actions. The NHS England’s standard primary medical service contracts contain provisions relating to the consequences of termination including a requirement that the contractor co-operates with the commissioner and arrangements for a financial reconciliation exercise.
10.2.6 Contracts may come to an end by reasons other than by expiry including by:
- being terminated by either the commissioner or the contractor (in which case refer to the chapter on contract breaches, sanctions and terminations)
- an adverse event (in which case refer to the chapter on adverse events)
- the death of the contractor (in which case refer to the chapter on the death of a contractor)
- retirement of the contractor (in which case refer to the chapter on contract variations)
10.3 Timetable for managing contracts coming to an end
10.3.1 The commissioner needs to be aware of the end dates of all contracts held so that advance planning can be undertaken to ensure both capacity and timescales can be aligned with the key stages outlined below.
10.3.2 It is essential that the commissioner ensures continued communication with contractors throughout the stages to enable them to have a clear understanding of the processes, expectations and obligations. Outlined in annex 1 and annex 2 are guides to communications with contractors and a proposed checklist for documentation recording.
10.3.3 Commissioner should also refer to PCSE practice mergers and closures process. In the case of a planned closure, the commissioner should involve PCSE in the process as soon as possible but not later than 14 days of when a closure/merger is to take effect. Further information is available on the PCSE website.
10.3.4 In each of the stages below there is a range of activities that may need to be undertaken, depending on the commissioner’s preferred route, and the commissioner may usually discuss with the appropriate LMC throughout.
10.4 Summary of key stages
There are 3 key stages:
10.4.1 Stage 1 – minimum 9 to 15 months before contract end (all essential):
(a) needs assessment
(b) impact
(c) engagement proposal
10.4.2 Stage 2 – 12 months before contract end:
(a) notice period – exit plan
(b) commence procurement and either:
(c) begin negotiations for continuation with contractor
(d) begin exit arrangements of incumbent provider and mobilisation of any new provider
10.4.3 Stage 3 – at contract end:
(a) contract end – possible dispersal of patient list
(b) variation to contract/extension
(c) commencement of new provider
10.5 Stage 1-9-15 months before contract end
10.5.1 The considerations that should be given when completing each action are provided below. This list is not exhaustive but does provide a platform for commissioners to fully assess the existing and future service needs of its population. Commissioners should ensure that all appropriate stakeholders are given the opportunity to input into the needs assessment for their population, including but not limited to public health.
(a) Needs assessment
10.5.2 Is there still a demand for this service in this locality and a requirement for it to continue? For example, to reduce inequalities in access or health outcomes.
10.5.3 Does the contract specification still address current local priorities?
10.5.4 Has the contract delivered on the expected outcomes?
10.5.5 Has it provided added value to the local population and service provision?
10.5.6 Have you assessed the potential service needs for any forthcoming new developments?
10.5.7 What is the capacity of other local providers and the market for other providers to deliver services?
10.5.8 Have you given consideration to any specialist services needs in the locality?
10.5.9 Are there any needs that are not met by the contract, which could be delivered?
(b) Impact
10.5.10 Have you considered available outcome and delivery data held nationally and locally, regarding the current service and impact on other providers?
10.5.11 Have you compared the cost of the current service against other providers, ie cost per head of population whilst taking into account any differences in the scope of the services provided?
10.5.12 Is the current service still affordable within projected future budgets?
10.5.13 Has the contract delivered on the expected financial outcomes?
10.5.14 What other objectives might be set within the existing budget?
10.5.15 Have you considered the potential impact on service users/patients?
10.5.16 Have you considered the potential impact on other service providers, eg GPs, pharmacy, local trust, out of hours, community services?
10.5.17 Have you considered the potential impact on the current provider, ie continued viability within the locality?
10.5.18 Have you considered patient choice and equality?
10.5.19 Have you considered the potential risks, ie reputational (adverse publicity, commissioner/provider relationship), market testing, timescales and financial?
10.5.20 Have you considered how the expiry of the contract affects compliance with the general duties? For further information, please refer to the chapter covering general duties of NHS England.
(c) Engagement proposal
10.5.21 Each situation will need to be managed regarding each individual circumstance and the nature of the procurement process to be followed, if at all. However, where it has been deemed appropriate to complete a form of engagement before taking action, the commissioner should consider:
10.5.22 Have arrangements been made for the involvement of patients and the public (please refer to the chapter covering general duties of NHS England) for more information on this requirement)?
10.5.23 Have other local providers and other interested parties, ie LMC, local members of parliament, review and scrutiny committee, etc been engaged?
10.5.24 Have the local ICBs been engaged?
10.5.25 If the answer is ‘no’ regarding any of the above, the commissioner should be able to identify the grounds under which they felt engagement was unnecessary and these should be included in the report defined below.
10.5.26 Completion of stage 1 will provide all the information required to enable the commissioner to make an informed commissioning decision on whether to recommission, procure or allow the service to end. At this stage, the commissioner should develop a detailed report (a template is provided in annex 3) about the investigations undertaken, engagement and outcomes. This report shall demonstrate that the commissioner has considered all possible options and the rationale behind the decision taken.
10.6 Stage 2 – 12 months before contract end
10.6.1 Below are the potential next stages following stage 1 based upon the commissioner’s decision regarding the proposed way forward. It is important to note that where a contract has a duration or an end date specified, and the intention is to allow the contract to naturally expire, there is no requirement to issue a formal termination notice. It would be best practice to issue a formal letter of notice detailing the commissioner’s intentions and the obligations on the contractor throughout the remainder of the contract period.
(a) Notice period – exit plan
10.6.2 Issue a letter of notice of intentions.
10.6.3 Develop an exit plan (a template is provided in annex 4) with the contractor with clearly defined commissioner/contractor responsibilities. This should be developed whether the contract is to cease or transfer to a new provider. Commissioner should review the contract and ensure any exit arrangements detailed in the contract are followed.
(b) Procurement
10.6.4 Ensure any new contract is procured in accordance with procurement law. Commissioners must also act in accordance with any procurement protocol issued by NHS England.
10.6.5 Once a preferred provider is established, agree an operational management plan (a template is provided in annex 5 – this template should only be used where the contract does not contain exit arrangements as any such arrangements take precedence over the template).
(c) Begin negotiations for continuation of the contract with the existing contractor, if appropriate
10.6.6 Extending any contract beyond a previously agreed end date could be considered a material change to the terms of that contract which could lead to a procurement challenge.
10.6.7 If there is no extension period already included in the contract, the commissioner will need to consider carefully whether such an extension should instead be subject to a full procurement process to ensure best value and mitigate the risk of challenge from previous and/or potential alternative service providers. If the commissioner’s decision is that no procurement process is necessary, then it must ensure it is aware of the necessary steps which must be taken to satisfy procurement law and any procurement protocol issued by NHS England.
10.6.8 Once the decision to extend has been reached and all correct processes have been followed the commissioner will need to consider:
- the length of the extension
- any alterations to the existing contract (including the financial arrangements)
- any agreement of new key performance indicators
(d) Begin exit arrangements (completion of stage 2)
10.6.9 Completion of stage 2 will provide the commissioner with the firm foundations and detailed preparations ready to manage the end of the contract.
10.7 Stage 3 – at contract end
Below are the possible outcomes culminating from stages 1 and 2.
(a) Contract end
10.7.1 Service ceases.
10.7.2 Dispersal of list if applicable (please refer to comments on managing patient lists in the termination section of the chapter on contract breaches, sanctions and terminations and section 2.5 of the unplanned closures chapter regarding orphan data.
10.7.3 Communication to be sent out to all those parties involved, eg management of patient communication working with provider, management of the press, notification of contract end to relevant stakeholders.
(b) Variation to contract – extension
10.7.4 Contract variation issued and signed off by both parties.
(c) Commencement of the new provider
10.7.5 Issue of a new contract.
10.7.6 Operational management plan implemented.
10.7.7 Relevant communications undertaken, internally and externally.
10.7.8 On completion of stage 3, the commissioner will have reached an agreed, structured outcome about the management of contract end.
10.7.9 As part of any practice close down, PCSE makes a site visit to remove, store and forward patient records to a new provider(s). Patient records should contain reprints of electronic records for patients who have not re-registered at the point of practice closure and will need to be individually placed in transit polytopes. Records will only be collected from the closing practice main site. The GP practice should send PCSE a list of records that are being collected. Records are held in archive until the patient re-registers, or the retention period expires, and they are securely destroyed.
10.7.10 Commissioner should ensure that the dispersal of all registered patients from the closed practice should be completed immediately following the contract end date and within 6 months at the very latest, as after this date the practice is classified as closed on national it systems. This includes, reconciling any patients who may have chosen not to re-register, ghost patients etc.
10.8 Primary care networks
10.8.1 When new services are procured, the commissioner should facilitate a discussion between the incoming contractor and the relevant primary care network (PCN), involving the relevant LMC, to ensure uninterrupted network services for the incoming contractor’s registered patients.
10.8.2 If the provider is not willing to join the PCN, then the commissioner will work with the existing PCN core network practices to ensure continuity of services to the registered patients of the practice not signed up to the Network Contract DES.
10.8.3 If the PCN is not prepared to accept the provider as a member, the commissioner may require a PCN to include the practice as a core network practice of that PCN. Where the commissioner is minded to require a PCN to do so, the commissioner must engage with the relevant LMC and, when making its determination, have regards to the views of the LMC. Section 4.6 of the Network Contract DES 2023/24 – PCN Requirements and Entitlements sets out the process for allocating a practice to a PCN.
10.9 Links to relevant PCSE information and documentation
11 Discretionary payments (made under section 96 of the NHS Act)
11.1 Introduction
1.1.1 Section 96 of the NHS Act (2006) (as amended) makes provisions for NHS England (delegated to local commissioners) to provide assistance and support to:
11.1.1.1 Primary medical services contractors, including financial support.
96 Assistance and support: primary medical services
(1) NHS England may provide assistance or support to any person providing or proposing to provide –
(za) primary medical services pursuant to section 83(2),
(a) primary medical services under a general medical services contract, or
(b) primary medical services in accordance with section 92 arrangements
(2) Assistance or support provided by NHS England under subsection (1) is provided on such terms, including terms as to payment, as NHS England considers appropriate.
(3) “Assistance” includes financial assistance.
11.1.2 For clarity of purpose, assistance and support relates to the provision of either:
- education or training
- financial assistance
- any other resources available to NHS England or the commissioner
11.2. However, NHS England is increasingly being expected to demonstrate publicly what it is spending its money on, what it is getting for its money and of that funding that is allocated to support initiatives that this is done fairly and in the best interests of the organisation and public funds. As such when providing any financial assistance, you must be able to demonstrate that you have acted with propriety, that you have understood and complied with any wider financial requirements as set out in the NHS England standing financial instructions, that you have followed all steps to provide best value for money and that you have followed requirements in relation to public sector bodies as stipulated in HMT managing public money (May 2023).
11.3 Key principles
11.3.1 All financial assistance must be provided within the principles of openness, fairness, probity and accountability.
11.3.2 The provision of financial assistance should not conflict with UK policies and actions including the rules on fraud, bribery, corruption, competition, state aid and other equality duties.
11.3.3 It must be demonstrated how the financial assistance supports NHS England and local commissioner functions and strategic objectives.
11.3.4 Financial assistance must demonstrate value for money and be in the best interests of NHS England, local commissioners and the patients.
11.3.5 Financial assistance must be proportionate to the identified need and represent better value for the taxpayer than alternative solutions.
11.3.6 Financial assistance will only be made available in exceptional circumstances and NHS England (delegated to the local commissioner) has the statutory duty to determine the payment terms.
11.4 Programme and non-programme financial assistance
11.4.1 Section 96 exceptional discretionary funding is generally used to safeguard patients’ interests by providing additional funding to support persons or public authority bodies, as listed in section 11.1 facing a crisis situation.
11.4.2 Often, financial assistance was made available through formal programmes such as the General Practice Resilience Programme (GPRP) or the current Covid Support Fund .
11.4.3 However, formal national programmes of support do not cover or replace all circumstances where there is a need for support and agreement on eligibility for funding support from local primary care budgets. Their proposed use – and the amount provided – will still generally need to be managed by individual local commissioners. When setting up a new section 96 financial assistance scheme, commissioners should seek legal advice as some section 96 payments may constitute a subsidy and be subject to the relevant control regime.
11.4.4 The pressures on general practice mean that requests for support are being received more frequently with a consequent need to have a more structured approach to considering and approving such expenditure outside of formal programmes.
11.4.5 It is also important to ensure that ad hoc requests are minimised through pro-active work with practices via appropriate programmes of support that may be in place.
11.5 Process for financial assistance for individual provider
Please note: updated for delegated ICB commissioning.
1. The practice raises its sustainability issue with its ICB contract officer to discuss issues. Verify contract payments are correct.
2. Practice submits Section 96 application (appendix 1) accompanied by the level of support requested, for what period, and for the type of expenditure with evidence provided to support application and ICB support
3. Primary Care team review submission and if necessary request for further information/supporting documentation in order to produce a business case.
4. Following review and validation of the practice information, a business case for the proposed financial assistance must be completed. This must confirm:
- the name and reference code of practice for whom discretionary payment request is being made
- the level of financial assistance being requested and the level being recommended
- how the financial assistance will be paid
- how long is the support anticipated to be needed (either to achieve a resolution or to prepare a business case for long term support) generally no more than a maximum of £200,000 or 3 months funding should be considered (apart from in exceptional circumstances)
- the practice need for financial assistance has been validated
- description of what precipitated the request for discretionary funding
- confirmation of what practical and financial support the practice has already invested to resolve these issues
- confirmation that the practice agrees to receiving the support and any conditions placed on the support including confirmation of any conditions
- details of the practices plan to recover the position and demonstrate that the short-term support will deliver a sustainable solution in the long term to ensure that the support is non recurrent
- performance management arrangements in respect of the financial assistance
- the case represents value for money
- financial assistance is a better option than any alternatives
- confirmation that the expenditure is in the ‘normal course of business’ for primary medical services
- confirmation that there is no reason why greater transparency is required in respect of the payment
- whether the contractor is already identified under any national or local programme providing support
- whether the contractor has applied for and/or received any funding (whether from any NHS or government body, or commercially) that relates to same subject matter of the s.96 application
- confirmation that there is no additional obligation being placed on NHS England as a result of the financial assistance, that this financial assistance does not arise out of a dispute or claim nor is there any fault or issue which a court may hold requires a payment must be made
5. Review of financial evidence including certified accounts for the previous year and management accounts for the current year, cash flow, declared earnings etc.
Consideration of whether the financial assistance will be sufficient to achieve the objectives.
Consideration of value for money vs alternatives.
Total likely overall financial risk to NHS England.
6. Before the application and any required business case is passed for authorisation the application must be considered and recommended by ICB local arrangements as required.
Where, in exceptional circumstances, the financial assistance is above £200,000 the business case must be endorsed by:
- the Management Accounts team to confirm the availability of funding within the existing budget
- budget holders for confirmation of the use of this financial assistance, and
- legal advice to confirm the correct use of the financial assistance power
7. All financial assistance provided must be in compliance with NHS England SFIs. As such, any application for financial assistance must be authorised as set out in the SFIs. The authority levels should be confirmed at the time the financial assistance is provided.
8. An application from the contractor along with commissioners business case containing operational and financial reviews set out above, should be submitted and approved in line with the ICBs local governance.
The NHS England regional team should be informed where financial assistance is above £1 million.
ICBs should ensure that financial assistance is approved either in line with ICB SFI, or as set out in the table below, unless the NHS regional team has specified additional or alternative approval requirements.
Below £50,000 | £50,000 to £200,000 | >£200,000 to below £1 million | Above £1 million |
ICB deputy appointed* by director of primary care and public health or director of commissioning, or equivalent senior person |
ICB director of primary care and public health or director of commissioning, or equivalent senior person |
ICB chief financial officer |
ICB chief financial officer and local NHS England team director or director of finance where this is specified locally by the NHS England regional team or in any delegation agreement |
* For audit purposes and compliance to governance manual this must be documented formally.
9. All decisions reported as set out below and logged for central reporting and consistency checking.
10. The practice is advised of outcome.
11. MOU populated and signed by the practice and the ICB.
The MOU must set out:
- name and reference code of practice (the ‘practice code’) for whom discretionary payment request is being made
- aims and objectives of the funding
- outputs agreed and long-term outcomes are defined, wherever possible, to enable active performance management
- clawback provisions included unless ICB authorised officer confirms that they are not appropriate
- regular reviews and adjustments are included where deemed necessary
- eligible expenditure is stated where necessary
- where appropriate, regular checkpoint meetings will be held to discuss progress against pre-agreed schedule
- supporting documentation and other evidence required to be provided from the recipient as appropriate
12. Payment set-up on a non-recurrent basis.
13. Review of MOU objectives mid-way through period of support.
14. Routine reporting via the primary care activity report (PCAR) (see section 7 below).
15. Advise practice of continuation or further review of support depending on MOU progress.
16. Final review and reporting to local arrangement (as required).
11.6 Process for commissioner proposed financial assistance programmes
11.6.1 Commissioners may only enter into contracts within the statutory powers delegated to it by the Secretary of State for Health and must comply with the following:
- NHS England Scheme of Delegation and standing financial instructions
- other statutory provisions
11.7 Reporting
11.7.1 The primary care activity report (PCAR).
11.7.1.1 PCAR was suspended during the pandemic to support commissioner burdens. It was reinstated in April 2023 collecting commissioning data for 2022/23.
11.7.1.2 A PCAR was introduced in 2016/17 as a new bi-annual collection to support greater assurance and oversight of NHS England’s primary care commissioning responsibilities. It replaced what had often been variable and ad hoc requests for information with a more systematic approach.
11.7.2 The report is managed through Strategic Data Collection Services (SDCS) and focuses on key operational areas for commissioned general practice services.
11.7.3 The 2022/23 iteration of PCAR reinstates the previous collection with the following minor changes:
11.7.4 Questions removed:
11.7.4.1 Question 1: equitable funding which focussed on the totality of section 96 (discretionary) funding awarded by local commissioners to GP practices.
11.7.4.2 Question 6: Primary medical care policy compliance: this assurance statement will now be covered by an annual self-declaration form ICBs must submit as part of a wider assurance framework (across all delegated commissioning responsibilities).
11.7.5 Question added:
11.7.5.1 New question to request count of what are termed ‘incorporation requests’ received and agreed by commissioners. An incorporation request is where a GP practice that is a traditional partnership requests to change its organisational structure to a company limited by shares. It is linked to increasing organisation and delivery of services at a primary care network level.
11.8 Maintaining records
11.8.1 A clear audit trail of all financial assistance authorised, along with any expenditure incurred under this arrangement, must be maintained, and reported. Summary information may be collected by NHS England, but you should also maintain adequate records such that you are able to respond to any other routine financial reporting arrangements. Please refer to section 10.6 for authorising and recording individual applications.
11.8.2 All applications for financial assistance should be recorded using the application (annex 1) and as set out above.
12 Premises running costs and service charges
Policy for consideration of applications from GP contractors for financial assistance towards premises running costs and service charges.
Purpose of the policy
To provide a consistent methodology that is fair, transparent, and equitable, for primary care commissioners to consider formal applications for financial assistance towards premises running costs and service charges in line with the NHS (GMS – premises costs) directions 2024, part 5 directions 47 and 48.
Introduction
The NHS (GMS – premises costs) directions 2024, part 5 directions 47 and 48 enable GP contractors to request financial assistance from the commissioner towards premises running costs and service charges that are not reimbursable elsewhere under the directions. The commissioner is required to consider such applications and, subject to budgetary targets, to approve them.
Applications for financial assistance, under direction 47, in respect of premises running costs, may include costs relating to business rates, business improvement districts levies, water and sewerage charges, the collection and disposal of clinical waste, and certain utilities and other service charges (directions 47 and 48).
Direction 48(3) offers methods for calculating the amount of financial assistance towards service charges that the commissioner may consider:
i. where the amount of the relevant charges can be accurately determined, the amount paid in respect of those charges
ii. where a lease has been in existence for less than 12 months and the amount of relevant charges cannot be accurately determined, the estimated amount of those charges for the first year of the lease; or
iii. where the commissioner has no information as to the amount of those charges, 40% of the amount which the commissioner estimates as being the total yearly service charge.
Directions 47 and 48 are produced in full on the gov.uk website.
What the above provisions take no account of is the period in which financial assistance should be provided; what the trigger(s) for a review might be; applications that the commissioner might prioritise over others in light of other budgetary targets; or whether the financial assistance being requested can be mitigated.
This policy seeks to address these issues.
12.1 Principles
In order for an application for financial assistance to be considered by a primary medical care commissioning organisation, the following principles need to be accepted and adopted by specified stakeholders:
12.1.1 Commissioners will:
12.1.1.1 Prioritise formal applications from GP contractors that have already been made or those from practices proposing to occupy local improvement finance trust, NHS PS (property services), or NHS trust buildings on a head or sub/under lease basis, in recognition of the commissioner’s budgetary targets. This does not preclude GP contractors in other tenancy arrangements or those considering entering new tenancy arrangements making an application to primary care commissioners for financial assistance towards their premises running costs or service charges but recognises that higher service charge costs are more typically evidenced by practices occupying or proposing to occupy NHS owned or head leased premises. This prioritisation is further evidenced within the local estates’ strategies, developed by ICBs with a wide range of local stakeholders, which seek to maximise use of existing public estate.
12.1.1.2 Only consider applications that pass through the eligibility criteria check gateway. This enables primary care commissioners to prioritise applications that demonstrate they have the greatest need, which in turn ensures that a GP contractor does not waste their time on completing and providing information when ultimately, primary care commissioners are unable to support their application.
12.1.1.3 Only reimburse amounts in accordance with directions 47 and 48, unless there are exceptional circumstances which justify reimbursement on another basis. Commissioners should be aware that fuel and electricity charges, buildings insurance costs, the cost of internal and external repairs, and the costs of plant, building and grounds maintenance are excluded for reimbursement under directions 47 and 48.
12.1.1.4 Make recommendations on applications that have passed through all gateways to the relevant commissioner part 2 Primary Care Commissioning Committee. Applications can take a considerable time to process, should they be subsequently approved, back claims will be with effect from the date that the original application was made.
12.1.1.5 Offer short-term financial support towards premises running costs and/or service charges to GP contractors where there is evidence that their practice expenses are significantly higher than the latest published averages, as a result of high service charge costs and other practice expenses. In this eventuality, a GP contractor must be prepared to put in place a clear action plan, demonstrating that over the next 12 months, it will optimise its income and reduce its expenditure. A further assessment as to whether a GP contractor should remain entitled to further financial support will be undertaken 1 year on by re-running the financial assistance model, subject to a GP contractor’s wish to continue to request such support.
12.1.1.6 Discontinue financial support to GP contractors towards premises running costs and/or service charges after a 12-month period, where the true cost pressure does not relate to service charge expenses. GP contractors can apply for further support under section 96 of the National Health Services Act 2006 (refer to the Primary care policy and guidance manual).
12.1.1.7 Have no direct involvement in managing service charge costs but will require evidence that GP contractors and landlords/head leaseholders have taken appropriate steps to mitigate costs. Steps taken by the incumbents may include but are not limited to: a formal meeting or correspondence with the landlord or head leaseholder during which the service charge costs were explained and justified. GP contractors should also seek assurance from the landlord/head leaseholder that the service charge costs demonstrate value for money and deliver soft and hard maintenance, in the interests of good estate management and following the principles within the Royal Institution of Chartered Surveyors (RICS)’ code of practice – service charges in commercial property. The current GP contractor should also show that they have analysed their own service expenditure to identify areas where costs can be reduced.
12.1.1.8 Have interest both in maintaining the viability of its practices and safeguarding taxpayer’s monies to ensure value for money is delivered.
12.1.1.9 Use the latest available GP earnings and expenses report currently published by NHS England to benchmark average PMS/GMS GP contractor’s earnings to expenses ratios, which are used as a yardstick to ensure fair and reasonable application.
12.1.1.10 Take into account changes in income and expenditure, advising GP contractors about any outlying (based on the above NHS England2 report) costs in the process.
12.1.1.11 Always use the average previous year’s annual service charge costs (where applicable) as the practice’s starting contribution to new service charge costs, should a case be made for service charge support. Whilst there is a provision to assume 40% of service charge cost is paid by a GP contractor in the event where no historical information is available, the model assesses financial assistance required by the GP contractor based on actual cost projections and expenses and income ratios.
12.1.1.12 Test a range of alternative inputs to its model to establish which variables provide the best match to enable the GP contractor to attain average PMS/GMS contract earnings.
In light of the number of variables that can impact upon a GP contractor’s ongoing need for financial support towards premises running costs and service charges, these would normally be reviewed on an annual basis, when the relevant information is available, reconciling costs back to the last review period.
12.1.2 GP contractors will:
12.1.2.1 Agree to full disclosure of income and expenditure on an open book and annual basis. Should GP contractors not wish to be party to an annual review, they will need to propose a one-off fixed term support package, which demonstrates a phasing out of financial assistance, taking into account the known variables.
12.1.2.2 Not seek to occupy an unreasonable amount of space, taking into account their potential list size; and undertake to share space to mitigate costs, wherever this is practicable.
12.1.2.3 Take responsibility for assessing the potential for growing their practice list and develop the associated trajectory over the relevant period.
12.1.2.4 Agree to negotiate and sign a lease at the earliest opportunity, whilst seeking assurance from the landlord/head leaseholder that the service charge costs being levied are fair and reasonable, in compliance with section 12.1.1.6.
12.1.2.5 Take responsibility for maximising their NHS income by providing GP services commissioned by local and national NHS and local authority commissioners within their sphere of competence, resources, and affordability, so that the burden of use of public monies for service charge assistance is reduced.
12.1.2.6 Take responsibility for minimising their practice expenditure by ensuring cost effectiveness and value for money spend.
12.1.2.7 Demonstrate through a clear action plan agreed with support from the LMC (as necessary), how they intend, over a reasonable period (deemed to be 12 months), to optimise their income and reduce expenditure, where there is evidence that their practice expenses are significantly higher than the latest published averages.
12.1.3 Landlords/head leaseholders will be expected to:
12.1.3.1 Ensure the proposed service charge costs being levied are fair and reasonable, and they have a clear strategy to drive down service costs; and provide associated evidence to their prospective tenant/occupier in accordance with the RICS’ code of practice – service charges in commercial property.
12.1.3.2 Enable space to be used flexibly to enable GP contractors to mitigate costs, where possible.
12.1.3.4 Allow GP contractors to procure their own services (such as cleaning) where it is practicable to do so, subject to the former providing assurance that their specification will comply with life cycle requirements.
12.1.4 Expectation management
12.1.4.1 Should there be evidence that a landlord is not prepared to fulfil the expectations detailed in 1.3.1 to 1.3.3, this will not, in principle, prejudice a GP contractor’s application for financial support towards premises running costs and service charges. However, it is likely to delay the processing of an application until the information required to complete it is available.
12.1.5 Evidence required to demonstrate application of principles
12.1.5.1 An expression of interest or application shall normally be considered when the steps identified in 1.5.1.1 to 1.5.1.4 have been evidenced:
12.1.5.2 Meetings and/or correspondence between the landlord/head leaseholder and the GP contractor which include full disclosure of soft FM costs backed up with supporting evidence.
12.1.5.3 Agreement that the footprint that the GP contractor occupies or wishes to occupy is sufficient to meet their current service provision and future potential provision.
12.1.5.4 Confirmation that key support service-related matters such as cleaning services have been discussed and agreed.
12.1.5.5 Evidence that the impact of procured soft financial model (FM) services has been discussed in the context of value for money.
12.2 The model
12.2.1 Eligibility criteria
12.2.1.1 Questions to help establish eligibility should be answered on tab 2 in annex 2 (financial model template).
12.2.1.2 Total practice expenses to total practice income (expressed as a percentage) for the most recent financial year must be greater than the published average 2015/16 expenses to earnings ratios for GP contractors in the UK for a similar contract type (see FMT, annex 2, tab 5). The expenses to earnings ratio is a measure of the proportion of an individual’s gross earnings that is consumed by business expenses. For ease of understanding it is expressed as a percentage throughout this report (refer to the latest GP earnings and expenses report). Note: “Full time and part time GPs are included. Figures are irrespective of working hours” (refer to the latest GP earnings and expenses report). “Earnings and expenses results relate to both NHS and private work. It is not possible to provide an NHS/private split using HMRC as a data source as most GPs submit a self-assessment tax return which contains information on all of their self-employment earnings while practising as a GP, but which cannot differentiate between NHS and private earnings. GPs can perform both NHS and private work both inside and outside of practice, including the NHS Out-of-Hours Service” (refer to the latest GP earnings and expenses report). Private income is identified as a very small percentage of average GP income – based on the England data collection “as a guide to NHS/private earning proportions, the average NHS superannuable income for GPMS contractor GPs was 94.8 per cent of income before tax in 2013/14” (refer to the latest GP earnings and expenses report) which is the latest year for which pensions data are available” (GP earnings and expenses 2015/16 by NHS England, published 13 September 2017, p.12). If the value of work being undertaken by a GP partner outside of their contractual commitment affects the total practice expenses to total practice income ratio, such that it is significantly greater than the relevant GMS, PMS or APMS benchmark ratio (as appropriate), NHS England reserves the right to exclude additional practice expenses relating to this (eg locum costs to cover GP partner’s practice sessions). The value of outside clinical work/advice should be included in the expenditure incurred by the practice. Primary care commissioners recognise that there may be circumstances that impact on the expenses/income ratio that could exclude a practice’s application for consideration for financial assistance towards service charges; these issues will always be evaluated on a case-by-case basis.
12.2.1.3 The practice should have had no serious contract breaches for any reason since 1 April 2013. The practice can make a statement for mitigation if they have had any serious contract breaches since 1 April 2013.
12.2.1.4 Should the above criteria not be met, or the practice has not yet provided acceptable explanations for mitigation, an application will not be considered any further.
12.2.2 Financial model template
Notes for completion of the template file can be found in tab 1 in the financial model template (FMT, annex 2).
12.2.2.1 For the purpose of this exercise, a contract is considered as a whole. In other words, where a practice operates from more than 1 site, the combined income and expenses should be entered on the template. Similarly, where 2 or more practices are merging, the estimated combined income and expenses of the new practice should be entered on the template.
12.2.2.2 The practice is required to populate the attached I&E template (income and expenditure – tab 3 in the FMT) declaring their income and expenditure for the most recent financial year, including full disclosure of service charge cost paid during the most recent financial year. Evidence of payment of service charges must be provided. If no service charges were paid, a statement is required stating the reasons why no service charge costs were paid during the most recent financial year. Applications where this applies will be evaluated on a case-by-case basis.
12.2.2.3 The practice must provide a breakdown of service charges which allows business rates, water and sewerage charges, and the collection and disposal of clinical waste to be identified. If the practice’s application includes an application for reimbursement of other amounts, the practice must distinguish them from fuel and electricity charges, building insurance costs, the costs of internal or external repairs, and plant building and grounds maintenance.
12.2.2.4 The practice must show baseline income separate from other income such as income received from QOF, enhanced services, non-NHS organisations, reimbursements, etc.
12.2.2.5 The practice income and expenditure will be compared with the published 2015/16 UK averages (tab 5 in the FMT) for GMS and PMS practices to determine if the practice is performing broadly in line with these averages. An adjustment may be made for service charges based on the information provided by the practice since the UK average for service charge cost is not available.
12.2.2.6 On the I&E template (tab 3 in the FMT), the practice should demonstrate through a clear action plan how it intends, over a reasonable period of time, as agreed with the commissioner, to optimise its income and reduce its expenditure, where applicable, to align broadly with the published UK averages for 2015/16 (tab 5 in the FMT) (or more recent when available).
12.2.2.7 On the service charge template (tab 4 in the FMT), the practice should further demonstrate how it plans to increase its share of the service charge cost and reduce the liability of the primary care commissioner to provide financial assistance. This can be done in fixed percentage/value increments each year or based on list growth or another plan tailored for the practice. The practice is advised to note the impact of its projections on its expenses to earnings ratios. Where a practice cannot increase its share of the service charge cost, it must give reasons why this is not possible. Note that the primary care commissioner’s liability for financial assistance for service charge support can never be higher than the total service charge cost to the practice.
12.2.2.8 The figures mentioned above will be reviewed on an annual basis in the interest of the practice, primary care commissioner as well as the taxpayer. This includes the income and expenditure, service charge cost as well as the comparison with UK averages where applicable. The projected reduction in primary care commissioner’s liability for financial assistance for service charge cost will also be assessed annually to evaluate whether it is viable or not for the practice to be responsible for a larger share, and ultimately 100% of the total service charge cost. The practice should notify the primary care commissioner of any significant changes and provide an updated FMT to enable the re-evaluation of financial assistance for service charge cost. If there are no significant changes, the practice must provide the primary care commissioner with proof of payment of the most recent years’ service charge costs in order to compare that with the FMT submitted previously. Primary care commissioners will reconsider financial assistance for service charge cost support to a practice if there are significant changes to the FMT as well as actual service charge costs.
12.2.2.9 Where a practice chooses not to disclose its income and expenditure information on an annual basis, it will need to propose a fixed term financial assistance package for service charge costs. The practice will still be required – in the first instance – to demonstrate that it meets the eligibility criteria to access financial assistance and must also provide proof of payment of the most recent years’ service charge costs (where applicable). The practice will need to demonstrate a reduction in required service charge support taking into account known variables such as changes in weighted list size, baseline price, other income, actual service charge costs, other expenditure, national averages and other variables that may impact the financial viability of the proposal. At the start of each financial year and while financial assistance is required, the practice must provide proof of payment of the most recent years’ service charge costs to the commissioner in order to compare that with the proposed financial assistance package, regardless of its agreement to a fixed term package. The commissioner will reconsider its financial assistance for service charge costs to the practice if there are significant changes to the proposed package and actual service charge costs. Financial assistance towards service charge costs will only be reimbursed based on actual service charge cost paid by the practice and not while there is a dispute between the practice and the landlord, and/or there is no lease in place and/or the service charge costs have not been agreed with the landlord following an increase in this cost.
12.3 Process flowchart
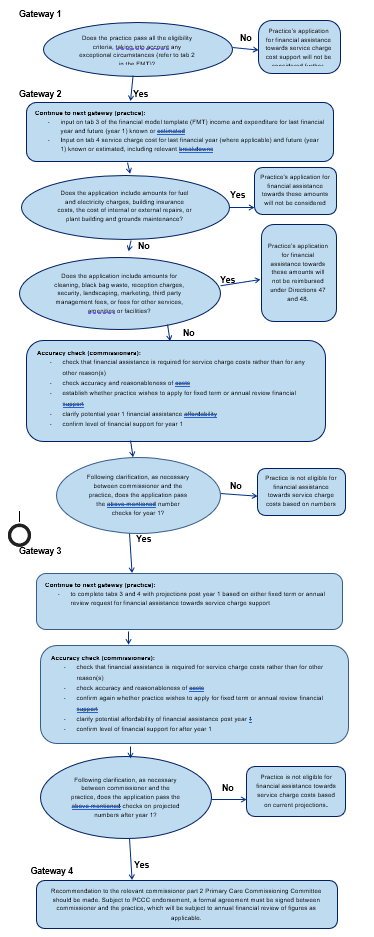
Annex 1: directions
Extract from NHS (GMS – premises costs) directions 2024
Payments in respect of running costs
47. – (1) Where–
(a) a contractor is in receipt of payments pursuant to this Part in respect of leasehold rental costs or borrowing costs, or by way of notional rent payments;
(b) the contractor actually and properly incurs the costs which are or relate to–
(i) business rates,
(ii) BID levies under the Local Government Act 2003(a),
(iii) water and sewage charges,
(iv) charges in respect of the collection and disposal of clinical waste, or
(v) a utilities and services charge which covers the matters in paragraph (2);
(c) those costs are not covered in other payments that the contractor is receiving pursuant to these Directions, and
(d) the contractor makes an application to NHS England for financial assistance towards meeting any or all of these costs,
subject to direction 48, NHS England must consider that application and, in appropriate cases (having regard, amongst other matters, to the budgetary targets it has set for itself), grant that application.
(2) The utilities and service charges in paragraph (1)(b)(v)-
(a) may include a service charge under a lease or a charge levied under separate arrangements made by a contractor which is an owner-occupier; and
(b) may include all or part of the service charge, depending on NHS England’s approval of both the costs included in the service charge and the basis on which the costs are apportioned to the contractor
(3) Where-
(a) NHS England grants an application made under paragraph (1) and makes a payment to the contractor in respect of that application: and
(b) the contractor subsequently receives a refund in respect of all or part of the costs referred to in paragraph (1)(b) from the body to whom the costs were paid, the amount of the refund is payable to NHS England no later than the day ending three months after the date of the contractor receiving the fund.
(4) Where-
(a) NHS England grants an application made under paragraph (1) and makes advance
Payments to the contractor in respect of that application based on the estimated
service charge costs;
(b) the contractor is subsequently required to pay additional service charge costs
following a service charge reconciliation to reflect actual service charge costs; and
(c) the contractor notifies NHS England within the period of months beginning with the
date on which the contractor paid the costs referred to in sub-paragraph (b), that it
has made those payments,
NHS England must reimburse the contractor with an amount equal to the difference
between the amount paid by NHS England and the actual amount paid by the contractor
for those costs.
Financial assistance towards certain elements of service charges
48. (1) In this direction, the “relevant charges” are those parts of a service charge payable
in respect of–
(a) fuel and electricity charges,
(b) insurance costs,
(c) costs of internal or external repairs, and
(d) plant, building and grounds maintenance costs,
(2) NHS England must deduct from any amount that it would otherwise be required to pay in
respect of an application of the type mentioned in direction 47 an amount calculated in
accordance with paragraph (3) by reference to the same time period as the period in
respect of which the service charge is payable.
(3) That amount is –
(a) where the amount of the relevant charges can be accurately determined, the amount
paid in respect of those charges;
(b) where the lease has been in existence for less than 12 months and the amount of the
relevant charges cannot be accurately determined, the estimate of those charges for the
first year of the lease; or
(c) where NHS England has no information as to the amount of those charges, 40% of the
amount which NHS England estimates as being the total yearly service charge.
(4) Where an application of the type mentioned in direction 47 has been made and the
service charge is payable in advance, NHS England must reimburse the contractor with
the amount paid by the contractor in respect of the charges referred to in paragraph
(1)(b) of that direction after deducting any element of those charges relating to relevant
charges.
(5) For the purposes of paragraph (4), the relevant charges are to be calculated in
accordance with paragraph (3).
13 Sub-contracting of Clinical services: assurance framework
13.1 Introduction
13.1.1 This framework was primarily developed to support commissioners’ assurance of proposals by a GMS contractor to expand into new areas across the country by sub-contracting clinical services to a separate company to deliver services to ‘out of area’ patients, both through the provision of ‘digital-first’ services and face-to-face consultations in sub-contractor’s premises located outside of the practice’s area.
13.1.2 The framework is particularly useful to commissioners when considering such proposals; however, it can be of use in relation to any proposal by a contractor to sub-contract clinical services.
13.1.3 The framework is provided as a resource to support commissioners and consists of:
- guidance on assuring sub-contracting of clinical services under GMS contracts
- annex A – assurance checklist
- annex B – mandatory contract terms regarding sub-contracting
The following are outside the scope of this framework:
- sub-contracting of non-clinical matters
- sub-contracting of out-of-hours services
- entering into a contract for services with a health care professional for the provision by that professional personally of clinical services
Guidance on assuring sub-contracting proposals
13.1.4 It can assist both commissioners in assuring proposals for sub-contracting, and providers in developing their proposals and addressing potential issues, to enter into preliminary discussions and co-operate with one another, prior to formally serving a notice of sub-contracting.
13.1.5 Doing so avoids the considerable time pressures associated with the 28-day period for commissioners to formally to object to a notice of sub-contracting under a GMS contract.
13.1.6 However, under the GMS contract, the contractor has the right to serve a notice of sub-contracting at any time. Where a contractor does so, commissioners must act rapidly to undertake assurance of the proposals and (where appropriate) serve any notice of objection within a 28-day period.
Step 1 – identify the relevant contract and terms
13.1.7 In all cases the commissioner should identify the relevant primary medical services contract in place with the contractor and review its terms regarding sub-contracting. These terms set out the respective rights and obligations of the parties in relation to sub-contracting and must be adhered to by both parties.
13.1.8 This guidance and the checklist focus upon GMS contracts only and reflect the mandatory terms regarding sub-contracts that must be included in all GMS contracts.
13.1.9 PMS and APMS contracts have fewer mandatory terms regarding sub-contracting and may also have bespoke sub-contracting arrangements agreed within the contract. Therefore, not all aspects of this guidance and checklist will apply to such contracts. See annex B for a summary of the mandatory terms for each type of contract and seek legal advice where required.
Step 2 – notice of sub-contracting
13.1.10 The contractor must give notice in writing of its intention to sub-contract as soon as reasonably practicable before the date on which the proposed sub-contract is intended to come into effect (‘notice of sub-contracting’).
13.1.11 Upon receipt of such a notice, the commissioner should check if it is valid. A valid notice must include:
- the name and address of the proposed sub-contractor
- the duration of the proposed sub-contract
- the services to be covered by the proposed sub-contract
- the address of any premises to be used for the provision of services under the proposed sub-contract
13.1.12 If the notice is valid, the commissioner should then calculate a period of 28 days beginning with the date on which the notice of sub-contracting was received. The last day of that 28-day period is the last date upon which the commissioner may serve a notice of objection (see step 5). The commissioner should take into account the notice provisions of the contract to ensure that the date is correctly calculated, and any such notice is served in time.
13.1.13 If the notice is invalid, the commissioner should advise the contractor of this and that the proposed sub-contract will be unlawful unless and until a valid notice of sub-contracting has been served. Upon receipt of a valid notice, the commissioner has a further 28 days to object starting on the date it was received.
Step 3 – notification of novel, contentious or repercussive proposals
13.1.14 The commissioner should take an initial view upon whether any of the following criteria are met:
- the sub-contracted services will be delivered wholly or partly via a ‘digital-first’ service (ie care delivery models through which a patient can receive the advice and treatment they need via online symptom checking and remote consultation)
- the sub-contracted services will be provided to ‘out of area’ patients (ie patients who reside outside of the practice area)
- the premises to be used for the provision of services under the proposed sub-contract are outside of the contractor’s practice area; or
- the proposed sub-contract is otherwise considered to be novel, contentious or repercussive
13.1.15 Where any of the above criteria are met, the commissioner should immediately notify its regional NHS England and Improvement primary care team. The purpose of this notification is to enable:
- monitoring of the rollout of such sub-contracting arrangements
- notification of commissioners affected by the proposed sub-contract
- provision of additional guidance and support to the commissioner, where appropriate
- in the case of a ICB commissioning primary medical services under delegated arrangements with NHS England, determining whether the decision requires additional approval by NHS England
13.1.16 In such cases, NHS England regional team will advise, having consulted with NHS England national primary care team, the commissioner of any additional procedures to be followed.
Step 4 – assurance of the proposed sub-contract
13.1.17 The commissioner must then assure the proposed sub-contract and decide:
- whether the proposed sub-contract is unlawful (ie not permitted under the GMS contract)
- whether there are any safety or financial grounds to object to the proposed sub-contract
13.1.18 Where the contractor has served a valid notice of sub-contracting, it is essential that this process is completed (and any notice of objection given) before the 28-day period ends (see step 2).
Unlawful sub-contracting
13.1.19 The contractor is not permitted to sub-contract clinical services unless:
- it has given notice in writing to the commissioner of its intention to sub-contract as soon as reasonably practicable before the date on which the proposed sub-contract is intended to come into effect (see step 2, above)
- it is satisfied that the sub-contractor has in force in relation to it an indemnity arrangement which provides appropriate cover
it has taken reasonable steps to satisfy itself that:
- it is reasonable in all the circumstances to sub-contract clinical matters; and
- the person to whom clinical matters are sub-contracted is qualified and competent to provide the service
- the sub-contractor would be able to meet the contractor’s obligations under the contract
- the sub-contract prohibits the sub-contractor from sub-contracting any of the clinical services that it has agreed with the contractor to provide under the sub-contract
13.1.20 The proposed sub-contract will also be unlawful if it involves the sub-contracting of essential services to a company or firm which is or was formed wholly or partly for the purpose of avoiding the restrictions on the sale of goodwill of a medical practice. Seek legal advice if this is a concern.
Objections on safety or financial grounds
13.1.21 The grounds of objection are that the sub-contract would:
- put the safety of the contractor’s patients at serious risk; or
- put NHS England at risk of material financial loss
13.1.22 These are the only grounds of objection available.
Assurance process
13.1.23 The assurance of the proposed sub-contract is at the discretion of the commissioner.
13.1.24 The assurance process should be proportionate and undertaken within the 28-day period to enable objections to be served if necessary.
13.1.25 What is proportionate in any particular case will depend upon the circumstances and the commissioner’s assessment of the potential safety, financial and compliance risks associated with the proposal. Proposals that have been identified as novel, contentious or repercussive under step 3 are likely to require the most detailed level of assurance.
13.1.26 Without prejudice to the discretion of commissioners, NHS England has prepared an assurance checklist which sets out a series of matters which could be interrogated as part of such an assurance process – see annex A.
Additional information
13.1.27 The commissioner may request further information relating to the proposed sub-contract as appears to it to be reasonable and the contractor must supply such information to the commissioner promptly.
13.1.28 This is particularly likely to apply where the contractor has not engaged with the commissioner in advance of giving notice of sub-contracting, as the commissioner is unlikely to have all of the information required to undertake an appropriate assurance exercise.
13.1.29 The 28-day period is not ‘paused’ when requests for information are made, therefore any requests for information should be made promptly to allow sufficient time to receive and scrutinise such information.
Decision
13.1.30 A decision on the above matters must be taken within the 28-day period based upon the information available at that time.
13.1.31 The decision should be taken in accordance with relevant decision-making processes and (in the case of an ICB commissioning primary medical services under delegated arrangements with NHS England) in accordance with the relevant delegation agreement.
Step 5 – implementation
No objections
13.1.32 If the commissioner considers that that the proposed sub-contract is permitted under the terms of the contract, and that there are no safety or financial grounds to object, no further formal steps are necessary. The contractor will be:
13.1.33 In these circumstances, the commissioner may indicate to the contractor that it does not presently have any objections, however it is recommended that the commissioner states that this is without prejudice to its rights under the contract, including to object to the sub-contract in future, where appropriate.
Unlawful sub-contracting
13.1.34 If the commissioner considers that the proposed sub-contract is unlawful (ie not permitted under the terms of the contract), it should notify the contractor of this in writing.
13.1.35 If the contractor nonetheless proceeds with the sub-contract, this should be treated as a breach of contract and appropriate contractual action should be taken. What action is appropriate will depend upon the circumstances and legal advice should be obtained if necessary.
Objection on safety or financial grounds
13.1.36 Where NHS England is satisfied that there are grounds to object on safety or financial grounds, the commissioner must give notice in writing of its objection to the sub-contract within the 28-day period (‘notice of objection’).
13.1.37 The notice must specify the specific grounds relied upon (see step 4) and include a statement of reasons for NHS England’s objections.
13.1.38 Where a valid notice of objection has been served on the contractor within the 28-day period, the contractor must not proceed with the sub-contract. If the contractor disagrees with the notice of objection, it must follow usual dispute resolution procedures.
13.1.39 If the contractor nonetheless proceeds with the sub-contract, this should be treated as a breach of contract and appropriate contractual action should be taken. What action is appropriate will depend upon the circumstances and legal advice should be obtained if necessary.
Step 6 – review
13.1.40 Where sub-contacting proceeds, commissioners should continue to monitor the arrangements. Where issues arise, appropriate contractual action should be taken. What action is appropriate will depend upon the circumstances and legal advice should be obtained if necessary.
13.1.41 In some cases, a proposed sub-contract may be unlawful or objected to on safety or financial grounds within the 28 day period, but is capable of being permitted following a further period of development and assurance of the proposal. If so, the commissioner may wish to schedule a future review of the decision to assess if any objections can be lifted.
13.2 GP and NHS provider (NHS trusts or foundation trusts) sub-contracting checklist
13.2.1 There are also various emerging arrangements in which NHS trusts or foundation trusts (or their subsidiary companies) are becoming involved in primary medical services contracts (including GMS contracts) through either:
- subcontracting of services
- contract award (PMS agreements and APMS contracts)
13.2.2 This (sub) section provides an overview of some key and emerging issues that commissioners may wish to assure themselves where such arrangements are proposed. It is structured into 4 parts:
- part A – issues that the NHS England and Improvement regional teams will need to consider, to ensure that its own statutory responsibilities are upheld
- part B – issues that an ICB would need to consider meeting its responsibilities
- part C – issues that would need to be considered by the NHS England and Improvement regional team or the ICB, depending on whether primary care commissioning responsibilities are delegated
- part D – issues on which the commissioner may need to seek assurance that the provider has considered
Part A: Issues for consideration by the NHS England and Improvement regional teams
Issue: responsible officers (RO)
The Medical Profession (Responsible Officers) Regulations 2010 establish the role of the ‘responsible officer’. Organisations with a responsibility to appoint a responsible officer include NHS England (for example, for an individual on the performers list) and organisations ‘designated’ under the regulations.
Those who wish to perform primary medical services on behalf of the NHS must generally be included in the national performers list (except in certain specified circumstances), and NHS England has a responsibility to provide a responsible officer for those on the performer’s list – this includes in instances where that person(s) on the performers list are employed by another organisation (such as a NHS trust or foundation trust) – this is likely to encapsulate the types of arrangements described given that they are performed under a GMS (sub)contract.
There may be circumstances in which it is appropriate for the NHS trust/foundation trust to provide a RO for someone providing primary medical services – for example, if they have employed an overseas GP who is not required to be on the performers list.
Considerations
There may be a risk of either:
- potential duplication between NHSE and providers – ie that both may provide a RO inappropriately; or
- that both the provider and NHSE may assume that the other party is providing the role
Action required:
NHS England should ensure its responsible officer (RO) responsibilities are upheld. In practice, NHS England regional/local teams should confirm which organisation is taking responsibility for appointing a responsible RO and check that each GP employed/operating the subcontract has a RO appointed.
Part B: Issues for consideration by the ICB
Issue: potential conflicts of interest
Commissioners are expected to manage any conflicts that may arise in relation to membership and decision-making.
Considerations
There is potential that a direct relationship between GPs and trusts/foundation trusts may raise additional conflicts of interest for decision-making. In particular, it is possible that GP practices affiliated with one NHS trust/foundation trust could become dominant within an ICB’s membership, and then potentially (dependant on its constitution), have an ability to influence other aspects of ICB policy which may benefit that trust. ICB may also need to consider and manage potential conflicts of interest in its governance and decision-making arrangements.
Action required
Commissioners should consider this issue and refer to NHS England’s Managing conflicts of interest guidance.
Part C: issues on which the commissioner may need to seek assurance that the provider has considered
Issue: following due process
There are set rules that govern the nature and circumstances in which primary medical services can be sub-contracted. It is worth noting that those rules differ slightly between GMS, PMS and APMS contractual frameworks. Further guidance on assuring sub-contracting arrangements is covered earlier in this chapter.
Those rules specify that where a GMS contractor wishes to subcontract clinical matters, they must give notice in writing to NHS England of its intention to subcontract as soon as is reasonably practicable before the date on which the proposed subcontract is intended to come into effect (note that there is an exception in relation to sub-contracting out of hours services).
The contractor must not proceed with a subcontract or, if the subcontract has already taken effect, the contractor must take steps to terminate it, where:
- NHS England gives notice in writing of its objection to the subcontract on the grounds that the sub-contract would:
(i) put the safety of patients at serious risk, or
(ii) put NHS England at risk of material financial loss
and notice is given by the NHS England before the end of the period of 28 days beginning with the date on which the NHS England received a notice from the contractor, or
- the subcontractor would be unable to meet the contractor’s obligations under the contract.
A statement of reasons for an objection must be provided and should set out a clear rationale for the decision.
Considerations
Commissioners must ensure that commissioned services continue to be delivered in accordance with the GMS contract.
In considering any such proposals to subcontract, commissioners will wish to consider whether the GMS contract will continue to be delivered to the nationally agreed terms and requirements. This may include seeking assurance of, for example, matters such as how services will be delivered in accordance with the GMS Contract and quality of care will be ensured.
Action required
Commissioners should consider whether the GMS contract, under sub-contract, will continue to be delivered to the nationally agreed requirements. This may include seeking assurance of, for example, matters such as how services will be delivered in accordance with the GMS Contract and quality of care will be ensured.
Commissioners should also identify whether, because of the particular delivery model, the GMS contract holder – and therefore the person to whom the ICB should be escalating performance management concerns – could have a conflict of interest with their responsibilities to the NHS trust/foundation trust. If any conflict is identified, the commissioner should ensure that measures are in place to manage them.
As part of the assurance process, commissioners may wish to seek confirmation from the contractor that they have updated their CQC registration, and to understand the detail of this registration.
Throughout the duration of any subcontracting arrangements, commissioners should continue to seek assurance about the delivery of the GMS contract through the lead contractor.
Part D: issues on which the commissioner may need to seek assurance that the provider has considered
There is a range of issues that contractors will need to properly consider and seek appropriate advice. These include but are not limited to:
- indemnity – for example, whether there is appropriate indemnity coverage for flexible use of workforce in the delivery of more integrated services
- implications for regulation – for example, to ensure that the provider’s registration with the Care Quality Commission has been appropriately updated where applicable
- pensions – in particular, staff employed by subcontractors are not able to access the NHS Pension Scheme (unless otherwise eligible in their own right, eg employees of trust/foundation trust). This is particularly an issue where primary care contracts are subcontracted to subsidiary companies with individuals becoming employed by the subsidiary rather than the trust/foundation trust directly
A sub-contractor does not automatically have access to the same digital services and support available to the practice. The practice will need to make a request to the ICB who will follow the guidelines in the GP IT operating model.
Part C – when things go wrong
1 Contract breaches, sanctions and terminations
1.1 Introduction
1.1.1 This policy chapter outlines the approach to be taken by the commissioner when a contract is considered to have been breached. Where processes differ with regards to GMS, PMS and APMS contracts, these are highlighted.
Primary Care Networks
While network services are delivered by the member practices, they are commissioned from the individual member practices.
Circumstances of non-delivery of network services may result in the issue of a breach notice, a remedial notice, contract sanction, or exceptionally lead the commissioner to consider termination and will be applied to individual member practices as those circumstances dictate or are clear, eg breach at network or practice population level.
1.1.2 Given that any decision to issue a breach or remedial notice, apply sanctions or terminate a contract or agreement can be challenged by the contractor under appeal, it is essential that the commissioner follows, and can demonstrate that it has followed, due process in investigating, communicating, and implementing actions in this respect and that the commissioner has acted fairly and reasonably throughout.
1.1.3 It is essential that the commissioner maintains thorough and accurate records of all communications and discussions in respect of all notices under this policy.
1.1.4 Commissioners should maintain accurate records of all breaches sanctions and terminations and will be required to demonstrate if requested, evidence of compliance, or otherwise support oversight of primary medical services commissioning arrangements. This may be for example via NHS England’s assurance arrangements or internal and external audit functions.
1.2 Contract breaches
Where the commissioner considers that a breach has occurred, there are a number of options on how to proceed. The commissioner can:
- take no action
- agree on an action with the contractor
- issue a remedial notice
- issue a breach notice
- apply a contract sanction
- terminate the contract
1.2.1 In many cases, it will be appropriate as a minimum, to serve a breach or remedial notice to formally document a breach as part of routine contract management. Where issues with a contractor then escalate, it is helpful if the pattern of breaches to date is already evidenced by appropriate breach and/or remedial notices. However, doing nothing or informally agreeing on an action with the contractor are options that the commissioner may consider appropriate for a very minor or technical breach. The commissioner should be aware of the implications of this decision, in that there will be no formal record of the breach to rely on as part of future contract management.
1.2.2 The following paragraphs set out the circumstances in which a remedial notice or a breach notice may be issued, a contract sanction may be applied, or the contract may be terminated with an explanation of the relevant process that the commissioner must follow.
1.2.3 The commissioner must ensure that, when issuing a remedial or breach notice, applying a contract sanction or terminating a contract, it follows the proper internal processes around the approval of the action, compliance with any standing orders and due consideration of all relevant factors in the decision-making process.
Delegated commissioning arrangements
The delegation agreement reserves primary medical services functions that relate to performers lists to NHS England. Circumstances that may result in the issue of a breach notice, a remedial notice, a contract sanction or may lead the commissioner to consider termination may relate to or include reference to performers lists matters. Where this is the case, the delegation agreement requires the ICB to work collaboratively with NHS England and support and assist NHS England to carry out its performers lists functions.
1.3 Remedial notices and breach notices
1.3.1 The GMS regulations, the PMS regulations and the APMS directions make a clear distinction between the process to be followed where a breach is capable of remedy and the process where a breach is not capable of remedy.
1.3.2 GMS/PMS – where a breach is capable of remedy, a remedial notice must be issued before the commissioner takes any other action under the contract (such as termination). Where a breach is not capable of remedy, a breach notice must be issued before the commissioner takes any other action under the contract (such as termination).
1.3.3 APMS – contracts are not required to contain provisions relating to remedial or breach notices. The NHS England standard alternative provider medical services contract does, however, contain these provisions. Where there is a potential breach of an APMS contract, the commissioner should always review the actual wording of the contract to ensure the right process is followed.
Remedial notice
1.3.4 Where a contractor has breached the contract and the breach is determined to be capable of remedy, the commissioner may issue a remedial notice to the contractor setting out the actions that must be taken to remedy the breach.
1.3.5 A flowchart highlighting the main steps that the commissioner should take when issuing a remedial notice is set out in annex 1.
1.3.6 The commissioner must issue a remedial notice before it takes any other action it is entitled to take under the contract, except where the breach relates to the rights of termination set out below. This is because the commissioner has a right to terminate the contract immediately for a breach of any of the circumstances set out below. These rights of termination are explained in more detail in paragraph 1.7 of this policy:
- provision of untrue information
- fitness to practise matters
- a serious risk to patient safety or risk of financial loss to NHS England
- unlawful sub-contracting
- in the case of a GMS contract, issues relating to the contractor’s eligibility to hold the contract
1.3.7 A breach capable of remedy is where the breach continues but the contractor could take action to stop the breach. Examples of breaches that may be capable of remedy include:
- failure to compile a practice leaflet
- failure to provide information to the commissioner
1.3.8 Where the breach creates a serious risk to patient safety, the commissioner can take more immediate action, regardless of whether the breach is capable of remedy or not. For further information on this, please refer to paragraph 1.7.32 of this policy.
1.3.9 Where the commissioner has determined that a breach is capable of remedy, the commissioner may, depending on the nature and circumstances of a breach take the following steps. These steps do not prejudice or delay a commissioner right to issue a remedial notice at any point before or during any of these steps being taken where the commissioner reasonably considers it is appropriate to do so:
- the commissioner should contact the contractor to discuss the breach and the action that they may be entitled to take, ie the issue of a remedial notice
- this discussion should provide the contractor with an opportunity to provide an explanation as to the circumstances that led to the breach. An accurate minute of any discussions should be retained
- the commissioner should review the evidence related to the breach including any information received during the discussion or in representations
- if the commissioner is satisfied that the matter is a breach which is capable of remedy, then the commissioner may issue a remedial notice to the contractor, requiring the contractor to remedy the breach
- it is important that when the steps above are undertaken, this is completed as quickly as is reasonably possible as long delays between the breach occurring, or the commissioner becoming aware of the breach, and the remedial notice being issued, could lead to an argument that the commissioner has accepted the breach and waived its right to take action. The commissioner will need to decide what action it considers would be reasonable to take before issuing a remedial notice considering the circumstances of an individual breach
A remedial notice must specify:
- details of the breach, which led to the remedial notice being issued and any evidence gathered in respect of the breach
- the steps the contractor must take in order to remedy the breach to the commissioner’s satisfaction
- the period in which the steps must be taken
- any arrangements for reviewing the matter to ensure that the requirements of the remedial notice have been met
- the actions that the commissioner shall take if the contractor fails to satisfactorily remedy the breach
1.3.10 The commissioner may wish to include in the remedial notice how the contractor may appeal against the decision to issue a remedial notice.
1.3.11 A template remedial notice is provided in annex 2. Where NHS England is the commissioner, the finalised remedial notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
[Annex 2 is provided as a template only and appropriate advice and support should be sought prior to issuing such a notice]
1.3.12 The period during which the steps to remedy the breach must be taken must not be less than 28 days from the date that notice is given, unless the commissioner is satisfied that a shorter period is necessary to protect the safety of the contractor’s patients or protect from material financial loss. In setting an appropriate remedial period, the commissioner should ensure that it would be possible for the breach to remedied within that timescale. For example, if a premises breach required major building works to remedy the issue, 28 days will not be reasonable if it seems likely that it would be impossible to meet this deadline.
1.3.13 The remedial notice must be delivered to the contractor in accordance with the notice provisions of the contract. This usually requires hand delivery or postal delivery (first class or registered post). Delivery of a notice by email may be permissible. The commissioner should review the relevant provisions to the contract to ensure proper delivery. Where the notice is hand delivered, the template receipt notice in annex 3 can be used.
1.3.14 The commissioner should ensure that arrangements are in place to follow up a remedial notice appropriately and in a timely fashion.
1.3.15 Where the commissioner is satisfied that the contractor has taken the required steps to remedy the breach within the required period, a letter should be issued to the contractor informing them that the terms of the remedial notice have been satisfied and that no further action will be taken at this stage. A template remedial notice satisfaction letter is provided in annex 4.
[This letter is provided as a template only and the commissioner should ensure that appropriate advice and support has been sought prior to issuing such a letter]
1.3.16 Where the commissioner is satisfied that the contractor has not taken the required steps to remedy the breach by the end of the required notice period, the commissioner may inform the contractor that they have failed to meet the terms of the remedial notice and that the commissioner may terminate the contract with effect from such date as the commissioner may specify in a further notice to the contractor.
1.3.17 Where the commissioner intends to terminate the contract, please refer to paragraphs 1.5 to 1.7 of this policy.
1.3.18 If, following the issue of a remedial notice, a contractor either repeats a breach that was the subject of a remedial notice or otherwise breaches the contract that results in a further remedial notice or a breach notice, then the commissioner has the right to terminate the contract by serving notice on the contractor.
1.3.19 For GMS and PMS, the right to terminate in paragraph 1.3.18 above must only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although check the contract wording. Where the commissioner intends to terminate the contract under this right, please refer to paragraph 1.7.46 of this policy.
1.3.20 If the contractor is in breach of any obligation and a remedial notice in respect of that default has been given to the contractor, the commissioner may withhold or deduct monies that would otherwise be payable under the contract in respect of that obligation which is the subject of the default.
Breach notice
1.3.21 Where the contractor has breached the contract and that breach is not capable of remedy, the commissioner may serve a breach notice on the contractor requiring the contractor not to repeat the breach.
1.3.22 A flowchart highlighting the main steps that the commissioner should take when issuing a breach notice is set out in annex 5.
1.3.23 Breach notices cannot be issued where the breach relates to the following rights of termination:
- provision of untrue information
- fitness to practice matters
- a serious risk to patient safety or risk of financial loss to NHS England
- unlawful sub-contracting
- in the case of a GMS contract, issues relating to the contractor’s eligibility to hold the contract
For further information on these rights of termination, please refer to paragraph 1.7.
1.3.24 A breach that is not capable of remedy is where a breach occurs but either does not continue prior to a notice being issued or there is no action that can be taken to remedy the breach.
1.3.25 Examples of breaches that are not capable of remedy include:
- a practice closing during its contracted opening times in the previous week with no access for the contractor’s registered patients to access essential services
- failure to store vaccines correctly and such vaccines have already been provided to patients
1.3.26 Where the breach creates a serious risk to patient safety, the commissioner can take more immediate action, regardless of whether the breach is capable of remedy or not. For further information on this, please refer to paragraph 1.7.32 of this policy.
1.3.27 Where the commissioner has determined that a breach is not capable of remedy, the commissioner may, depending on the nature and circumstances of a breach take the following steps. These steps do not prejudice or delay a commissioner right to issue a breach notice at any point before or during any of these steps being taken where the commissioner reasonably considers it is appropriate to do so:
- initially the commissioner should contact the contractor to discuss the breach and the action that they may be entitled to take, ie the issue of a breach notice. This does not prejudice or delay a commissioner’s right to issue a breach notice
- the discussion will afford the contractor the opportunity to provide an explanation as to the circumstances that led to the breach and this discussion should be recorded accurately in writing
- the commissioner should review the evidence related to the breach including any information received during the discussion or in representations
- if the commissioner is satisfied that the matter is a breach which is not capable of remedy, then the commissioner may issue a breach notice to the contractor, requiring the contractor not to repeat the breach
The breach notice must specify:
- details of the breach
- the requirement that the contractor must not repeat the breach again
- the consequences of the contractor further breaching the contract
1.3.28 A template breach notice is provided in Annex 6. Where NHS England is the commissioner, the finalised breach notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, The ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
1.3.29 The breach notice must be delivered to the contractor in accordance with the notice provisions of the contract. This usually requires hand delivery or postal delivery (first class or registered post). Delivery of a notice by email may be permissible. The commissioner should review the relevant provisions to the contract to ensure proper delivery. Where the notice is hand delivered, the template receipt notice in annex 3 can be used.
1.3.30 If, following the issue of a breach notice, a contractor either repeats a breach that was the subject of a breach notice or otherwise breaches the contract that results in a further remedial notice or a breach notice, then the commissioner has the right to terminate the contract by serving notice on the contractor.
1.3.31 For GMS and PMS, this right to terminate can only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although check the contract wording. Where the commissioner intends to terminate the contract under this right, please refer to paragraph 1.7.46 of this policy.
1.3.32 If the contractor is in breach of any obligation and a breach notice has been issued, the commissioner may withhold or deduct monies that would otherwise be payable under the contract in respect of that obligation.
1.3.33 The commissioner should retain and be able to report on all contractual notices issued in any financial year to support local and national assurance arrangements. A template notice return is set out Annex 11 (see also 1.4):
1.4 Contract sanctions
1.4.1 GMS/PMS – the commissioner must follow the process set out in this section. PMS agreements refer to “agreement sanctions” rather than contract sanctions. Reference to contract sanctions in this policy should be read as including reference to agreement sanctions.
1.4.2 APMS – APMS contracts are not required to contain provisions relating to contract sanctions. The NHS England standard alternative provider medical services contract does not contain references to contract sanctions. The commissioner must check the relevant contract to determine whether contract sanctions can be applied.
1.4.3 Contract sanctions must not be applied to a contract unless the commissioner has the right to terminate. Where contract sanctions are applied, this is instead of terminating the contract. The commissioner cannot apply contract sanctions and later decide to terminate the contract based on the breach that triggered the contract sanction.
1.4.4 The circumstances in which the commissioner may apply contract sanctions are those circumstances set out below where a right of termination arises. Please refer to the relevant right of termination in paragraph 1.7 for further information on how these rights of termination arise:
- provision of untrue information
- fitness to practice matters
- where there is a serious risk to patient safety or NHS England is at risk of material financial loss
- where the commissioner is satisfied that the contractor has not taken the steps required by a remedial notice to remedy a breach within the required period
- where, after a remedial notice or breach notice has been issued, the contractor
- repeats a breach that was the subject of a remedial notice or a breach notice; or otherwise breaches the contract resulting in a further remedial notice or breach notice
- where the contractor carries on business detrimental to the contract
- for GMS contracts only, where changes in the membership of the partnership are likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform obligations under the contract
1.4.5 Contract sanctions must not be applied if they terminate or suspend any obligation that relates to essential services.
Contract sanctions may involve:
termination of specified reciprocal obligations
suspension of specified reciprocal obligations for a period of up to 6 months
withholding or deducting monies otherwise payable under the contract
1.4.6 The choice of which contract sanction to use would ordinarily depend on the nature of the breach, or cumulative effect, and what is felt to be the most appropriate and proportionate action in those circumstances. For example, if the breaches have occurred in relation to a specific service element under the contract, it might be most appropriate to move to terminate that specific service, such as minor surgery.
1.4.7 Where the commissioner is considering imposing a contract sanction and the contractor has a GMS contract, it is a statutory requirement that the commissioner consults the relevant LMC before it imposes the contract sanction, where it is reasonably practicable to do so. There is no such statutory requirement in respect of PMS or APMS contracts and the commissioner should ensure it considers any relevant wording in the contract.
1.4.8 Where the commissioner decides that the most appropriate sanction would be to withhold or deduct monies, this must be calculated to establish a consistent, fair and measured approach. Annex 7 provides further information on calculating a financial contract sanction.
1.4.9 Where the commissioner decides to impose a contract sanction, the commissioner must issue a notice of its intent to apply a sanction to the contractor which must include:
the nature of the sanction to be applied
if withholding or deducting monies, how this has been calculated and the duration of any such sanction
if services are to be terminated, which services and from what date
if a suspension of specified reciprocal obligations under the contract or agreement, the period of that suspension and its end date
an explanation of the effect of the imposition of the contract sanction
the contractor’s right to appeal the decision to apply a contract sanction
1.4.10 A template contract sanctions notice is provided in Annex 8. Where NHS England is the commissioner, the finalised contract sanction notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
[Annex 8 is provided as a template only and appropriate advice and support should be sought prior to issuing such a notice]
1.4.11 The date that the contract sanction takes effect must not be until at least 28 days after the notice was served unless the commissioner is satisfied that it is necessary to impose the contract sanction earlier to protect the safety of patients or protect from material financial loss.
1.4.12 Where a contract sanction is imposed, the commissioner can charge the contractor reasonable administration costs of imposing the contract sanction.
1.4.13 After imposing the contract sanction on a contractor with a GMS contract, it is a statutory requirement for the commissioner to, as soon as reasonably practicable, notify the relevant LMC in writing of the contract sanction imposed. There is no such statutory requirement in respect of PMS or APMS contracts and the commissioner should ensure it considers any relevant wording in the contract.
1.4.14 If the contractor disputes the imposition of a contract sanction, the commissioner must not impose the contract sanction until the dispute has been determined unless the contract sanction is necessary to protect the safety of patients or protect from material financial loss.
1.4.15 Where a dispute arises in relation to the imposition of contract sanctions, please refer to the chapter on managing disputes.
1.4.16 The commissioner should ensure that arrangements are in place to monitor the contractor’s compliance with a contract sanction notice.
1.4.17 The commissioner should retain and be able to report on all contractual sanctions issued in any financial year to support any local and national assurance arrangements. A template notice return is set out annex 11 (see also 1.4).
1.5 Termination
1.5.1 Termination is a very significant action to take both on the part of the commissioner and the contractor and is an area of high risk for both parties in respect of financial impact and continuity of services. Where the commissioner considers that a termination notice may be issued, the commissioner should seek legal advice early in the process to confirm the appropriateness and lawfulness of taking such a step. It is essential that the commissioner maintains thorough and accurate records of all communications and discussions in respect of all notices.
1.5.2 Contractors have the right to appeal so it is essential that the commissioner follows and can demonstrate that they have followed due process in investigating, communicating and implementing actions leading to termination.
1.5.3 It is essential that prior to moving to terminate a contract, the commissioner is satisfied that they are fully within their rights to do so.
1.5.4 Legislation sets out certain rights of termination that are required to be in each type of primary medical contract. These mandatory termination rights are set out below and explained more fully in paragraph 1.7. Where the termination relates to a matter that is contained within an alternative policy, this is highlighted.
1.5.5 GMS/PMS may only be terminated using mandatory termination rights. An APMS contract may contain additional termination rights. The commissioner should consider the relevant contract to ensure it is fully aware of all termination rights.
1.5.6 GMS / PMS – The following circumstances relating to rights of termination are required to be in GMS and PMS contracts:
death of a contractor
contractor serving notice
late payment
provision of untrue information
fitness to practice issues
patient safety
material financial loss
unlawful sub-contracting
remedial notices and breach notices
carrying on business detrimental to the contract
1.5.7 GMS – GMS contracts are required to contain additional rights of termination relating to:
breach of regulation 4 (conditions relating solely to medical practitioners) of the GMS regulations
certain partnership matters
1.5.8 PMS – PMS agreements are required to contain additional rights of termination relating to:
commissioner serving notice
contractor’s exercise of the right to a GMS contract
agreement of the parties
1.5.9 APMS – The following circumstances relating to rights of termination are required to be in APMS contracts:
death of a contractor
provision of untrue information
fitness to practice issues
patient safety
material financial loss
unlawful sub-contracting
1.5.10 APMS – APMS contracts are likely to have further rights of termination. Where the commissioner wishes to terminate for a reason other than those set out in paragraph 1.5.9 above, the commissioner must review the contract to determine if any further rights of termination apply.
1.5.11 Contracts may also terminate by:
- reaching their natural end dates, without the need for termination notice (in which case, please refer to the chapter on practice closedown for more information); or
- retirement of the contractor (in which case, please refer to the chapter on contract variation)
1.5.12 Where the commissioner has considered all the relevant factors and has decided to proceed with termination, it must send a termination notice to the contractor, which is provided in a template at Annex 9.
1.5.13 Where NHS England is the commissioner, the finalised termination notice should be signed off by the director of commissioning operations or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
1.5.14 For GMS and PMS contracts, where the termination relates to:
provision of untrue information
fitness to practice issues
patient safety
material financial loss
remedial notices and breach notices
for GMS agreements
certain partnership matters
for PMS agreements
carrying on business detrimental to the agreement
The notice usually specifies a date on which the contract terminates that is not less than 28 days after the date on which the commissioner has served the notice on the contractor. The commissioner may state a date less than 28 days where this is necessary to protect the safety of the contractor’s patients or protect from material financial loss. APMS contracts are not required to contain any such provisions and the commissioner should consider the wording of the particular APMS contract.
1.5.15 Where the contractor disputes the commissioner’s decision to terminate the contract, the contractor may invoke the NHS dispute resolution procedure. In such circumstances, the commissioner should refer to the chapter on managing disputes.
1.5.16 The commissioner should retain and be able to report on all termination notices issued in any financial year to support local and national assurance arrangements. A template notice return is set out Annex 11 (see also 1.4).
1.6 Key considerations on termination
1.6.1 The commissioner must establish that grounds exist under the terms of the contract to terminate. The commissioner must follow due process and investigation of the facts and provide the contractor with the opportunity to provide a response to allegations, wherever possible.
1.6.2 A flowchart highlighting the main steps that the commissioner should take when issuing a termination notice is set out in Annex 10.
1.6.3 The commissioner must consider all relevant information available and decide on the appropriate course of action and whether the contract should be terminated.
1.6.4 Apart from considerations regarding whether the right to terminate arises, there are a number of common factors that the commissioner should consider when termination is a proposed course of action. These factors are set out below.
1.6.5 This list is not exhaustive and there are likely to be other issues that need due consideration under these provisions. These considerations will also apply following the sudden death of a contractor (see the chapter on the death of a contractor) and in some part on the closure of a branch surgery (see the chapter on contract variations).
Continuity of service provision
1.6.6 NHS England has a statutory duty to ensure the continuity of provision of primary care services. Termination of existing service provision may result in some persons not being able to access primary care services. The commissioner must therefore consider how this duty will be discharged if it decides to terminate the contract. This should be considered as soon as the commissioner starts to think about terminating.
1.6.7 If the commissioner envisages that a new contract will be entered into with a provider, the commissioner must consider how to procure that contract and to ensure it is in accordance with procurement law and any procurement protocol issued by NHS England.
PMS to GMS
1.6.8 PMS agreements provide a right for certain contractors to request to enter into a GMS contract. Such a request can only be refused where the contractor fails to meet the conditions set out in the PMS regulations.
1.6.9 For further information on this, please refer to the chapter on managing a PMS contractor’s right to a GMS contract.
General duties
1.6.10 NHS England has a number of statutory duties relating to the exercise of its functions including reducing health inequalities and public involvement. The commissioner must ensure that its actions in terminating a contract and any consequential actions ensure compliance with these duties. In an urgent situation, it may be necessary to balance the duty to involve with the public interest in maintaining continuity of care and protecting the health, safety and welfare of patients or staff. Please refer to the full chapter on general duties for further information.
1.6.11 NHS England has set out its plans as to how it intends to involve the public in the following publications:
The statement of arrangements and guidance on patient and public participation in commissioning
The framework for patient and public participation in primary care commissioning
LMC consultation (GMS contracts)
1.6.12 For GMS contracts, the commissioner must consult the LMC for the area in which the contractor provides services where the commissioner is considering:
terminating the contract
which alternative notice to issue where there is a right to terminate for unlawful sub-contracting
imposing a contract sanction
1.6.13 Whether or not the LMC has been consulted, whenever the commissioner imposes a contract sanction or terminates a GMS contract, the commissioner must as soon as reasonably practicable, notify the relevant LMC in writing of the sanction or termination. PMS and APMS contracts are not required to contain such provisions. The commissioner should review the relevant contract to determine whether any requirement has been included.
Premises
1.6.14 The commissioner should ascertain who owns the premises and what arrangements apply to the premises. Where the outgoing contractor owns the premises, a future service provider may not be able to use those premises for the delivery of services. The commissioner should consider what arrangements need to be put in place to ensure continued service provision. Commissioner should also ensure they consider any premises cost directions or guidance published by NHS England in relation to premises.
TUPE
1.6.15 The commissioner should consider the impact of termination on the staff currently employed under the terminating contract. Where a new contract is entered into with a new provider, TUPE may apply to transfer the staff to the new provider.
1.6.16 TUPE can be complex, risky and time consuming for any incoming provider and is likely to have a financial impact on the cost of any service. The commissioner should consider whether the potential for TUPE to apply may be considered a significant risk to any incoming provider.
Equipment
1.6.17 All equipment, including associated software, issued through GP IT are owned by NHS England and these are being managed on its behalf by ICBs as responsible commissioners of GP IT services. Arrangements should be put in place to retrieve this equipment, together with other kits issued by the ICB, to ensure it is available to a future service provider.
Patient lists – see also the PCSE website
1.6.18 Patients have a right of choice meaning the commissioner must not routinely transfer all of the registered patients to an alternative provider. Patients should be provided with a detailed list of other local practices that are currently accepting new patients and offered the opportunity to register with one of them.
1.6.19 The commissioner should consider what steps will be taken in regard to patients who have not registered elsewhere at the end of the contract. It is often the case that the majority will voluntarily seek alternative registration; however, there are usually a number of patients who do not, some of whom may no longer be resident in the UK or simply moved within the UK and not changed their address details at the practice and others who have not yet chosen an alternative provider. Some may have died. In these circumstances, the commissioner must be clear on the process of dispersal or allocation that they will follow in order to avoid the risk of challenge from other local providers. Please refer to the chapters on planned and unplanned closure for more information.
Patient records – see also the PCSE website
1.6.20 The commissioner should consider management of NHS patient paper records (Lloyd George notes) and any subsequent clinical mail – it is very likely that the contractor has retained a significant number of patient paper records both in the reception area and often stored elsewhere in the practice premises, including loft spaces and store cupboards. The commissioner must be able to securely retrieve these records and communications, having full regard of data protection and confidentiality in order that these can be distributed accordingly to any providers or returned to central storage. The contractor (or their representative) is responsible for any non-NHS patient or client record, though agreement may be reached with the commissioner to manage (dispose of) any confidential information on their behalf. Please refer to the chapters on planned and unplanned closure for more information.
Prescriptions
1.6.21 The commissioner should consider prescription pads, electronic prescriptions and any uncollected completed prescriptions – these will also need to be retrieved and dealt with accordingly. The commissioner may wish to decide on a specified age of a current prescription (such as 1 month) and make appropriate arrangements for the handling of these and disposal of any that are older – see also the PCSE website.
Drugs and medicines
1.6.22 The commissioner should consider practice held drugs – these will need to be disposed of but are technically likely to be owned by the contractor whose contract is terminating. The commissioner should seek assurances about the safe and effective disposal of such drugs.
1.7 Rights of termination
Death of a contractor
1.7.1 Please refer to the chapter on the death of a contractor for further information.
Termination where both parties agree
1.7.2 PMS agreements are required to contain a provision stating that both parties may agree to terminate a contract. Although GMS or APMS contracts are not required to contain such a provision, all types of contracts may be terminated where both parties agree.
1.7.3 Where the parties agree to terminate, the parties must agree on the date from which termination will take place and any further terms relating to the termination. Before agreeing on the termination date, the commissioner should ensure any proposed timescale allows the commissioner to consider any other factors or actions that may be required prior to termination.
1.7.4 The contractor party may be composed of more than 1 person. The commissioner must agree to the same termination arrangements with all persons that constitute the contractor.
1.7.5 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to the chapter covering general duties of NHS England.
Termination where the contractor serves notice
1.7.6 GMS and PMS contracts can be terminated by the contractor by serving notice in writing at any time. APMS contracts may also contain this right of termination.
1.7.7 Where a contractor serves notice to terminate a GMS contract, it shall terminate 6 months after the date on which the notice is served, except where the contractor is an individual medical practitioner in which case the contract shall terminate 3 months after the date on which the notice is served.
1.7.8 If the date on which the GMS contract will terminate is not the last calendar day of a month, the contract shall instead terminate on the last calendar day of the month in which the termination date falls.
1.7.9 Where a contractor serves notice to terminate a PMS agreement, the period of notice shall not be less than six months (unless both parties agree in which case, please refer to paragraph 1.7.2 to 1.7.5 – termination where both parties agree).
1.7.10 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.100.
Termination where the commissioner serves notice
1.7.11 PMS agreements can be terminated by the commissioner by serving notice in writing at any time, without needing to establish any breach by the contractor. APMS contracts may also contain this right of termination.
1.7.12 Where the commissioner serves this type of notice to terminate a PMS agreement, the period of notice shall not be less than 6 months (unless both parties agree in which case, please refer to paragraph 1.7.2 – termination where both parties agree). Commissioners should bear in mind the right of some PMS contractors to request a GMS contract. For further information on this, please refer to the chapter on managing a PMS contractor’s right to a GMS contract.
1.7.13 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 1.6.10.
1.7.14 GMS contracts are usually contracts in perpetuity without any right for the commissioner to terminate on notice.
Termination where the contractor exercises the right to a GMS contract
1.7.15 Please refer to the chapter on managing a PMS contractor’s right to a GMS contract for further information.
Termination due to late payment
1.7.16 The contractor may give notice in writing to the commissioner if the commissioner has failed to make any payment due to the contractor under the contract. If the commissioner has failed to make any such payment within 28 days of the notice, the contractor may terminate the contract by a further written notice.
1.7.17 Where the NHS dispute resolution procedure has been invoked by the commissioner, within 28 days of the initial notice, the contractor may not terminate the contract until either the NHS dispute resolution determination allows termination or the commissioner ceases to pursue the NHS dispute resolution process.
1.7.18 For further information on the NHS dispute resolution process, please refer to the chapter on managing disputes.
1.7.19 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination for provision of untrue information
1.7.20 The commissioner may serve notice to terminate the contract immediately (or from any date set out in the notice) if, after the contract has been entered into, it comes to the attention of the commissioner that written information provided to the commissioner:
before the contract was entered into; or
for GMS contracts, pursuant to paragraph 50(1)(a) or (b) or 51(1) of schedule 3 of the GMS regulations; or
for PMS agreements, pursuant to paragraph 46(1)(a) or (b) of schedule 2 of the PMS regulations,
in relation to:
for GMS contracts, regulations 5 and 6 of the GMS regulations
for PMS agreements, regulation 5 of the PMS regulations; and
for APMS contracts, direction 6 of the APMS directions,
was, when given, untrue or inaccurate in a material respect
1.7.21 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to paragraph 1.6.12 of this chapter and the full chapter on general duties of NHS England.
Termination due to fitness to practice issues
1.7.22 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from any date set out in the notice) where a person connected with the contract (such as a medical practitioner, a partnership, a company or a director) falls within any circumstances set out in the relevant regulations/directions. Those circumstances include where the person:
is disqualified from practising by a licensing body
has been convicted of certain offences
has been adjudged bankrupt
has been subject to a disqualification under the Company Director Disqualification Act 1986
The full list of circumstances is set out in the relevant law for GMS contracts, PMS agreements and APMS contracts at:
GMS regulations 2015, schedule 3, paragraph 67
PMS regulations 2015, schedule 2, paragraph 58
Direction 7(2)(q) of the Alternative provider medical services directions (2022)
1.7.23 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination where there is a serious risk to patient safety
1.7.24 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from such date set out in the notice) where the contractor has breached the contract and, as a result of that breach, the safety of the contractor’s patients is at serious risk if the contract is not terminated.
1.7.25 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination where there is a material financial loss
1.7.26 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from such date set out in the notice) where the contractor’s financial situation is such that the commissioner considers that NHS England is at risk of material financial loss.
1.7.27 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination due to unlawful sub-contracting
1.7.28 The Commissioner will have a right of termination where it comes to the commissioner’s attention that the contractor has sub-contracted any of its rights or duties under the agreement in relation to the provision of essential services to a company or firm:
owned wholly or partly by the contractor, or by any former or current employee of, or partner or shareholder in the contractor
formed by or on behalf of the contractor, or from which it derives or may derive a pecuniary benefit
formed by or on behalf of a former or current employee of, or partner or shareholder in, the contractor, or from which such a person derives or may derive a pecuniary benefit,
where that company or firm is or was formed wholly or partly for the purpose of avoiding the restrictions on the sale of the goodwill of a medical practice in section 54 of the NHS Act or any regulations made wholly or partly under that section.
1.7.29 Where this occurs, the commissioner may serve notice in writing on the contractor terminating the contract immediately or instructing the contractor to terminate the relevant sub-contract.
1.7.30 It is a requirement under GMS contracts that, whenever reasonably practicable to do so, the commissioner must consult with the relevant LMC when considering which alternative notice to issue (for further information on LMC consultation requirements, refer to paragraph 1.6.122). PMS and APMS contracts are not required to contain such provisions. The commissioner should review the relevant contract to determine whether any requirement has been included.
1.7.31 If the contractor fails to terminate the sub-contract, the commissioner may serve a notice in writing on the contractor terminating the contract immediately.
1.7.32 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination relating to remedial notices and breach notices
1.7.33 The commissioner has a right to terminate the contract where the commissioner is satisfied that the contractor has not taken the required steps to remedy the breach by the end of the required period as stated in the remedial notice.
1.7.34 The commissioner has a further right of termination where, following the issue of a remedial notice or breach notice, a contractor:
repeats a breach that was the subject of a remedial notice or breach notice
otherwise breaches the contract that results in a further remedial notice or breach notice
1.7.35 The further breach must have occurred after the breach which was the subject of the remedial notice or breach notice. The commissioner may intend to issue a further remedial notice or breach notice for a breach that occurred prior to the original breach with the need to investigate or gather information delaying the issue of the notice. In these circumstances, the commissioner cannot then rely on this right of termination as the further breach did not occur following the issue of the original remedial notice or breach notice.
1.7.36 For GMS and PMS, this further right to terminate can only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although check the contract wording.
1.7.37 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination due to the contractor carrying on business detrimental to the contract
1.7.38 For GMS and PMS, where the contractor is a company that is carrying on business which the commissioner considers is detrimental to the contractor performance of the contract, the commissioner may give notice to the contractor requiring that it ceases carrying on the relevant business within a specified period (which must not be less than 28 days from the date the notice was given). This termination right does not have to be included in an APMS contract so please check the specific contract to see whether it is included.
1.7.39 Where the contractor has not satisfied the commissioner that it has ceased carrying on the business by the end of the notice period, the commissioner may by further written notice terminate the contract immediately (or from such date set out in the notice).
1.7.40 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
Termination due to partnership matters
1.7.41 A commissioner has a right to terminate a GMS contract where:
the contractor is two or more persons practising in partnership;
where one or more partners have left the practice during the contract; and
if the commissioner reasonably considers that the changes in the membership of the partnership are likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform its obligations under the contract
1.7.42 Where this occurs, the commissioner may terminate the contract by notice in writing on such date as is set out in the notice. The notice must contain the commissioner’s reasons for considering that the change in the membership of the partnership is likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform its obligations under the contract.
1.7.43 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
1.7.44 Termination due to breach of regulation 5
1.7.45 Regulation 5 sets out conditions that the contractor must satisfy in order to enter into a GMS contract. There are a number of rights of termination relating to these conditions, which can be found at:
GMS regulations 2015, schedule 3, paragraph 65
1.7.46 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to paragraph 1.6.10 of this chapter and also the full chapter on general duties of NHS England.
1.8 Consequences of termination
1.8.1 Contracts usually contain certain obligations on both parties on termination of the contract. The GMS regulations, PMS regulations and APMS directions do not set out any requirements for primary care contracts to contain such provision but the Standard GMS Contract contains a number of obligations including provisions relating to:
- co-operation in dealing with any outstanding matters
- delivering up property owned by the other party
- carrying out a financial reconciliation
1.8.2 It is likely that PMS and APMS contracts will contain similar provisions. The commissioner should consider the relevant contract to determine what obligations are set out on termination.
1.9 Dealing with Care Quality Commission (CQC) issues
1.9.1 Commissioners may become aware of potential contract breaches when the CQC takes action following an inspection. CQC action may include suspending registration or cancelling registration completely. Whenever the commissioner becomes aware of issues identified and/or action taken by the CQC, it needs to consider those issues to see if any contractual action should be taken too.
1.9.2 Where evidence from the CQC’s findings and/or any further investigation by the commissioner identifies any breach(es) of contract, the commissioner should work through this chapter in the usual way to determine what steps to take. Often, CQC action will highlight a number of breaches, and this may result in several breach or remedial notices being served.
1.9.3 In some cases, the issues identified may be so significant that it is appropriate to consider termination of the contract. In very serious cases, it may be possible to move straight to termination, if an appropriate termination right arises. The position can be complex, particularly where for example a suspension has removed any immediate risk to patient safety and the contractor has been given a period of time by the CQC to address the issues. In those cases, it may be appropriate to wait and see whether the contractor complies with the CQC’s requirements, rather than moving straight to termination. Commissioners should seek legal advice if they are unsure how to proceed.
1.9.4 Issues identified by the CQC will sometimes form part of a wider pattern of problems under the contract, in which case the commissioner should consider the full range of problems in deciding appropriate next steps.
1.9.5 During any period of suspension by the CQC, the commissioner will need to ensure that the patients of that practice are able to access primary medical services elsewhere. It may be that the cost of any caretaking arrangement can be partly off-set by appropriate deductions under any breach or remedial notice being served in relation to the issues leading to suspension (see paragraphs 1.3.20 and 1.3.33 of this policy).
1.9.6 If a contractor’s CQC registration is cancelled, they will not be able to provide any services and the commissioner will need to terminate the contract. The commissioner should, however, be aware that the cancellation process can take time and that there is an appeal period following cancellation. Cancellation should not be relied on as final until that appeal period has expired, or any appeal has been determined. See the chapter on unplanned/unscheduled closedown for further information.
2 Unplanned/unscheduled and unavoidable practice closedown
2.1 Introduction
2.1.1 When a GP Practice closes at short notice, it is important that commissioners respond and act in a timely way. Such closures may be as result of actions by the CQC, for example voluntary closure in response to an adverse inspection or cancellation of the practice’s registration, or due to the sudden inability of a provider to continue providing a service for some other reason such as bankruptcy.
2.1.2 Furthermore, it is critical that the management and transfer of patient records (both paper and digital) are undertaken in a secure and robust manner. It is important that adherence to all applicable information governance, records management and data protection regulations and data protection principals are maintained throughout this process.
2.2 Scope
2.2.1 This guidance clarifies the role of the commissioner and the engagement required with patients and any partner organisations (eg NHS England or CQC). This chapter is intended as guidance with which commissioners can work, with 4 fundamental principles at the core:
- The needs of the registered patients must be at the heart of all decision and actions.
- In many cases taking preventive action in conjunction with support could be a preferable option to closing a practice.
- In circumstances where this chapter applies (eg a closure is unavoidable or in the best interests of patients), all partners and stakeholders should know what to do, when and how, and work effectively together to minimise any disruption to patients and services.
- Effective communication must be maintained throughout with patients and their families and carers and with other partners (eg PPGs/LMCs/Healthwatch).
2.3 Roles and responsibilities
Commissioners
2.3.1 The commissioner will take the lead in the following actions:
- Ensure appropriate interim measures are put in place (eg a caretaker GP) to keep people safe after the identification of concerns or issues or at the very latest, the point it is informed of the closure.
- Establish a team with specialist skills to oversee the closure, including contracting and communications staff, and lead on arranging meetings/consultations with any partners.
- Establish a task and finish group to oversee the process.
- Co-ordinate assessments of the practices’ registered list to ascertain patient needs and preferences. This should be completed by individuals with the relevant skills and governance to access patient records (where this is required) or by those brought in for their specialist skills (risk-stratified eg vulnerable patients, children in care, end of life patients, etc).
- Communicate to patients the details of alternative GP practices which could provide essential and minor surgery, including any details on the current quality of the service (ie links to nhs.uk website etc.).
- Maintain ongoing consultative relations with patients, their families, other local GP practices, the primary care network and any other system partners to ensure they are kept informed at each step of the process.
- Commission new services and arrange people to move and resettlement, including a review of the placement after a reasonable timeframe.
- Identify a lead to coordinate communications.
- Engage with local medical committee (LMC).
2.3.2 In the event the practice physically closes, the commissioner/lead commissioner will:
- Put in place arrangements for practice post to be redirected to the commissioner and where appropriate make a personal visit to the premises.
- Forward clinical correspondence to PCSE for 28 days, who will manage onward forwarding to any new provider(s). GP clinical records are delivered by City Sprint on behalf of PCSE so as part of the closedown process, the closed practice is removed from the delivery locations. PCSE address for returning correspondence can be found on the PCSE website.
- After 28 days, mails are redirected to the commissioner, but it is not forwarded to the new provider(s). The commissioner will return clinical correspondence to the sender (hospitals etc) and should inform the sender of the new provider(s). The sender should update their records accordingly to prevent reoccurrence.
- Ensure call forwarding arrangements are in place or appropriate answerphone messages are established for the closing practice to alert patients and inform 111, OOH services.
- As part of the practice closedown, the commissioner will ensure that legacy IT hardware is removed from the practice, Health and Social Care Network (HSCN) connections are terminated and clinical system call-off agreements ended as part of the GPIT system de-commissioning activities.
- Provide guidance to review, remove or copy files/folders that may be required by the outgoing owners.
GP practice (during any period where the practice is still open)
2.3.3 The commissioner will ask the GP practice to:
- Assist with ensuring appropriate interim measures are put in place to keep people safe after the identification of concerns.
- Assist the commissioner with the assessment of, and communication, with residents and their families to ascertain their needs and preferences.
- Assist the commissioner in any patient engagement, in particular those people accessing services provided at or by the GP practice and their families.
- As part of the practice closedown, work with the commissioner to ensure legacy IT hardware is removed from the practice as part of the GPIT System de-commissioning activities.
- Review and act on any guidance provided by the commissioner in relation to the closure.
- Record, collate and remove prescription pads. This includes both handwritten and computer scripts.
- Ensure all drugs/medicines in the practice are noted and handed in to the local pharmacy and signed for.
Primary Care Support England (PCSE)
2.3.4 As part of any practice close down, PCSE makes a site visit to remove, store and forward patient records to a new provider(s). Patient records should contain reprints of electronic records for patients who have not re-registered at the point of practice closure and will need to be individually placed in transit polytopes. Records will only be collected from the closing practice main site. The GP practice should send PCSE a list of records that are being collected. Records are held in archive until the patient re-registers, or the retention period expires, and they are securely destroyed. Further information can be found on the relevant PCSE information and documentation.
Care Quality Commission (CQC)
2.3.5 CQC will lead in the following actions:
- Share with the commissioner any information held about the quality of the current service.
- Share with the commissioner any information held about the quality of alternative services being considered, including the model of care used.
- Share with the commissioner any information on other providers likely to be involved in the provision of care to people at the new service.
- Consider bringing forward inspection or other evaluative activities for alternative providers where only limited quality information is available (lead role).
[Note ‘share with the commissioner’ does not have to be in writing and could be verbal or as part of any scheduled or regular meetings].
Local medical committee LMCs
2.3.6 The LMC for the area will be engaged in the following processes:
- Made aware of the engagement occurring with patients.
- Made aware of any interim proposals and immediate next steps.
- Made aware of any long term plans.
This LMC section recognises that LMCs will champion the welfare of its members and wider practice staff.
2.4 The process
2.4.1 The process for a planned practice closedown commences between 9 and 15 months prior to the scheduled end date of the contract. For unplanned closure(s), it will be necessary to undertake a rapid assessment and determine the most appropriate course of action.
2.4.2 In the large majority of cases where closure is rapid (ie immediate removal of CQC registration), the most appropriate course of action will likely involve an initial ‘caretaker’ arrangement (another GP or GP Practice team) temporarily overseeing the practice at the closing practice’s existing premises and the care of its registered list. Please refer to the section on urgent contracts in part B, chapter 1: urgent contracts.
2.4.3 In the very unusual circumstance that this is not possible, it may be necessary to rapidly disperse the list. Whilst the NHS Constitution is clear that patients have a right to choose their GP practice, to mitigate against the risk of patients being without care, the commissioner may temporarily assign a patient to an alternative provider. However, the patient must be advised of the rights under the NHS Constitution, to change at any time.
2.4.4 Patient assignment is also possible during any list dispersal (ie at the end of a ‘caretaker period’) for the same reason. This should be as a last resort, such that the commissioner has been unable to contact the patient.
2.5 Key steps (in the case of a list dispersal)
- patients are contacted in the first instance advising them of the list dispersal and available options (i.e. neighbouring practices accepting patients)
- in the event of no response or no registration at another practice, patients are re-contacted advising them again of the list dispersal and available options (ie. neighbouring practices accepting patients). Patients should also be advised at this point that, in order to prevent risk to on-going patient care, particularly in vulnerable patient groups, patients that do not re-register or contact the commissioner to advise them that they do not wish to be registered with a GP, will be allocated to another practice
- in the event of no response or no registration at another practice following the second reminder, patients must be allocated to a GP practice (except where they have not been seen or received treatment for 5 years or more – as confirmed by the GP practice). Commissioners should adopt the same approach as that set out in paragraphs 39 and 40 of schedule 3, part 4: ‘assignment of patients to lists’ of the GMS contract regulations (2015) or paragraphs 38 and 39 of schedule 2, part 4 of the PMS agreements regulations (2015)
- the patient must then be notified in writing of the allocation, the reason for the allocation and of their rights under the NHS Constitution to de-register, or re-register at an alternative GP practice should they wish
- it is imperative that at the end of the process, all patient records, and any associated data pertaining to patients (including digital records) and any clinical correspondence are transferred to the provider with whom the patient has registered. This process will generally be routine and in any case, is triggered for digital records when the patient registers at an alternative practice
- for the avoidance of doubt, at the point of closure, all patients that have not self- registered at an alternative GP practice should be allocated to another GP practice (except where they have not been seen or received treatment for 5 years or more). It is recognised that this may temporarily result in the allocation of ghost patients or patients that have gone away, however, this will be corrected through the rolling list maintenance programme
- the GP clinical system should be monitored by the commissioner or nominated IT delivery partner for a diminishing patient list. The GP clinical system should not be decommissioned until all patients dispersed/re-registered either with their practice of choice, allocation or in the case of orphaned records (where neither allocation nor re-registration occurs) the records transfer to NHS England as the data controller
- allocations should however have regard to paragraphs 23 to 31 of schedule 3, part 2 of the 2015 GMS regulations, and paragraphs 22 to 30 of schedule 2, part 2 of the 2015 PMS regulations, in relation to the removal of patients (see below)
- removal from the list at the request of the patient
- removal from the list at the request of the contractor
- removal from the list of patients who are violent
- removal from the list of patients registered elsewhere
- removal from the list of patients who have moved
- removal from list of patients whose address is unknown
- removal from the list of patients absent from the United Kingdom etc.
- removal from the list of patients accepted elsewhere as temporary residents
- removal from a list of pupils etc. of a school
- termination of responsibility for patients not registered with the contractor
2.5.1 They should also have regard to paragraph 40 (GMS) and 39 (PMS) ‘factors relevant to assignments’; namely:
When assigning a person as a new patient to a contractor’s list of patients, the commissioner must have regard to –
(a) the preferences and circumstances of the person;
(b) the distance between the person’s place of residence and the contractor’s practice premises;
(c) any request made by a contractor to remove the person from its list of patients within the preceding period of six months beginning with the date on which the application for assignment is received by the commissioner.
(d) whether, during the preceding period of six months beginning with the date on which the application for assignment is received by the commissioner, the person has been removed from a list of patients on the grounds referred to in—
(i) paragraph 23 (relating to circumstances in which a patient may be removed from a contractor’s list of patients at the request of the contractor),
(ii) paragraph 24 (relating to circumstances in which a patient who is violent may be removed from a contractor’s list of patients), or
(iii) the equivalent provisions to those paragraphs in relation to arrangements made under section 83(2) of the NHS Act 2006 (which relates to the provision of primary medical services) or under a contract made in accordance with the general medical services contracts regulations;
(e) in a case to which sub-paragraph (d)(ii) applies (or to which the equivalent provisions as mentioned in sub-paragraph (d)(iii) apply), whether the contractor has appropriate facilities to deal with such patients; and
(f) such other matters as the commissioner considers relevant.
2.5.2 It is imperative that at the end of the process, all patient records, and any associated data pertaining to patients (including digital records) and any clinical correspondence are transferred to the provider with whom the patient has registered. This process will generally be routine and in any case, is triggered for digital records when the patient registers at an alternative practice.
2.5.3 For the avoidance of doubt, at the point of closure, all patients that have not self- registered at an alternative GP practice should be allocated to another GP practice (except where they have not been seen or received treatment for 5 years or more). It is recognised that this may temporarily result in the allocation of ghost patients or patients that have gone away, however, this will be corrected through the rolling list maintenance programme.
2.5.4 The GP clinical system should be monitored by the commissioner or nominated IT delivery partner for a diminishing patient list. The GP clinical system should not be decommissioned until all patients dispersed/re-registered either with their practice of choice, allocation or in the case of orphaned records (where neither allocation nor re-registration occurs) the records transfer to NHS England as the data controller.
2.6 Engagement and re-procurement
2.6.1 Where arrangements have been made for a caretaker to temporarily manage the GP practice (refer to the urgent contract section within the contract described chapter), or a practice has terminated a contract with little notice, (eg 6 months) the commissioner should refer to the 3 stages and templates listed in this policy and guidance manual under the chapter on planned closedown.
2.6.2 It is recognised that is may not be possible to undertake each of these stages as vigorously or at the same length as if there was a 12-15 months period available as is often the case with a planned closure.
2.6.3 NHS England has a number of statutory duties relating to the exercise of its functions including reducing health inequalities and public involvement. The commissioner must ensure that its actions in re-procuring a contract or dispersing a list and any consequential actions ensure compliance with these duties. Please refer to the chapter on general duties for further guidance.
2.6.4 However, in an urgent situation, it may be necessary to balance the duty to involve with public interest in maintaining continuity of care and protecting the health, safety and welfare of patients or staff. If a commissioner considers acting in a way that may not comply with its statutory duties, it should seek further advice.
2.7 Links to relevant PCSE information and documentation
3 Death of a Contractor
3.1 Introduction
3.1.1 The aim of this policy is to provide consistency when dealing with the death of a contractor, whether they are a single-handed contractor or in a partnership and includes consideration of GMS, PMS, APMS contracts.
3.1.2 This policy outlines the procedure to follow when the death of a contractor occurs. This is a rare occurrence, but there are certain steps to follow within fixed timescales that are laid down in legislation.
3.2 Individual – GMS contract
3.2.1 Where a GMS contract is with an individual medical practitioner and that practitioner dies, the contract must terminate at the end of the period of 7 days after the date of the contractor’s death unless, before the end of that period:
- the commissioner and the contractor’s personal representatives agree in writing that the contract will continue for a further period of up to 28 days after the initial 7-day period (ie the longest possible extension is 35 days from the date of death); and
- the contractor’s personal representatives have confirmed in writing to the commissioner that they wish to employ or engage one or more general medical practitioners to assist in continuing to provide clinical services under the contract during that period; and
- the commissioner agrees to provide reasonable support which would enable the provision of clinical services under the contract to continue during that period; and
- the commissioner and the personal representatives agree the terms upon which clinical services under the contract can continue to be provided during that period
3.2.2 The commissioner should issue a confirmation letter setting out the timescales of the continuation. A template letter is provided in annex 1.
3.2.3 Note that it is not possible to extend the existing GMS contract for any longer period. Termination is mandatory and automatically takes place. Commissioners should refer to section 2: unplanned/unscheduled and unavoidable practice closedown) in relation to planning for caretaking, re-procurement or list dispersal on termination.
3.3 Individual – PMS or APMS contract
3.3.1 Where the PMS or APMS contract is with a single individual and that individual dies, the contract shall terminate at the end of the period of 7 days after the date of the contractor’s death unless, before the end of that period, the commissioner has agreed in writing with the contractor’s personal representatives that the contract should continue for a further period, not exceeding 28 days after the end of the period of seven days (ie the longest possible extension is 35 days from the date of death).
3.3.2 The commissioner should issue a confirmation letter setting out the timescales of the continuation. The template letter in annex 1 can be used.
3.3.3 Note that it is not possible to extend the existing PMS or APMS contract for any longer period. Termination is mandatory and automatically takes place. Commissioners should refer to section 2 (unplanned/unscheduled and unavoidable practice closedown) in relation to planning for caretaking, re-procurement, or list dispersal on termination.
3.4 Partnership – GMS contract
3.4.1 The GMS regulations state that where the contract is with 2 or more individuals practising in partnership, the contract shall be treated as made with the partnership as it is from time to time constituted.
3.4.2 The default position in partnership law is that every partnership is dissolved as regards all the partners by the death of any partner. The partners can, however, change this position and agree between themselves that the partnership will not dissolve on the death of any partner. It is likely that most partnerships will have dealt with this issue in their partnership deed to avoid termination of their contract.
3.4.3 The GMS regulations require GMS contracts to contain specific provisions relating to the dissolution of partnerships.
3.4.4 Where a partner dies, the GMS regulations distinguish between GMS contracts that are entered into with a contractor that consists of only 2 individuals practising in partnership and those GMS contracts where the contractor consists of more than 2 individuals.
2 individuals practising in partnership – GMS contract
3.4.5 Where the contractor consists of two individuals practising in partnership and the partnership is dissolved or terminated due to the death of one of the partners, the surviving partner must notify the commissioner in writing as soon as is reasonably practicable of the death of their partner.
3.4.6 Where the commissioner receives such a notice, it must acknowledge receipt of the notice in writing.
3.4.7 If the surviving partner is a general medical practitioner, the contract will continue with that individual. The commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date upon which that variation is to take effect.
3.4.8 A template notification letter is provided in annex 2. A variation notice will need to be included with this letter.
3.4.9 To provide assurance that the individual is able to meet the contractual obligations, the commissioner should discuss with the individual continued service delivery options bearing in mind the size of the practice, the range of services provided and any potential capacity issues.
3.4.10 If the surviving partner is not a general medical practitioner, the commissioner must enter into discussions with the surviving partner and use reasonable endeavours to reach an agreement to enable the provision of clinical services to continue under the contract. The commissioner may, if it considers it appropriate to enable clinical services under the contract to continue, offer the surviving partner reasonable support.
3.4.11 The commissioner may choose to consult the relevant LMC, if it considers it appropriate or any other person that the commissioner considers necessary.
3.4.12 Where the commissioner reaches an agreement with a surviving partner who is not a general medical practitioner, the commissioner must notify that individual confirming:
- the terms upon which the commissioner agrees to the contract continuing with that individual
- the interim period during which the contract is to continue which must not exceed 6 months
- that the individual will employ or engage a general medical practitioner for the interim period to assist in the provision of clinical services under the contract
- the support, if any, which the commissioner is to provide to enable clinical services under the contract to continue during the interim period
3.4.13 A template notification letter is provided in annex 3. A variation notice will need to be included with this letter.
3.4.14 Where the commissioner cannot reach an agreement with the surviving partner or if the surviving partner does not wish to employ or engage a medical practitioner, the commissioner must terminate the contract immediately by serving notice in writing on the surviving partner.
3.4.15 The commissioner must also terminate the contract in writing to the surviving partner if:
- the surviving partner wishes to withdraw from the agreed arrangements at any stage during the interim period; or
- at the end of the interim period, the contractor has not entered into partnership with a general medical practitioner who is not a limited partner
3.4.16 Where the commissioner intends to terminate the contract, please refer to the chapter on contract breaches, sanctions and termination for further information on considerations relating to terminating a contract.
3.4.17 A template termination letter is set out in annex 4.
More than 2 individuals practising in partnership – GMS contract
3.4.18 Where there are more than 2 individuals practising in partnership, the death of 1 of the partners may result in the partnership being dissolved. This may not always be the case as the partnership arrangements between the partners may state that the partnership will continue or make other provision on the death of a partner that does not result in the dissolution of the partnership.
3.4.19 Where the partnership is not dissolved or terminated, the contract will continue and the provisions below will not apply provided that the partnership remains eligible to hold the GMS contract. Please refer to the contracts described chapter for further information on eligibility requirements.
3.4.20 It is possible for the contract to continue where the partnership is dissolved or terminated for whatever reason (which may be due to the death of a partner) and the contractor consists of more than 2 individuals practising in partnership. The contract may continue with one of the former partners if the following conditions apply:
- the former partner must be nominated by the contractor
- the former partner must be a medical practitioner that meets the condition in regulation 4(2)(a) of the GMS regulations
3.4.21 The nomination of the former partner by the contractor must be:
- in writing and signed by all of the persons who are practising in partnership
- specify the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- be provided to the commissioner at least 28 days in advance of the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- specify the name of the medical practitioner with whom the contract will continue, which must be one of the partners
3.4.22 Where the commissioner receives such a nomination, it must acknowledge receipt of the notice in writing before the date specified in the nomination as the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner.
3.4.23 The commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date upon which that variation is to take effect.
3.4.24 A template notification letter is provided in annex 5. A variation notice will need to be included with this letter.
3.5 Two or more signatories – PMS agreement
3.5.1 The PMS regulations do not allow PMS agreements to be treated as made with a partnership. Where individuals are practising in partnership, the PMS agreement will be entered into with each individual (who may or may not be in partnership). The individual signatories to a PMS agreement collectively form the contractor. The PMS regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The Commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
3.5.2 Ideally, a surviving signatory to a PMS agreement will notify the commissioner in writing as soon as reasonably practicable of the death of their co-signatory.
3.5.3 Upon receipt of the notification from the surviving co-signatory(ies), the commissioner will need to consider the implications that the death of the co-signatory will have on the ongoing provision of services under the agreement.
3.5.4 Where the commissioner is satisfied that the remaining signatory(ies) is eligible to hold the agreement and agrees that the agreement is to continue, the agreement will need to be varied to remove the deceased as a signatory.
3.5.5 The process above does not affect any right that the commissioner may have to terminate the agreement under any terms of the agreement.
3.6 2 or more signatories – APMS contract
3.6.1 The commissioner must review the relevant APMS contract to determine whether any provisions relate to the death of a contractor prior to following any process for variation.
3.6.2 Where no provisions cover this scenario, paragraphs 3.5.2 to 3.5.5 are likely to be relevant.
3.7 Practical issues arising from death of a contractor
Request to form a partnership
3.7.1 Where a GMS contract is held by an individual as a result of the death of a partner, that individual (like any individual GMS contractor) may propose to practice in partnership with 1 or more persons during the existence of the contract. Please refer to the chapter on contracts variations for more information on the relevant process and obligations of the commissioner.
Procuring a new contract
3.7.2 Where death of a contractor results in termination of the contract in any of the ways described above, the commissioner will need to decide whether to procure primary care medical services to replace the contract.
3.8 Links to relevant PCSE information and documentation
4 Managing disputes
4.1 Introduction
4.1.1 This policy describes the process to determine the action required when a contractor has requested to follow the NHS dispute resolution process or where the commissioner elects to follow the NHS dispute resolution procedure.
4.1.2 The policy focuses on primary medical services contracts in their various forms.
4.2 Background
4.2.1 The commissioner must identify whether the contract is an NHS contract or a non-NHS contract. In GMS contracts, the commissioner can do this by reviewing clause 3.1 of the standard GMS contract. A similar clause will also be set out within PMS and APMS contracts.
4.2.2 An NHS contract (as set out at section 9 of the NHS Act) is an arrangement under which one health service body arranges for the provision of goods or services to another health service body. It must not be regarded as giving rise to contractual rights or liabilities.
4.2.3 A non-NHS contract is where the contract is legally binding.
4.2.4 Contractors have the right to be regarded as a health service body under regulation 10 of the GMS regulations or regulation 9 of the PMS regulations or where the APMS contractor is a health service body by virtue of section 9 of the NHS Act.
4.2.5 Where a contractor is regarded as being a health service body, its contract will be an NHS contract. Where a contractor is not regarded as a health service body, its contract will not be an NHS contract. Health service body status affects the eligibility and application process for NHS dispute resolution.
4.2.6 GMS and PMS contracts require the parties to make every reasonable effort to communicate and co-operate with each other to resolve the dispute before referring the dispute for determination in accordance with the NHS dispute resolution procedure or, where applicable, before commencing court proceedings.
4.2.7 There are 2 different routes that can be taken for resolving contractual disputes, depending on the contractor’s health service body status:
4.2.7.1 where the contractor is a health service body, and the contract is an NHS contract the steps laid out in this policy will be used to resolve all matters of dispute. The parties should not make a claim at court in relation to the contracts; or
4.2.7.2 where the contractor is not a health service body and the contract is a non-NHS contract, the dispute can either be resolved using the process described within this policy or using the court system.
4.2.8 The dispute resolution process for APMS contracts is specific to the parties’ agreement as set out in the APMS contract. The APMS contract must be reviewed in the event of a dispute and that process followed. The APMS directions do not require the NHS dispute resolution to be included in the APMS contract and more commercial terms are usually set out.
4.2.9 The use of the court system can be an expensive and public route. In normal circumstances, non-health service bodies will elect to follow the NHS dispute resolution.
4.2.10 Where the parties have followed this policy and the NHS dispute resolution to the end determination, the result is binding. A second referral to the court system for a further ruling on the same issue cannot be made other than to enforce the decision as having the status of a county court judgement or to seek judicial review of the process.
4.3 Managing disputes – informal process
4.3.1 The parties must make every reasonable effort to communicate their issues in relation to decision-making and rationale and must co-operate with each other to resolve any disputes that emerge informally before considering referring the matter for determination through formal dispute resolution procedures.
4.3.2 The formal process should not be initiated until the informal process has been exhausted and it should be noted that both parties may wish to involve the relevant professional representative (eg LMC).
4.3.3 The use of an informal resolution process helps develop and sustain a partnership approach between contractor and commissioner.
4.3.4 The informal process may include (but is limited to):
- regular telephone communications
- face-to-face meetings at a mutually convenient location; and/or
- written communications
4.3.5 It is essential that the commissioner maintains accurate and complete written records of all discussions and correspondence on the contract file in relation to the dispute at all levels of dispute resolution. The commissioner should ensure that it responds to contractor concerns and communications in a timely and reasonable manner.
4.4 Managing disputes – stage 1 (local dispute resolution)
4.4.1 The timescales set out in this stage 1 are indicative only. The commissioner should ensure any timescales used are appropriate to the circumstances. Regardless of timescales, the parties must ensure that every reasonable effort to communicate and co-operate with each other is made prior to invoking stage 2 of the NHS dispute resolution procedure.
4.4.2 Where a dispute arises, the commissioner should refer to the relevant policy that covers the issue that caused the dispute to determine whether due process has been followed.
4.4.3 The contractor should notify the commissioner of its intention to dispute one or more decisions made in relation to its contract. This notification should usually be received no later than 28 days after the commissioner advises the contractor of its decision except in exceptional circumstances.
4.4.4 The commissioner will immediately cease all actions in relation to the disputed notice or decision, until:
- there has been a determination of the dispute and that determination permits the commissioner to impose the planned action; or
- the contractor ceases to pursue the NHS dispute resolution procedure or court proceedings,
- whichever is the sooner
4.4.5 Where the commissioner is satisfied that it is necessary to terminate the contract or impose a contract sanction before the NHS dispute resolution procedure is concluded in order to:
- protect the safety of the contractor’s patients; or
- protect NHS England from material financial loss
- then the commissioner shall be entitled to terminate the contract or impose the contract sanction at the end of the period of notice it served. This should only be followed with close reference to the GMS regulations and PMS regulations, pending the outcome of that procedure.
4.4.6 The paragraphs below set out a process that may be adopted for stage 1 (local dispute resolution).
4.4.7 The commissioner may acknowledge the notification of dispute within seven days of receipt and request the submission of supporting evidence from the contractor within a further 28 days from the date they receive the letter. An example acknowledgement letter is provided in annex 1.
4.4.8 Upon receipt of the evidence the commissioner should review the evidence within 28 days and invite the contractor to attend a meeting, which should be as soon as possible, but at the very latest within a further 28 days. The contractor(s) has the opportunity to invite representative bodies to support it at the meeting, for example, the LMC. An example invite letter is provided in annex 2.
4.4.9 Once the meeting has been held, the commissioner should notify the contractor in writing of the outcome of the meeting, whether the dispute will now need to be moved to stage 2 of the NHS dispute resolution procedure (refer to the example stage 1 outcome letter in annex 3) or that the dispute has been successfully resolved (refer to the example stage 1 outcome letter in annex 4):
4.4.10 Where the matter is resolved, the issue can be deemed closed, and the commissioner should document the outcome accordingly on the contract file.
4.4.11 Where the matter remains unresolved, the process may be escalated to the next stage of the dispute resolution procedure.
4.4.12 At this point the commissioner should commence preparation of the contract file to ensure that if and when NHSR or court requests submission of evidence in respect of the dispute the documentation is in order.
4.5 Managing disputes – stage 2 (NHS dispute resolution procedure)
4.5.1 The informal process and stage 1 (local dispute resolution) should be exhausted before proceeding to this stage of the process. The commissioner or a contractor wishing to follow this route must submit a written request for dispute resolution to:
Postal address: NHS Resolution, Primary Care Appeals
8th Floor, 10 South Colonnade, Canary Wharf, London, E14 4PU
Email: nhsr.appeals@nhs.net
Primary Care Appeals (PCA) at NHSR carries out the NHS dispute resolution functions of the Secretary of State in the GMS regulations and the PMS regulations and any written request for dispute resolution should include:
- the names and addresses of the parties to the dispute
- a copy of the contract
- a brief statement describing the nature and circumstances of the dispute
4.5.2 The written request for dispute resolution must be sent within 3 years from the date on which the matter gives rise to the dispute occurred or should have reasonably come to the attention of the party wishing to refer the dispute. Please see NHSR PCA determination reference 17156 for further details on the date that the dispute should have reasonably come to the attention of the relevant party.
4.5.3 The commissioner will be required to prepare documentation evidence and potentially an oral presentation in response to evidence presented in support of the dispute. Each party will be asked to prepare representations on the dispute, which will be circulated to the other party and an opportunity to provide observations on the other party’s representations will be given. Again, the observations of each party will be circulated to the other party.
4.5.4 The commissioner should not underestimate the preparation that will be required in the event that evidence is required by NHSR PCA, as all records pertaining to the contractor in question may be required, including (but not limited to) all contract documentation and contract variations, all written correspondence (both to and from the commissioner and the contractor) and any electronic correspondence that may have passed between the parties, in relation to the dispute. This process will benefit from a clearly recorded contract file.
4.5.5 The commissioner must ensure that records of communications and contract files are maintained to a high standard and all documentary evidence is collated correctly prior to submission to NHSR PCA.
4.5.6 Once NHSR PCA has reached a conclusion (the determination) the commissioner will receive a copy and will be required to act upon it. Parties involved in dispute resolution should follow the NHSR PCA guidance note.
Delegated commissioning arrangements
The Delegation Agreement includes a section on claims and litigation which is likely to include a dispute with a GMS, PMS or APMS contractor that has been referred to stage 2 of the NHS dispute resolution procedure. In such cases, the commissioner is required to act in accordance with the delegation agreement which includes but is not limited to:
- notifying NHS England of any documents concerning the dispute and providing copies of these documents
- co-operating fully with NHS England in relation to such dispute and the conduct of such dispute
- providing, at its own cost, to NHS England all documentation and other correspondence that NHS England requires for the purposes of considering and/or resisting such dispute; and/or
at the request of NHS England, taking such action or step or providing such assistance as may in NHS England’s discretion be necessary or desirable having regard to the nature of the dispute and the existence of any time limit in relation to avoiding, disputing, defending, resisting, appealing, seeking a review or compromising such dispute or to comply with the requirements of NHSR PCA in relation to such dispute.
4.6 Other dispute resolution procedures
4.6.1 The GMS and PMS regulations allow the NHS dispute resolution procedure to be used by the contractor as a means of resolving every dispute except where an assessment panel determines that the commissioner may assign new patients to contractors that have closed their practice list of patients.
4.6.2 Disputes may also arise prior to a contract being entered into. Such disputes will relate to the eligibility of the person seeking to enter the contract or contract terms.
4.6.3 Where the commissioner is of the view that a person seeking to enter a contract does not meet the eligibility conditions (please refer to the contracts described chapter for further information), the commissioner must notify the person in writing.
4.6.4 This notice must state the commissioner’s view of the person’s eligibility, reasons for that view and guidance on the person’s right of appeal.
4.6.5 Where the commissioner has issued such a notice, the recipient of the notice has a right of appeal to the First-Tier Tribunal.
4.6.6 Where the dispute relates to the parties being unable to agree on a particular proposed term of a GMS or PMS contract, either party may refer the dispute to the Secretary of State to consider and determine the matter in accordance with:
- for GMS contracts, part 12 and regulation 9 of the GMS regulations; or
- or PMS agreements, Part 13 and regulation 8 of the PMS regulations’
- except where both parties to the prospective agreement health service bodies are, (in which case section 9 of the NHS Act applies)
4.7 Assignment of patients to lists: procedure relating to determinations of the assessment panel
4.7.1 Where an assessment panel determines that the commissioner may assign new patients to contractors which have closed their practice list of patients, any contractor specified in that determination may refer the matter to the Secretary of State to review the determination of the assessment panel.
4.7.2 If a referral is made to the Secretary of State, it shall be reviewed in accordance with the following procedure:
- where more than one contractor specified in the determination of the assessment panel wishes to refer the matter for dispute resolution, those contractors may, if they all agree, refer the matter jointly, and in that case the Secretary of State shall review the matter in relation to those contractors together
- within the period of 7 days beginning with the date of the determination by the assessment panel, the contractor(s) shall send to the Secretary of State a written request for a dispute resolution which shall include or be accompanied by:
- the names and addresses of the parties to the dispute
- a copy of the contract (or contracts)
- a brief statement describing the nature and circumstances of the dispute
4.7.3 Each party will be asked to make representations and observations on the representations of the other party both of which will be allocated between the parties.
4.7.4 Within the period of 21 days beginning with the date on which the matter was referred to him, the Secretary of State shall determine whether the commissioner may assign patients to contractors that have closed their lists of patients. If the Secretary of State determines that the commissioner may make such assignments, the Secretary of State shall also determine those contractors to which patients may be assigned.
4.7.5 The Secretary of State may not determine that patients may be assigned to a contractor which was not specified in the determination of the assessment panel.
4.7.6 In the case of a matter referred jointly by contractors, the Secretary of State may determine that patients may be assigned to one, some or all of the contractors that referred the matter.
4.7.7 The period of 21 days for determination may be extended (even after it has expired) by a further specified number of days if an agreement to that effect is reached by:
- the Secretary of State
- the Commissioner
- the contractor(s) that referred the matter to dispute resolution
4.7.8 The Secretary of State shall record the determination and the reasons for it in writing and shall give notice of the determination (including the record of the reasons) to the parties.
5 Adverse events (eg flood fire)
5.1 Background
5.1.1 Adverse incidents are dealt with in the force majeure provisions of the standard GMS, PMS and APMS contracts. Although these provisions are not required by the GMS regulations, the PMS regulations or the APMS directions, the majority of contracts will include them.
5.1.2 The commissioner is advised to check that the force majeure provisions are included in each contract and if they are to follow the guidance in this policy. This policy is only applicable where the contract in question has retained the recommended force majeure provisions.
5.1.3 The contractor is responsible for informing the commissioner of any force majeure event.
5.2 Contract wording
5.2.1 Clause 27.5 of the standard GMS contract states that:
“27.5.1 Neither party shall be responsible to the other for any failure or delay in performance of its obligations and duties under this contract which is caused by circumstances or events beyond the reasonable control of a party. However, the affected party must promptly on the occurrence of such circumstances or events:
(a) inform the other party in writing of such circumstances or events and of what obligation or duty they have delayed or prevented being performed; and
(b) take all action within its power to comply with the terms of this Contract as fully and promptly as possible.
27.5.2 Unless the affected party takes such steps, clause 27.5.1 shall not have the effect of absolving it from its obligations under this contract. For the avoidance of doubt, any actions or omissions of either party’s personnel or any failures of either party’s systems, procedures, premises, or equipment shall not be deemed to be circumstances or events beyond the reasonable control of the relevant party for the purposes of this clause, unless the cause of failure was beyond reasonable control.
27.5.3. If the affected party is delayed or prevented from performing its obligations and duties under the contract for a continuous period of 3 months, then either party may terminate this contract by notice in writing within such period as is reasonable in the circumstances (which shall be no shorter than 28 days).
27.5.4. The termination shall not take effect at the end of the notice period if the affected party is able to resume performance of its obligations and duties under the contract within the period of notice specified in accordance with clause 27.5.3 above, or if the other party otherwise consents”.
5.2.2 The provision of individual PMS and APMS contracts should be reviewed, and advice sought.
5.2.3 A force majeure event is one which is caused by circumstances beyond the reasonable control of either the commissioner or the contractor that could not have been avoided or mitigated with reasonable care and where the event has had a material effect on the fulfilment of the contract.
5.2.4 Examples of events that may invoke the force majeure provisions are as follows:
- fire
- flood
- severe weather conditions and for which precautions are not ordinarily taken to avoid or mitigate the impact (for example a severe hurricane)
- industrial action which significantly affects the provision of public services or services upon which the party is reliant
- death of a significant performer or close relative
- pandemic disease or circumstances that might otherwise be considered “an act of God”
- war
- civil war (whether declared or undeclared)
- riot or armed conflict
- radioactive, chemical, or biological contamination
- pressure waves caused by aircraft or other aerial devices travelling at sonic or supersonic speed
- acts of terrorism
- explosion
5.2.5 Examples of events that would not be considered force majeure events are as follows:
- refurbishment of practice premises
- adverse weather in the winter months (including snow and ice)
- planned events (including elective surgery, leave, weddings and similar events)
- long-term sickness, maternity/paternity, or adoption leave
5.3 Contract compliance
5.3.1 All contractors will likely be obliged under the terms of their contracts to promptly notify the commissioner of a force majeure event, detailing the cause or event, what service provision is being delayed or prevented and what business continuity action(s) within their power they are taking in order to comply with the terms of the contract as fully and promptly as possible.
5.3.2 Failure to notify the commissioner will mean that the contractor is not absolved from its obligations under the contract.
5.3.3 Neither party will be responsible to the other for any failure to delay in performing its obligations and duties under the contract which is caused by an event of force majeure
5.3.4 A template notification is provided in annex 1 which the commissioner can send to the contractor for completion.
5.3.5 The commissioner will record that the event has happened and provide the contractor with an acknowledgment letter, a template is provided in annex 2.
5.4 Clinical governance and risk management/termination
5.4.1 If the consequence of the contractor’s failure to deliver services is significant and poses a risk to patient safety or the efficiency of wider primary care services, the commissioner may wish to consider recording the incident on the risk register or consider whether it may invoke its termination rights.
5.4.2 If the service provision is delayed or prevented for a continuous period of 3 months, then either party will likely be able to terminate the agreement by notice in writing within a period which is reasonable (and no less than 28 days). This termination will not take effect where the service is resumed within the period of notice or if the contractor consents to this.
5.5 Appeals
The parties should refer to the chapter on managing disputes for the process in relation to a dispute.
5.6 Payment and contract system
- The parties should discuss the effect of force majeure on payments by the commissioner to the contractor. The commissioner should use its reasonable discretion in determining payments with regard to the need for the contractor to continue to provide services once it is no longer affected by the force majeure event provided the contract has not been terminated.
Part D – general
1 GP IT operating model: data and cyber security arrangements
1.1 Introduction
1.1.1 This chapter provides an overview of GP IT operating arrangements, as outlined in the GP IT operating model, securing excellence in primary care (GP) digital services: the primary care GP digital services operating model 2019-21, published by NHS England. Particular reference is made to data and cyber security arrangements, following the publication of the National data guardian review in July 2016 which included key recommendations and proposed 10 data security standards.
1.2 Background
1.2.1 NHS England is accountable for the delivery of GP IT services, with responsibility for the commissioning of GP IT services delegated to ICBs under the NHS Act 2006 (as amended).
1.2.2 The GP IT operating model outlines accountabilities and commissioning responsibilities for the provision of high quality GP IT support services.
1.2.3 ICBs are encouraged to work in partnership with primary care stakeholders to develop a local digital strategy and delivery plans, set priorities and local direction for digital support services and technology, that can be used to optimal effect for the benefit of patient care.
1.2.4 The GP IT operating model, provides a detailed schedule of ‘core and mandated’ capabilities and enabling requirements, which includes standards to ensure that procured services are compliant with data protection and cyber security regulations and controls. In addition, ‘enhanced’ requirements to facilitate local service improvement and transformation should be developed and agreed locally to support local strategic priorities and commissioning strategies to improve service delivery. ICBs are responsible for ensuring all these requirements are provided to the standards described in the GP IT operating model.
1.2.5 An ICB may choose to commission services from one or more GP IT delivery partners. The GP IT commissioning specification support pack is available to support ICBs in the effective procurement and ongoing review of GP IT services. This includes a GP IT data capture service schedule which can be used by ICBs to review current service provision arrangements or to support re-procurement activities, including the development of local service specifications.
1.2.6 The details of the provision of these services must be recorded in the ICB practice agreement, signed by both the ICB and each constituent general practice, as a core contractual requirement. This nationally developed agreement sets out the terms governing the provision and receipt of digital services in general practice and will include as an appendix, details of local service provision arrangements.
1.2.7 Each practice needs to work with the ICB and its locally commissioned GP IT delivery partner(s), as outlined in the ICB practice agreement, to enable them to effectively support the IT infrastructure, respond to service incidents and maintain compliance with security standards, in line with national standards and locally agreed service level agreements.
1.2.8 As end users of technology, GPs and their staff need to be familiar with the GP IT services being provided and delivered locally, the support arrangements particularly in cases of cyber security incidents and what local contingency and recovery processes are in place when technology fails.
1.3 GP IT operating model: cyber and data security updates
1.3.1 The GP IT operating model revised in 2020, provides a detailed schedule of services outlining ‘core and mandated’ capabilities and enabling requirements, which includes standards to ensure that procured services are compliant with data protection and cyber security regulations and controls.
ICBs have delegated responsibility to provide by either directly or through commissioning digital services for their practices as defined in the GPIT operating model. ICBs are not expected to offer GP IT funds directly to general practices to enable them to provide or commission these services, unless advised otherwise for a specified purpose in the GP IT operating model. Where a practice declines the digital service or support offered by the ICB as described in the GP IT operating model, the ICB is under no obligation to offer an alternative or to fund the practice in lieu of the service.
1.3.2 An ICB may choose to commission ‘core and mandated’ services from one or more GP IT delivery partners. The GP IT commissioning specification support pack is available to support ICBs in the effective procurement and ongoing review of GP IT services. This includes a GP IT data capture service schedule which can be used by ICBs to review current service provision arrangements or to support re-procurement activities, including the development of local service specifications.
1.3.3 Each practice needs to work with the ICB, or the locally commissioned GP IT delivery partner(s) as outlined in the ICB practice agreement, to enable them to effectively support the IT infrastructure, respond to service incidents and maintain compliance with security standards, in line with national standards and locally agreed service level agreements.
1.3.4 As end users of technology, GPs and their staff need to be familiar with the GP IT services being provided and delivered locally, the support arrangements particularly in cases of cyber security incidents and what local contingency and recovery processes are in place when technology fails.
1.4 Review of data security, consent and opt-outs (national data guardian, July 2016)
1.4.1 In July 2016, recommendations and 10 proposed standards for Data Security were published for consultation in the National data guardian (NDG) for health and care review of data security, consent and opt-outs. These are aimed at strengthening the safeguards for keeping health and care information secure and ensuring the public can make informed choices about how their data is used.
1.4.2 A parallel review was also conducted by the Care and Quality Commission on (CQC) ‘Safe data, safe care’ which focused on the availability, integrity and confidentiality of patient data.
1.4.3 Following national consultation, the plan outlined within ‘Your data: better security, better choice, better care (DH Data Sharing and Cyber Security team, July 2017) supports the recommendations within the NDG and CQC reviews respectively and centres on ensuring local organisations are implementing the 10 data security standards. These have been further strengthened in some areas, including data security standard 6, which now requires significant cyber-attacks to be reported by health and care organisations to the Data Security Centre as soon as possible following detection. These are supported by national support services and backed by clear contractual obligations and by assurance and regulatory action.
1.4.4 National services and security advice are offered by NHS England’s Data Security Centre to ensure patient data and information is used safely and securely and to enable health and care organisations prepare their own resilience to cyber security threats, and to respond effectively and safely when they occur.
1.4.5 As part of the GP contract for 2017/18 non-contractual changes to joint guidance have been agreed which include general practice compliance with the ten new data security standards in the NDG review, as outlined below:
1.5 10 data security standards
Category: people
Ensure staff are equipped to handle information respectfully and safely, according to the Caldicott Principles
Data security standard 1
All staff ensure that personal confidential data is handled, stored, and transmitted securely, whether in electronic or paper form. Personal confidential data is shared for only lawful and appropriate purposes.
Data security standard 2
All staff understand their responsibilities under the National Data Guardian’s data security standards, including their obligation to handle information responsibly and their personal accountability for deliberate or avoidable breaches.
Data security standard 3
All staff complete appropriate annual data security training and pass a mandatory test, provided through the redesigned Information governance toolkit.
Category: process
Ensure the organisation proactively prevents data security breaches and responds appropriately to incidents or near misses.
Data Security Standard 4
Personal confidential data is only accessible to staff who need it for their current role and access is removed as soon as it is no longer required. All instances of access to personal confidential data on IT systems can be attributed to individuals.
Data security standard 5
Processes are reviewed at least annually to identify and improve any which have caused breaches or near misses, or which force staff to use workarounds which compromise data security.
Data security standard 6
Cyber-attacks against services are identified and resisted and CareCERT security advice is responded to. Action is taken as soon as possible following a data breach or near miss, with a report made to senior management within 12 hours of detection. Significant cyber-attacks are to be reported to CareCERT immediately following detection.
Data security standard 7
A continuity plan is in place to respond to threats to data security, including significant data breaches or near misses, and it is tested once a year as a minimum, with a report to senior management.
Category: technology
Ensure technology is secure and up to date.
Data security standard 8
No unsupported operating systems, software or internet browsers are used within the IT estate.
Data security standard 9
A strategy is in place for protecting IT systems from cyber threats, based on a proven cyber security framework such as Cyber Essentials. This is reviewed at least annually.
Data security standard 10
IT suppliers are held accountable via contracts for protecting the personal confidential data they process and for meeting the National Data Guardian’s data security standards.
1.5.1 The Data security and protection toolkit is an online self-assessment tool that enables organisations to measure and publish their performance against the National Data Guardian’s 10 data security standards. The ICB-practice agreement requires general practices to complete the DSPT annually. Local (ICB) commissioned GP IT delivery partners (providers) must also be contractually required to complete the DSPT.
1.5.2 The DSP toolkit will provide individual organisations with the necessary tools to assess adherence to the standards and level of cyber capability, as well as providing a national picture of data security across the health and social care system, and intelligence for independent assurance processes. A new incident reporting tool for data security and protection incidents was launched within the Data security and protection toolkit. Through the Data Security Centre and the Cyber Security Programme, NHS England will enable organisations to put those standards into practice.
1.5.3 Information from the DSPT will support CQC inspections, which from September 2017 will include the importance of meeting the data security standards. In addition, a new incident reporting tool for data security and protection incidents has been launched within the Data security and protection toolkit. The DHSC has published the 2017/18 data security and protection requirements clarified action required by general practices.
1.5.4 The network and information systems regulations 2018 which came into force in May 2018 gave further legal backing to the 10 data security standards, by requiring those organisations identified as ‘operators of essential services’ to comply with defined security requirements. GP IT operating model arrangements will continue to be reviewed and will be updated to reflect these requirements.
1.6 Locally procured 3rd party digital systems, services and architecture
1.6.1 Consideration needs to be given to security arrangements for locally procured digital systems, services and architecture which are provided by suppliers outside the GP IT futures framework, the local commissioned GP IT services, and national digital services.
1.6.2 The commissioner or general practice needs to ensure that any digital services and infrastructure procured locally are provided by organisations compliant with the applicable standards in the operating model.
Practices remain responsible for choice and funding of their practice telephony system but are encouraged to consider using advanced voice over internet protocol (VoIP) cloud-based telephony systems which better support peak demand management, PCNs and federated working and operational resilience. A support pack and template specification to assist practices is provided in the GP IT operating model.
1.6.3 Clear support arrangements are essential and should describe how these align with local GP IT delivery arrangements. This is critical in effective incident management.
1.7 Disaster recovery and business continuity (DR/BC)
1.7.1 Each practice will have a business continuity plan as part of their DSP Toolkit compliance and this should include responses to data security and cyber security threats/incidents, significant breaches or near misses and response to a loss of access to patient records.
1.7.2 All practices must register with the MHRA Central Alerting System which will be utilised as required, to support any national cyber security incident.
1.7.3 The ICB will ensure advice/guidance to support the development of the digital element of the practice BC plan, is available. ICBs should approve practice BC plans. As more systems become securely hosted externally and fewer are located within individual practice premises and control the role of a practice disaster recovery (DR) plan becomes less relevant. In the event of a practice BC plan being invoked, the ICB will ensure specialist technical support is available as necessary.
1.7.4 It is important for all staff in the practice to understand their roles when the plans are activated. The practice team will need to work together to do the right thing at the right time and to ensure that the right people are in place with the right support. All practice staff must complete the annual NHS data security awareness level 1 training.
1.7.5 The recovery process after an incident is equally important to ensure that electronic patient records are kept up to date and lessons are learned on how the response to the incident was managed.
1.7.6 BC plans should be reviewed as required under the terms of the ICB practice agreement.
1.7.7 The review of BC plans will need to consider those circumstances where the practice may be unaffected, but providers are. For example, the shutdown of a secondary care provider that supplies pathology services may delay the availability of test results or the availability of discharge advice notes. Whilst these may be beyond the scope of the practice, planning and agreement with the ICB on how to handle these circumstances will be of benefit to the practice and their patients.
Practice business continuity plans should also consider practice resilience arrangements including the capability for home and remote working, alternate consultation channels (eg online, video) and exceptional demand management. BC plans must always be reviewed following their invocation.
1.7.8 Local (ICB) commissioned GP IT delivery partners (providers) must also be contractually required to prepare and maintain BC and DR plans for those services relevant to the delivery of GP IT.
1.8 Further Information
Commissioners seeking further information on the GP IT Operating Model and associated support materials and guidance, can visit the digital primary care section of the NHS England website or contact the NHS England Digital Primary Care (GP IT) team: england.digitalprimarycare@nhs.net
For further information about the DSP toolkit please visit DSP toolkit help section or contact cybersecurity@nhs.net
2 Protocol in respect of locum cover or GP performer payments for parental and sickness leave
2.1 Background
2.1.1 The General Medical Services Contracts Statement of Financial Entitlement Directions 2023 (SFE) sets out the provisions, conditions and payments relating to reimbursement to GP practices for GP performers covering parental leave and sickness leave.
2.1.2 This protocol applies only to GMS practices, but commissioners should ensure they treat primary medical services (PMS) practices equitably.
2.1.3 For the purposes of this protocol:
- “parental leave” means ordinary or additional maternity leave, paternity leave, ordinary or additional adoption leave, or shared parental leave
- “full-time” means nine sessions of clinical work per working week
- “working week” is defined as the core hours set out in the National Health Service (GMS contracts) regulations: “the period beginning at 8:00 am and ending at 6.30 pm on any day from Monday to Friday except Good Friday, Christmas Day or bank holidays”
2.1.4 The commissioner will not make payments in respect of locum or GP performer cover outside of core hours.
2.2 Parental and sickness leave payments
2.2.1 Providing the relevant provisions of the SFE are met, GP practices are entitled to claim reimbursement of the cost for providing GP performer cover when a GP performer is on parental leave or on sickness leave.
2.2.2 The reimbursement of costs can be claimed where the cover is provided by:
- a locum
- a salaried GP on a fixed term contract
- a GP already working in the practice but who is not full-time (either employed or a partner)
2.2.3 Payments will not be made on a pro-rata basis having regard to the absent performer’s working pattern and will be the lower of actual invoiced costs or maximum amount.
2.2.4 The SFE sets out the maximum amount of reimbursement for a GP performer providing cover as follows.
2.3 Parental leave
2.3.1 In respect of maternity leave or adoption leave where the GP performer going on leave is the main care provider, or shared parental leave, the maximum amount payable is £1,143.06 per week for each of the first 2 weeks and then £1,751.52 per week for each of weeks 3 to 26.
2.3.2 Commissioners should reimburse shared parental leave in the same way as maternity leave. It will be for the practice to demonstrate that a GP performer is eligible for shared parental leave either under statute (for salaried GPs) or under the terms of a partnership agreement. See information on eligibility for shared parental leave.
2.3.3 In respect of paternity leave or special leave (which is equivalent to the terms and duration of paternity leave) where the GP performer going on leave is not the main care provider, the maximum amount payable is £1,143.06 per week for each of the first 2 weeks.
2.4 Sickness leave
2.4.1 In respect of sickness leave, for each period of sickness leave, there is a qualifying period of 2 weeks during which time no payments are made.
2.4.2 After two weeks, payments start and the maximum amount payable is £1,751.52 per week for each of weeks 3 to 28. Thereafter, the maximum amount payable is £875.76 per week for each of weeks 29 to 54.
2.4.3 As set out in the SFE, for weeks 29 to 54 the commissioner will pay half of whatever it determined was payable for weeks 3 to 28. The SFE also sets out a methodology for calculating these periods with respect to any payments made in the previous 52 weeks and that methodology continues to apply.
2.5 Sickness leaves and phased return to work
2.5.1 Commissioners support the safe return to work of GP performers and recognise that GP practices exercise flexibility in managing sickness absence (where GP performers under a fit note are declared they may be fit to work, subject to advice and agreement on phased return or adjusted hours). The fit note in such cases is continuing to declare sickness absence for the period, subject to and excluding any agreed working arrangements. For example, if a GP performer is advised they may be fit to work 2 days out of 5 for two weeks – then the other 3 days in each week for that period remain as sickness absence.
2.5.2 Payment in respect of necessary cover for this sickness absence under a fit note advising phased return or adjusted hours may however be mandatory or discretionary, subject to the requirements of the SFE being met.
2.5.3 In respect of GP performer who is a partner, the SFE makes no distinction on sickness leave, meaning paragraph 10.3 of the SFE applies whether a GP partner is under a fit note declaring they are unfit to work, or may be fit to work subject to advice given on phased return or adjusted hours. Mandatory provision for payment therefore applies and commissioners should continue to reimburse locum cover covers costs as per paragraph 11 above.
2.5.4 In respect of GP performer who is an employee, the SFE applies further requirements at paragraph 10.3 to qualify for payment – which is that the contractor is required to pay the GP performer statutory sick pay (SSP) or their full salary during sickness leave under their contract of employment.
2.5.5 A phased return or adjusted hours arrangement may interfere with a contractor meeting these requirements – SSP is subject to forming a period of incapacity to work of 4 consecutive days. Where these requirements are not met, payment to reimburse any locum cover costs would be discretionary (see section 2.8).
2.5.6 Where these requirements continue to be met under a phased or adjusted hours arrangement commissioners should continue to reimburse locum cover costs as per paragraph 2.4.1 above.
2.6 Further discretionary payments
2.6.1 This protocol details (as required under part 7 paragraph 22 of the SFE) a number of policies the commissioner is obliged to set out:
- how the commissioner is likely to exercise its discretionary powers to make payments (including top-up payments) in respect of locum cover for parental or sickness leave, where it is not obliged to make such payments
- where the commissioner is obliged to make payments in respect of cover for parental or sickness leave pursuant to part 4 of the SFE, the circumstances in which it is likely to make payments of less than the maximum amount payable
- how the commissioner is likely to exercise its discretionary powers to make payments in respect of cover for absent GP performers, which is provided by nurses or other health care professionals
- how the commissioner is likely to exercise its discretionary powers to make payments to a partner or employee who is providing locum cover
- how the commissioner is likely to use its discretionary powers to make payments in respect of long-term sickness leave exceeding 52 weeks
- how the commissioner is likely to exercise its discretionary powers to make payments in respect of a sole practitioner who is absent for the purposes of attending an accredited postgraduate educational course
2.7 Discretionary powers in respect of cover for parental and sickness leave
2.7.1 The commissioner has the discretion to make payments in circumstances where it is not obliged to under the terms of the SFE, including top-up payments above the level of the agreed weekly maximum.
2.7.2 The commissioner may exercise these discretionary powers to make payments only in exceptional circumstances, for example (but not limited to) consideration of:
- demonstrable financial hardship
- areas of significant deprivation
- GP recruitment difficulties
- applications from single-handed GPs
- applications from nurse-led PMS practices
2.7.3 Where practices plan to apply for reimbursement in such circumstances, they should always ensure they have written agreement from the commissioner prior to arranging cover.
2.8 Discretionary payments in respect of cover for employed GP performers on phased return or adjusted hours arrangement following sickness absence
2.8.1 The commissioner has the discretion to make payments where employed GP performers are returning to work under a phased return or adjusted hour’s arrangement following sickness absence.
2.8.2 The commissioner will make payments in the following circumstances:
- the employed GP performer’s phased return or adjusted hours arrangement directly follows sickness absence leave which attracted a locum payment under section 10 of the SFE
- where the phased return or adjusted hours arrangement has been advised under a fit note (and for the period only that fit note covers or advises)
- where the contractor is paying the employed GP performer their full salary in respect of their phased return or adjusted hours arrangement, ie taking account of both working and sickness absence days/sessions
2.8.3 In these circumstances the commissioner will pay the lower of actual invoiced costs or maximum amounts payable calculated in line with paragraph 2.4.1.
2.9 Circumstances where it is likely payments will be less than the maximum amount payable
2.9.1 The commissioner will pay the maximum amount payable except in the following circumstances:
- Where actual invoiced costs are less than the maximum amount payable, then the commissioner will pay the actual invoiced costs subject to the provisions of this protocol including the bullet points below:
- With respect to parental leave, where the commissioner agrees to make payments for any week between weeks 27 to 52 for cover for additional maternity leave or adoption leave, the commissioner will pay the lower of either 50% of the weekly rate it paid for weeks 3 to 26 or 50% of the actual invoiced costs.
2.10 Payments for locum cover provided by nurses or other healthcare professionals
2.10.1 The commissioner will not pay for cover provided by nurses or other healthcare professionals.
2.11 Payments to a partner or employee who is providing cover
2.11.1 Where a contractor wishes to engage the services of a partner or shareholder in, or an employee of, that contractor, payments will be made to the GP practice in accordance with the normal provisions set out above. However, the GP performer providing cover would only be permitted to work up to the full-time limit of 9 clinical sessions per working week. The maximum of 9 clinical sessions per working week is to include any existing/normal commitments by the GP performer providing the cover.
2.12 Discretionary payments in respect of long-term sickness leave exceeding 52 weeks
2.12.1 Where a GP performer is on long term sickness leave, and locum payments are no longer payable under section 10 of the SFE, it will be at the commissioner’s discretion whether to continue to make payments.
2.12.2 In any case, those payments will not exceed the half rate payable in the second period of 26 weeks under paragraph 10.7(b) of the SFE, or the amount that would be payable under the NHS Pension Scheme regulations if the performer retired on ground of permanent incapacity, whichever is the lower.
2.13 Discretionary payments in response of sole practitioners who are absent for the purposes of attending an accredited postgraduate educational course
2.13.1 The commissioner will not pay for locum cover in respect of a sole practitioner’s attendance at an accredited postgraduate educational course.
2.14 Claims and payments
2.14.1 For parental leave, payments start from the day the GP performer goes on parental leave for the periods set out above and payment weeks are 5 working days.
2.14.2 For sickness leave, payments start 2 weeks from the day the GP performer goes on sick leave for the periods set out above and payment weeks are also 5 working days.
2.14.3 A sample claim form is at annex A. Frequently asked questions are available in annex C.
3 Guidance note: GP practices serving atypical populations
3.1 Introduction
3.1.1 Purpose of this document
3.1.2 The general medical services (GMS) funding formula (Carr-Hill formula) is an attempt to fund practice workload, regardless of the population they serve. It applies to the vast majority of the UK, but there are some practice populations that are so significantly atypical that using the GMS funding formula would not ensure the delivery of an adequate general practice service. This working group has looked at three such atypical populations: unavoidably small and isolated; university practices and those with a high ratio of patients who do not speak English.
3.1.3 Support for practices should directly impact on patient care as well as the long-term viability of practices, and therefore commissioners are encouraged to undertake a review of identified practices in their area. By reviewing the practices in your area, commissioners and providers can identify practices that require such support. Without this support, many practices will be unable to maintain the service and as a result, health outcomes may suffer.
3.1.4 Background to this work
3.1.5 Whilst the vast majority of GP practices serve communities that have common characteristics and work to contracts that have similar terms, conditions and funding arrangements, a small cohort of practices provide services to a patient population which is sufficiently demographically different to result in particular workload challenges that are not always recognised in the practice’s existing contract/s or its funding allocation. A population that triggers ‘uncommon’ workload challenges that are not experienced by the majority of GP practices is referred to here as ‘atypical’.
3.1.6 This document was produced to assist commissioners of 3 such atypical ‘populations’ by detailing the challenges faced by providers and offering examples of either provider or commissioner reports that may help either articulate or address these pressures. How members of the public relate to, and use GP services is influenced by the accessibility of other services including, for example, pharmacy, A & E, walk-in centres, and voluntary agency support infrastructure.
3.1.7 The populations are:
- unavoidably small and isolated
- university populations
- practices with a significantly high ratio of patients who do not speak English including those services designed to address the needs of migrants
- 3.1.8 This document guides commissioners to the types of issues and data sources they could consider in coming to a judgement about the support that is relevant to their circumstance, where commissioners and individual practices have a shared concern about meeting the health needs of their patients
3.1.9 This document outlines the additional needs of these patient groups, the pressures that providers face and the duty on commissioners to secure quality services which may legitimately require consideration of additional funding support.
3.1.10 In reading this document, commissioners and providers should be aware that services should be equitable for all population groups in line with the Public Sector Equality Duty (PSED) under the Equality Act 2010 and have regard to reduce health inequalities under the Health and Social Care Act 2012.
3.1.11 Promoting equality and addressing health inequalities are at the heart of NHS England’s values. Throughout the development of the policies and processes cited in this document, we have:
- given due regard to the need to eliminate discrimination, harassment, and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it
- given regard to the need to reduce inequalities between patients in access to, and outcomes from, healthcare services and in securing that services are provided in an integrated way where this might reduce health inequalities
3.1.12 In addition, this guidance is designed to complement but not duplicate or replace other related support initiatives. As such it does not advocate any one service model over another, specify or advocate specific funding arrangements, specify financial arrangements for managing the workload associated with temporary residents or describe how to distribute the national programme funds (General Practice Resilience Programme £8 million per annum) supporting struggling practices to improve their sustainability and resilience over the short/medium term.
3.1.13 Call for evidence
3.1.14 Where available, this document also describes some examples of innovative practice to overcome challenges associated with serving the atypical populations. Hyperlinks to further information are included in this document where available.
If commissioners have further examples of local initiatives to address issues associated with ‘atypical practices’, please submit them to england.gpcommissioning@nhs.net with the heading ‘Atypical populations: call for evidence’. Suitable case studies will be published on the Learning Environment website as a resource for commissioners and providers.
3.1.15 To complement these case studies NHS England will consider the viability of commissioning a more detailed investigation into these cohorts of patients to properly understand the difference in workload and related pressures not recognised in the funding formula.
3.2 Context: general medical services (GMS) funding formula review
3.2.1 Commitments to reviewing primary care funding.
3.2.2 NHS England has committed to reviewing the GMS funding formula which underpins the capitation payments made to GP practices under the general medical services (GMS) contract. This commitment was confirmed in the General Practice Forward View. We are working with the BMA’s General Practitioners Committee, NHS Employers, the Department of Health and Social Care and academic partners on the review to develop a formula that better reflects factors that drive workload, such as age or deprivation.
3.2.3 Existing GMS funding formula (introduced in 2004).
3.2.4 The intention of the formula was to weight remuneration to reflect the comparative practice workload, complexity and the relative costs of service delivery based on the demographics of the patient list. As such the formula has 2 parts:
a. a workload part that provides an estimate of the workload for each GP practice based on its list size and various patient and practice characteristics
b. a cost part that adjusts the payment for workload for variation in costs experienced by practices in different places
3.2.5 The workload part is also used to inform the primary medical services component of the primary care allocation formula. It is recognised that due to the wide diversity of populations serviced by GP practices, a national formula will never be able to accommodate the workload needs of all practices, hence the need for guidance on atypical practices.
3.2.6 What does the GMS funding formula not achieve?
3.2.7 It has been suggested that the GMS funding formula could be improved upon in a number of ways:
- the data that make up the formula requires updating (some of the data are more than 10 years out-of-date)
- factors currently included do not adequately reflect the workload associated with older people who may not be living in nursing or residential care and have a range of complex co-morbidities
- the impact of deprivation has been questioned and all the weightings will need to be reviewed
3.2.8 It is acknowledged that no formula will address the characteristics of ‘atypical’ populations hence this guidance.
3.3 Background to developing this document
3.3.1 A joint workshop between NHS England, the British Medical Association’s (BMA) GPs’ Committee, Local Medical Committee (LMC) representatives and NHS Employers was convened in September 2015 to:
- provide a list of propositions on atypical practices and views on whether these could or could not be reflected in a formula
- identify those characteristics that will never be fully met by a formula
- aid a description about the characteristics of a practice where it is likely that some additional support is required due to the practice characteristics not being fully recognised by any formula approach
3.3.2 The information used at that workshop has been used as the basis for this paper focusing on 3 specific cohorts, agreed with the BMA’s GPs’ Committee:
- unavoidably small and isolated (from other practices and other NHS services) with static populations
- university practices
- practices with a significantly high ratio of patients who do not speak English including those designed to address the needs of migrants (asylum seekers are excluded from the scope of this work as it is recognised this group requires a more specialised service)
3.3.3 These populations were chosen as priority areas because:
- small and isolated practices have challenges when meeting demand from dispersed rural communities. Opportunities to develop primary care working ‘at scale’ are more limited and population growth is slower, impacting on the available primary care budget
- anecdotal evidence tells us that university practices (campus-based services) have a population that consults general practice more than expected for their age and health (eg in terms of mental health and sexual health issues)
- practices supporting a significant number of patients that do not speak English have operational complications associated with communication problems (this also links to a separate NHS England work stream on translation and interpretation)
3.3.4 A working group was convened in Spring 2016, comprising NHS England and local commissioners, LMC representatives, a BMA representative, and a Royal College of General Practitioners (RCGP) representative.
3.3.5 The working group was chaired and administered by NHS England.
3.4 Identifying ‘atypical’ populations locally
3.4.1 Because of the degree of variation nationally in terms of health and social care economies and patient expectation, demand and behaviour, there is no one method of identifying which populations could be considered as atypical. There are however a number of examples of how commissioners have scoped the issues and what data sources they have used (an example from Devon can be found on the Learning Environment’s case studies pin board).
3.5 Unavoidably small and isolated
Description of the Issues
3.5.1 Practices serving small but dispersed populations have limited ways in which to influence their income or costs yet provide a vital primary care service.
3.5.2 Their funding is governed by their registered list (global sum/QOF payments) which, by the nature of their geography, cannot be expanded and may compromise the ability to deliver quality care and exacerbate workload pressures.
3.5.3 Because of their location they are often serviced by small B class roads, potentially making travel difficult and time consuming for patients and service providers.
3.5.4 Many such communities do not have easy access to a pharmacy or an A&E department, ambulance access and response times can be longer than in an urban environment and community services are diluted.
3.5.5 Public transport makes it difficult for patients to attend outpatient departments and other health facilities. As a result, some patients tend to rely on practices to provide a wider range of services than is normally regarded as ‘core’ general practice and staff require regular training to maintain their skills for providing first response in the absence of A&E. It may be hard to measure this effect, but it can be summarised as a greater independence by patients from hospital care and a higher level of intervention and support from the practice.
3.5.6 Engagement of GP locums or recruitment of successors to a contract can be problematic because of geographic isolation, income, and potential workload pressures. It is recognised that country or island life is not everyone’s preference.
3.5.7 Housing costs associated with ‘desirable’ or expensive country or island locations can also negatively impact on recruitment of practice administrative staff.
3.5.8 Some rural locations attract itinerant workers who may not speak English, have no accessible medical record and consultations take longer.
Information/data considerations
3.5.9 Here are some data sources or information that you may wish to consider when trying to define if a population is atypical:
- the average population density and the average distance from patient residences are both available for individual practices and, when considered in conjunction, may produce some useful insights. It should be noted that population density is measured in persons per hectare (calculated from the population density of the relevant electoral ward) and distance to main surgery is measured in 100 metre units (as the average distance from patient’s home to main surgery location). It may be useful to consider practices that rank in the top percentiles for both indicators, to help in reaching a judgement about relative rurality and isolation. These data are available as an extract from the Exeter system
- ambulance response times (available from the local ambulance trust on request by the lead commissioner ICB in your area)
- current service profile: does the practice provide additional or extra services that are not commonly available in other practices and not additionally funded. Could these be captured in a bespoke enhanced service, set of KPIs, or added formally into a PMS agreement? Examples may relate to the absence of locally accessible health and social care services
- data sources that you could use to compare practices in your area include:
- General practice expenses, GMS and PMS contracts in England 2013/14 (NHS England, published July 2016)
- NHS payments to general practice, England, 2017/18 (NHS England, published Dec 2018)
Case studies
3.5.10 The case studies listed below are not an exhaustive list. Commissioners and providers can review these case studies, tailor them to their local area as required, and/or decide on other support arrangements that might be appropriate:
- Contract for primary care support to secondary care (eg pre-operative assessments, post-operative wound checks, and suture removal).
- The My Life A Full Life Programme is a collaboration between NHS Hampshire and Isle of Wight Integrated Care Board, Isle of Wight NHS Trust, Isle of Wight Council, Community Action Isle of Wight and other local voluntary sector organisations. It aims to change the face of social and health care on the Island, helping people live life to the full. Objectives are to achieve a more co-ordinated approach to the delivery of health and social care services for older people and people with long term conditions.
3.5.11 Village agent schemes or link schemes
- Bedfordshire: Supported 950 clients over the financial year (with an average of 3 visits per client) delivering a range of outcomes that included accessing health and housing services, getting home adaptations, obtaining mobility aids, take-up of benefits and tackling isolation through transport.
- Gloucestershire: The village agents support older people living in the area. Read reports on their projects and case studies. Polish speaking agents are employed to support the local Polish community.
- Wiltshire: The link schemes are community-based initiatives that aim to improve the quality of life for disadvantaged, elderly or infirm people by providing a structured good neighbour service delivered by volunteers from within the local community. The range of link scheme services varies from providing volunteer drivers to take someone to a medical appointment, taking them shopping or to visit an old friend, or simply providing good neighbour care. They aim to complement the provision of other services, whether statutory or voluntary.
Patient group observations
3.5.15 Support services provided by volunteers and community groups act as a link between statutory services and the local community (some examples are listed in the case studies section above). They are well-placed to work across various isolated groups and share good practice as needed. Services such as those in Dorset (Dorset Community Action’s Navigator pilot as part of the Better Together Programme) and the Isle of Wight (My Life A Full Life)) operate at a strategic level to bring providers and commissioners together to address issues and find solutions. The key challenge is that all these services need support from commissioners and funding in some way so that there is a whole system approach. This support is not free but can be tailored to meet the needs of statutory providers and help to fill gaps and is cost effective, flexible, and resourceful in its approach.
Provided by Paul Dixon, Action with Communities in Rural England
3.5.16 All Our Health is a resource that helps front-line health and care staff use their trusted relationships with individuals, families and communities to take action on inclusion health.
3.6 University populations
Description of the issues
3.6.1 Some practices serving university populations are not able to earn as much QOF funding due to the low prevalence of diseases. There is an assumption by some that service provision is less onerous due to low disease prevalence.
3.6.2 Anecdotally, it is believed that:
- since many students are living independently for the first time, this can be a time when they experiment by engaging in behaviours that affect their health and need for service interventions, eg around alcohol and drug use and sexual activity, leading to a higher-than-average demand for services related to these. In addition, for students who do not have access to immediate family support, there can consequently be a greater need for primary care services especially in respect of mental health support
- students can present with minor ailments or with seemingly unfounded worries about their wellbeing. For those who have moved away from home and are living independently for the first time, it is important that they are provided with information about the range of primary care services available including pharmacy as well as online sources of support (ie supported to develop ‘health literacy’)
- a significant number of students with long term and complex health needs attend university (eg cystic fibrosis, transplants, multiple sclerosis, asthma, diabetes) and transition to new primary care and secondary care arrangements, if they are leaving home, is important as is support for the transition to adult services which can take place during the university years
- for foreign students, a lack of familiarity with the country and how health services work can create additional demand for GP practices to signpost patients to more appropriate services or lead foreign students to go directly to A&E which leads to additional demand on ICB resources.
- In addition, some foreign students may have greater health risks/needs (eg tuberculosis, hepatitis)
- Additional administrative effort required to register large numbers of new patients in September/October and de-register in the summer.
Information/data considerations
3.6.3 Here are some data sources or information that you may wish to consider when trying to define if a population is atypical:
- comparative consultation rates (if local data available)
- prevalence of disease not covered by QOF, particularly common mental health disorders
- per-patient weighted funding level provided by global sum
- registration data in September – October to identify student registrations and de-registrations over the summer
Support initiatives
3.6.4 The case studies listed below are not an exhaustive list. Commissioners and providers can review these case studies, tailor them to their local area as required, and/or decided on other support arrangements that might be appropriate.
- promotion of online support tools for young people, eg NHS Go app
- using technology to reduce administration, eg text message results service, online administration, eg updating address) (University Health Centre, Sheffield)
- local QOF or local enhanced service for specific needs of the population
- skype consultations, eg Newham’s young people with diabetes project
- shared care between ‘home’ and university-based health care services can help support adherence of and management of long-term conditions for young people
Patient group observations
3.6.5 There is a risk that primary care practitioners expect young people to behave in a particular way. It is important that assumptions are not made about young people based on their age or that all university students behave the same way.
3.6.6 The issue that a young person may present with may not be the real reason they have attended. Young people need to feel confident to trust a clinician. Clinicians need to be skilled in recognising where there may be an underlying issue and give the young person the confidence to reveal it during a consultation.
3.6.7 Young people are undergoing a significant transition when they start university and having a trusted primary care practitioner to talk to can be extremely significant. They need to have information about the range of health services that exist so that they can be confident to seek help from primary care, pharmacy, A&E etc.
- young people may wish to attend services with their peers. Practice staff should not be surprised if students attend in a group to support each other using health services, in the same way that younger children attend with a parent or carer. If a peer wishes to sit in on a consultation, clinicians should ensure that part of the consultation is with the patient alone – this would also be recommended for young people attending consultations with parents or carers
- there is a unique opportunity to increase university students’ awareness of how to use health services appropriately which has long term benefits for the health service
- young people with long term conditions need to access repeat prescriptions quickly when they move to university to avoid gaps in medication. Foreign students don’t always recognise drug brand names and often do not understand how to access medication
Provided by Emma Rigby, Association for Young People’s Health
3.7 Practices with a high number of patients who do not speak English
Some practices have a high ratio of patients who do not speak English, including practices designed to address the needs of migrants.
Asylum seekers: The working group had initially intended to include asylum seekers as part of the non-English speaking atypical group. However, it became clear that the needs of asylum seekers may go beyond primary “ordinary” care. There are often significant levels of post-traumatic stress disorder (a result of trafficking, torture, violence, rape (for women, children, and men) and illness (eg HIV, hepatitis B/C, TB).
Note: A separate work stream to this atypical population work stream is ongoing in NHS England’s Primary Care Commissioning team on translation and interpreting services. Further information can be found on the NHS England website. Another separate work stream to the Primary Care team’s translation and interpreting project is ongoing between the Race Equality Foundation and NHS England’s Equalities team to scope the viability of a community languages information standard.
3.7.1 Description of the issues
- the need for an interpreter means that all conversations take longer and increases the cost of each patient contact (in relation to the time taken and the cost of interpreting)
- if interpreting is not available, miscommunication increases the risk of patients not attending follow up appointments and delayed access to care
- surrounding support services (eg improving access to psychological therapies, obesity management) and literature are usually in English, thus necessitating the development of additional in-house support
- lack of literacy, both in English and for some groups their native language removes the value of written material normally used to reinforce appropriate access (eg, appointments) and health advice
- in addition, the lack of cultural understanding of the NHS requires extra support, signposting and often the recalibration of patient expectations
- some patients have a basic lack of health education – for instance, no knowledge of terms that describes cholesterol or calories, or the importance of taking medication correctly
3.7.2 Information/data considerations
Here are some data sources or information that you may wish to consider when trying to define if a population is atypical:
- evidence of languages spoken and percentage of list
- percentage of patients requiring an interpreter (recognising that the level of support may decrease over time for some patients as they learn English)
- consultation rates compared to the average and whether different language groups consult more, and what the reasons may be for this
- reported average length of consultation
- demand for interpreting (spoken word) and translation (written word) support services and growth in demand over time
3.7.3 Examples of support
The examples cited below are not an exhaustive list. Commissioners and providers can consider these, tailor them to their local area as required and/or decide on other support arrangements that might be appropriate.
- funding that recognises increased consultation times/access
- education materials available in community languages
- acknowledgement of costs associated with interpreting, either in contractual payments or a provided service (local enhanced service)
- Public health support for staff to help manage different needs of patients (eg, hepatitis B vaccinations)
- additional training for staff in public health messaging/realistic health interventions, eg patient issues surrounding diet, behaviours, and expectations of services
- screening for patients new to the UK for communicable diseases
- staff training on the use of interpreters particularly recognising where a patient is uncomfortable with the interpreter and knowing what action to take if staff question the quality of the interpreting service
- bi-lingual receptionist or in-house interpreting
- bi-lingual patient health questionnaires have been developed for commissioners and GP practices to support initial health assessments and management of newly registered vulnerable migrants, including people seeking asylum and those arriving under government relocation schemes. There is also an English/blank version of the form so that it may be translated into different community languages where local needs require. These can be found on this NHS England website
3.7.4 Patient group observations
Professional interpreters are the preferred means of communication and may also have knowledge of medical language. In addition, family interpreting may not be appropriate where the procedures or consultations are of a sensitive or intimate subject. Family interpreters may have no, or limited, medical knowledge.
Provided by Samir Jeraj, Race Equality Foundation
3.8 Conclusion
We hope that this document will enable local commissioners to identify and support the practices that serve these populations in order that patients will continue to receive effective primary care. Further examples of case studies can be submitted to the Primary Care Commissioning team: england.gpcommissioning@nhs.net .
3.9 Notes for NHS England commissioners
When discussing this topic locally, please be aware that you may need to review equalities and health inequalities and the 13Q duty to consult. Copies of supporting documents completed for this project are available in the project files. Please email the Primary Care Commissioning team for more details: england.gpcommissioning@nhs.net.
4 Provision of occupation health services
4.1 Introduction
4.1.1 Occupational health (OH) is “a specialist branch of medicine focusing on the health of staff in the workplace. OH, professionals aim to find out what impact work has on staff health and make sure that staff are fit to undertake the role they are employed to do both physically and emotionally. OH, specialists can support organisations through advising on work-related illnesses and accidents, carrying out assessments for new starters and existing employees, monitoring the health of employees and prevention. OH, services are also used to assist organisations in managing both short and long-term absence situations”. (NHS Employers).
4.1.2 “Employers are required by law to prevent physical and mental ill health in their workers that may occur as a result their business activities. An important part of occupational health is concerned with how work and the work environment can impact on workers’ health, both physical and mental. It also includes how workers’ health can affect their ability to do their job. In health and safety law, there are things organisations must do to make sure workers’ health is not adversely affected by their work and that workers are medically fit to carry out their work safely. This includes:
- implementing health or medical surveillance when necessary, ensuring workers are medically fit to undertake the role required (your industry may produce such standards)
- reviewing your risk assessment when a worker is returning to work following sickness absence or declares a health condition
- have a responsibility to make available occupational health services for their staff and it is important that staff know how to access their service provider”. (Health and Safety Executive)
4.2 Provision of occupation health services – services funded by the primary care contractor
This section outlines what primary care services contract holders are responsible for funding as part of their employer responsibilities to their staff. These services include:
- OH, pre-employment screening/clearance: OH assessments as required for all staff working in their organisation, as required
- virology testing, vaccination for blood borne viruses (BBVs) and immunisation: available to all staff who are not already immunised, and includes hepatitis B, varicella, tuberculosis (BCG), diphtheria, pertussis and tetanus, measles mumps and rubella
- enhanced/other OH assessments: this may include a range of different OH assessments or support needed for all staff including:
- assist in the appropriate placement of people at work, considering their physical and mental health, and prevent ill health arising as a result of work done or the conditions in which work is done
- enhancing staff performance and morale through reducing risks at work which lead to ill health, staff absence and accidents
- protect the public from any adverse consequences arising as a result of ill health or infected primary care staff
- review prolonged/recurrent sickness absence and support return to work after sickness absence or following an accident
- advice on ill health retirement
- periodic health assessment for example: radiation, COSHH regulations or where risk assessment has indicated that this is required
- advice on onward referral to other services that could support staff, eg counselling
4.3 Provision of specific occupation health services – applicants to join the national performers list
Performers seeking to apply to join the national performers list (NPL) will need to self-fund for the following OH services:
- pre-employment screening
- virology testing
- vaccination for BBVs
- immunisation
4.4 Provision of specific occupational health services – funded by the commissioner
4.4.1 For all primary care staff (general practice, community pharmacy, dentistry and optometry): management of staff on exposure to and working with BBVs: this includes specialist support for the management of staff who have a BBV, and urgent and longer-term advice to all staff working in primary care settings (including trainees) on exposure to potential BBV, eg following needle stick injury. Post exposure risk assessments, blood testing, and post-exposure prophylaxis (PEP) treatments are included. Mainstream NHS services are responsible for ongoing treatment if BBV contracted (eg, anti-retroviral medication).
4.4.2 For performers already on the national performers list: OH, services funded by the commissioner include: virology testing, vaccination for BBVs and immunisation.
4.4.3 For performers who are under review or investigation by responsible officer/medical director: Any OH referrals made by responsible officer/medical director in respect of formal proceeding as part of the national performers list.
Summary of ‘who pays’ for what occupational health services
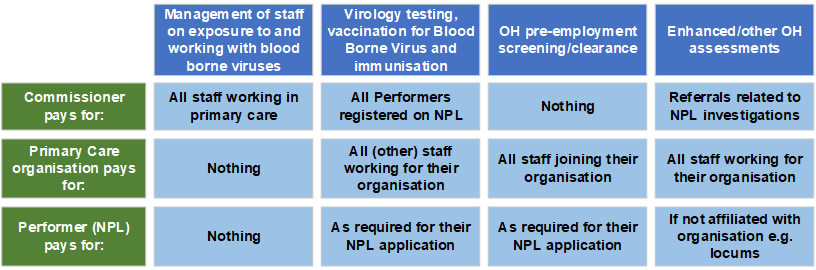
4.5 Role of the commissioner in enabling occupational health access for primary care workforce
Joint approach to procuring OH services
4.5.1 Although the different OH provisions are a shared responsibility, ie commissioners fund part and primary care organisations fund part, commissioners should take steps to support primary care staff to access OH services in a consistent and efficient way.
4.5.2 Commissioners are much better placed to procure system-wide OH services on behalf of primary care organisations and should enable this by procuring OH service providers for all OH requirements set out above, with the option for primary care organisations to access these OH services on a fee basis for services they’re responsible for funding.
4.5.3 It is strongly advised that commissioners collaborate with other primary care commissioners (ie, general practice, community pharmacy, dentistry, and optometry), and local NHS organisations/ integrated care boards (ICB) to ensure a cross-system sustainable and consistent access to OH services.
We have previously published a service specification for OH in primary care; we are currently reviewing this to better align to the work of the NHS people plan and system transformation.
4.6 Good communications are essential
Commissioners must ensure information about how to access OH services are clearly communicated to primary care organisations and their staff. Many believe OH services are not available in primary care, which is not true. We must therefore do more to promote OH services available; As a minimum this should clearly present information as set out below, but you should work with your OH supplier on promotional materials and posters as required:
Urgent occupational health services
- management of staff on exposure to and working with blood borne viruses, eg needle stick injury
Routine occupational health services
- virology testing, vaccination for blood borne virus and immunisation
- occupational health pre-employment screening/clearance
- enhanced/other occupational health assessments
Working hours
- contact phone number and instructions
Out of hours
- contact phone number and instructions
Occupational health supplier
- supplier name
- supplier phone number
- supplier email address
- supplier website
For any queries contact england.gpcommissioning@nhs.net
Publication reference: PRN00613

