Introduction
Same day emergency care (SDEC) allows specialists, where appropriate, to assess, diagnose and treat patients on the same day of arrival who would otherwise have been admitted to hospital. It is part of a wider UEC system that should be fully integrated locally to deliver the core principle of patients being seen by the right team first time.
The SDEC model was adopted nationally by NHS England in 2019 to accelerate the work previously delivered in walk in emergency care services. It is now a widely accepted model of care and credible alternative to admission for those patients who can be seen, treated and discharged on the same day as arrival to hospital.
SDEC supports early senior clinical decision-making through direct access and referral to/from SDEC services by maximising the opportunity to complete patient care on the same day. A patient may need to return to hospital for additional treatment and monitoring where clinically appropriate as part of their ongoing care. This often means patients do not attend other urgent and emergency care (UEC) services inappropriately such as the emergency department (ED) or urgent treatment centre (UTC). Virtual wards should be aligned to SDEC to ensure patient transfer is seamless.
1 Service specification: overview
1.1 This specification defines what should be delivered as part of the SDEC service. It includes links to reference documents and metrics for measurement (the desired outcomes and outputs) so that safe, effective same day services are delivered across healthcare systems to deliver UEC services.
1.2 It offers guidance to support local systems and providers to deliver a standardised model of SDEC and, wherever possible, to see and treat and stream directly clinically appropriate patients in SDEC.
1.3 Using available data, evidence and clinical expertise, the aim is to reduce pressure on the inpatient bed base, as well as ensure patients are directly referred or redirected to SDEC.
1.4 The specification is for providers and integrated care boards (ICBs)/integrated care systems (ICSs) to use, and will help all SDEC services, including those co-located (paragraph 2.4) to build on emerging policy to support alternatives to admission. The minimum requirements are:
- SDEC is a dedicated specialty assessment process.
- SDEC assessment is delivered by teams that integrate with the delivery of a comprehensive specialty assessment function (for example, bedded assessment units).
- SDEC is delivered within an appropriate environment designed to deliver the most efficient assessment processes.
2 Scope
By April 2024 every acute hospital with a Type 1 Emergency Department (ED) will move to a comprehensive model of SDEC for a minimum of 12 hours a day, 7 days a week.
2.1 This service specification covers the provision of adult SDEC services (excluding acute frailty services).
2.2 The overarching principle of SDEC is that all patients who attend UEC services can be referred to be rapidly assessed, diagnosed, and treated without being admitted to a ward, and if clinically safe to do so will go home on the same day of arrival.
2.3 SDEC is not an elective outpatient service and does not treat patients on an elective pathway (unless the patient presents with an acute exacerbation of illness).
2.4 SDEC provides in-hospital care within:
- a stand-alone unit
- a combined or co-located SDEC with the acute medical unit
- acute surgical unit/surgical assessment unit
- acute frailty unit
- ED
2.5 SDEC enables swifter access to clinicians as well as diagnostics and investigation as early as possible in the clinical pathway. Enhanced response from specialists such as cardiology, respiratory disease, gastroenterology, endocrinology and general surgery should be provided as a minimum, to complement care if the patient needs to be admitted as part of their treatment plan.
2.6 SDEC supports all non-elective activity with a zero-day length of stay (0LoS) from arrival in hospital. Providers should regularly review patient activity with a +1–3 day in-hospital LoS as some admitted patients may be suitable for same day care.
2.7 SDEC should work closely with providers in community and primary care settings, utilising physical and virtual capacity.
3 Care pathways and patient selection
3.1 Care pathway
3.1.1 SDEC services are delivered within discrete locations such as SDEC units, EDs or combined SDEC units (including co-located SDECs). Sometimes these services are dedicated to one specialty, for example medicine, but increasingly surgical and medical specialties (including those for older patients living with frailty) are clinically integrated into a single SDEC service/footprint within the hospital. Additional internal professional standards that may exist for specialty focused SDECs will not be covered in this specification.
3.1.2 As a minimum the following SDEC services should be provided:
- medical
- surgical
- acute frailty
- obstetrics and gynaecology (including early pregnancy)
- urology
- oncology
- orthopaedics
- paediatrics (a separate service specification)
3.2 Patient selection
3.2.1 Patient selection is a key step in ensuring that those most likely to benefit can access SDEC. It should consider any stable patient requiring acute admission but who can safely be treated on the same day.
3.2.2 Referring or streaming the ‘wrong’ patients to SDEC will limit the capacity for patients who would benefit most. With this in mind, robust gatekeeping processes are needed to ensure the right patients are referred or streamed to the service. The following groups should not be managed in SDEC:
- Type 2 and Type 3 ED attenders. These patients should continue to receive their care in ED/UTC within the 4-hour standard.
- Type 1 ED patients who will breach the 4-hour standard and are awaiting ward admission (inpatient specialty).
- clinically unstable patients
- patients who are awaiting discharge or transfer; SDEC is neither a discharge lounge nor an ‘overflow’ unit for other services
3.2.3 Patient safety is paramount in the decision-making process. A patient’s suitability for SDEC is based on a clinical decision that balances the clinical benefit for inpatient care. It is predicated on whether an admission to hospital is the safest outcome for the patient, and is the key selection criterion for treatment in a same day environment. The assumption that admitted care is the most appropriate and safest environment for the patient may need to be challenged. If a patient does not need ‘in-hospital’ care, the senior decision-maker should consider a virtual ward as an alternative.
3.2.4 The local provider should set appropriate thresholds for the severity (acuity) of patients who can be seen in SDEC, although clinical consensus suggests that patients should be deemed SDEC appropriate until ruled out for an alternative clinical setting (excluding those listed in paragraph 3.2.2). Some providers use the National Early Warning Score version 2 (NEWS2) <5 as the threshold for medical patients, and where appropriate the referring specialist discusses a patient with a higher score with a senior clinical decision-maker. All decisions on thresholds should be influenced by the wider care environment and the workforce model.
3.2.5 Patients with complex social and functional needs, including those will mental ill health, dementia or who are at end of life, should not to be excluded from SDEC. These groups are potentially well served by a same day environment as it avoids admission and the deconditioning associated with long lengths of stay, as well as disruption to care packages. Using SDEC rather than admission allows community-based care to continue without interruption when the patient needs a period of emergency assessment and intervention in secondary care. There are opportunities to use the flexibility of SDEC to manage older people living with frailty in a way that is planned, personal and less distressing for them.
3.3 Referral to SDEC
3.3.1 Referral guidance should be in place to support easy access to SDEC from all healthcare settings, both direct and indirect. This should be communicated and reviewed regularly to increase learning, reflect system maturity and maximise appropriate referrals.
3.3.2 The NHS England Surgical and Medical Alternative Route Tool (SMART) was launched in March 2024 to support providers with an insight into the opportunity available within hospital sites to maximise SDEC activity through high volume pathways.
3.3.3 SDEC services can be delivered across acute hospital and community settings face to face, virtually or with a mixture of the two.
3.3.4 Senior clinical decision-makers are essential for the rapid identification and streaming of patients to and from SDEC, they need to be present in both SDEC and referring services. Senior clinical decision-makers should have the autonomy to admit, diagnose, formulate a management plan and refer patients onwards or discharge them from the service. They should also be able to provide advice and/or guidance to other healthcare colleagues around patient care.
3.3.5 Care pathways should be streamlined to promote early identification of SDEC patients, with multiple triages, clinical assessments and handovers avoided to reduce patient delay as well as improve clinical continuity.
3.3.6 Clear referral pathways should be implemented and agreed to maximise the use of direct referral from NHS 111, primary care, community services, virtual wards and 999 to other hospital services (including SDEC and specialty hot clinics).
3.3.7 SDEC should maximise the referral window to ensure patients can access same day care while the service is operational for a minimum of 12 hours a day, 7 days a week.
3.3.8 Patients who the responsible clinician deems clinically appropriate for SDEC can be directly conveyed following a clinical conversation. Every effort should be made to ensure the patient is transferred to the appropriate care setting and EDs are only used where clinically appropriate. We recognise some organisations have moved to a trusted assessor model for receiving referrals, removing the need for a clinical conversation and further reducing delay. Where a patient is directly referred without a clinician-to-clinician conversation, this should be supported by digital referral systems that provide an audit trail and transfer the full patient referral prior to the patient attending SDEC. National policy will be developed to support this development of referral guidance in due course.
3.3.9 When making a referral to SDEC, the clinician should routinely consider using an SBAR (situation, background, assessment, recommendation) approach to support decision-making.
3.4 Direct referral
3.4.1 To enable referring clinicians to have a clinical discussion, the SDEC should provide a direct contact number. The clinical discussion is the key to ensuring the patient’s suitability for SDEC (unless the trusted assessor model is being used).
3.4.2 The SDEC clinician should support decision-making. SDEC will not always be the most suitable service and there may be more appropriate services within the community or primary care.
3.4.3 For NHS 111/999 services, criteria for direct referral into each SDEC specialty should be provided via the Directory of Service, in collaboration with the accepting SDEC service.
3.4.4 All SDECs within the ICB should include medical, surgical and frailty. Specialist SDECs, for example oncology, could also be included.
- SDEC profiles should exclude life limiting or life threatening illness or injury (that requires immediate treatment or resuscitation).
3.5 Standards of referral
3.5.1 The below referral standards should be implemented to provide consistency and ease of referral into SDEC. ICBs are encouraged to take a wide view when considering appropriate use of SDEC for any patient where an admission is being considered.
3.5.2 Development of exclusion criteria should be led at ICS level to minimise variation and maximise appropriate access to SDEC.
3.5.3 The SDEC patient pathway decision-making tool (Figure 1) asks a series of questions. Where the answer to a question is no, a further question must be asked to determine if the patient is suitable for SDEC; and where the answer is yes, the patient is referred to an alternative service.
3.5.4 Ideally, initial assessment on arrival should ensure all patients are directed to the most appropriate setting first time. High volume pathways should be considered for referral as a minimum but not limited to the below:
- lower respiratory tract infection
- cellulitis review +/- intravenous treatment
- low risk community acquired pneumonia
- suspected pulmonary embolism
- anaemia
- gastritis
- low risk chest pain (non-cardiac)
- shortness of breath (COPD, heart failure, asthma)
- early pregnancy bleeding
- palpitations/hypertension/atrial fibrillation
- acute headache/migraine
- abscess (torso, perianal, pilonidal)
- suspect ureteric stone
- appendicitis
- suspect biliary colic/cholecystitis
- suspect diverticulitis
- neutropenic sepsis
- Hickman line procedures
3.5.5 NHS England Standard guidance for ambulance clinician referral to SDEC is available (October 2021).
Figure 1
Same Day Emergency Care (SDEC) Patient pathway decision making tool.
This has been designed to support decision making from Primary and Community Care, Ambulance services, Streaming in Emergency Departments and from Single Point of Access Services.
If the patient has a life-threatening injury or illness, call 999 immediately
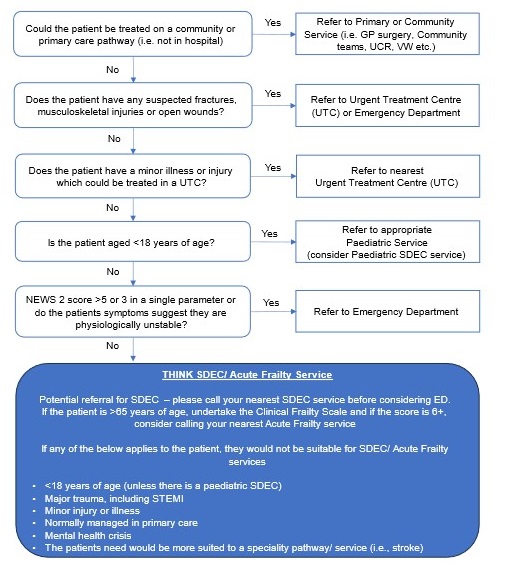
The flowchart begins with questions about the patient’s condition, such as whether they can be treated in a community or primary care setting, if they have suspected fractures or open wounds, and if they have a minor illness or injury.
The flowchart guides the user through various decision points, leading to different recommendations such as referring to a Primary or Community Service, Urgent Treatment Centre, Emergency Department, or Pediatric Service.
At the bottom, there is a blue box labelled “THINK SDEC/Acute Frailty Service,” which provides additional guidance for potential referrals to SDEC, especially for patients over 65 years of age or those with specific conditions like major trauma or mental health crises.
3.6 Discharge processes
3.6.1 Prior to discharge all diagnostic tests should be followed up and where onward referrals or additional diagnostics are required, these should be co-ordinated through the SDEC service. Reporting times will need to be responsive to same day care to avoid delay.
3.6.2 Following completion of the agreed treatment plan, patients will be discharged back to primary care, community care or a virtual ward for ongoing care where clinically appropriate.
3.6.3 Within a maximum 4 working days of completion of treatment, a comprehensive final report that includes diagnosis, management and recommendations will be sent to the referring GP/primary care clinician. Every effort should be made to complete reports within 1 working day.
4 Workforce
The SDEC workforce should be able to provide a safe service that can accommodate fluctuations in demand and volume patterns. A workforce plan will provide sustainable levels of appropriately trained and educated staff.
4.1 Staffing
4.1.1 The provider should ensure that the service is staffed by consultants, specialist and associate specialist doctors, doctors in training, allied healthcare professionals (AHPs) nurses, advanced clinical practitioners, physician associates, nurse specialists and support staff relevant for the specialty. Job plans should reflect the clinical commitments required to deliver the service for a minimum of 12 hours a day.
4.1.2 The team should be supported by administrative staff undertaking ward clerk, reception and clerical functions.
4.1.3 Every provider should have appropriate medical/nursing cover at all times, taking account of guidance from relevant expert or professional bodies.
4.1.4 The provider should ensure that staff have the correct professional registration.
4.1.5 The service should be led by an experienced competent senior clinical decision-maker to ensure timely decision-making.
4.1.6 The multidisciplinary team should have close relationships with community/primary/
UCR/virtual ward teams as well as mental health services.
4.1.7 Robust inter-professional standards should be in place to support specialty in-reach into SDEC.
4.2 Training
4.2.1 All staff should be appropriately trained to provide care, treatment and support.
4.2.2 The provider (along with the relevant professional body) should ensure that staff are competent practitioners and that they are fit to practise.
4.2.3 The provider should facilitate both mandatory and continual professional development (CPD) training for all staff.
4.2.4 Staff should carry out sufficient activity to maintain their competence in caring for patients, taking account of guidance from relevant expert or professional bodies.
4.2.5 The provider should give healthcare professionals the opportunity to attend clinical training sessions as part of their training programme.
4.2.6 Best practice providers deliver locality-based training events for all healthcare professionals to attend and accrue CPD points.
4.2.7 The provider should establish a professional forum for all staff who support same day provision of care across all specialties to share learning and best practice.
4.2.8 A training plan and web-based information should be developed by the provider to support:
- postgraduate education of all healthcare professionals
- access for undergraduate training at minimum of 2 weeks
- research programmes
- safeguarding
- initial assessment
4.3 Tools to support staffing
4.3.1 Supporting SDEC workforce planning reviews the tools available for staffing SDEC services.
4.3.2 The workforce modelling tool has been adapted to support SDEC. This supports SDEC services to optimise the skill mix, workload and redistribution, growth and cost comparisons against establishment.
4.3.3 The task and skill set framework supports SDEC services in reviewing their staffing models and to think differently about which roles in the service can undertake tasks along the patient journey.
4.3.4 The ECIST demand and capacity tool looks at the current and future workforce requirements for the SDEC environment, and identifies any gaps. It has been developed in MS Excel so that all NHS colleagues can use it at their convenience.
4.3.5 The NHS England safer nursing care tool is a NICE-endorsed evidence-based tool currently used in the NHS to determine optimal nurse staffing levels. It can also support organisations to deliver evidence-based workforce plans that help existing services assess workload in an SDEC facility and provides a visual representation of staffing.
4.3.6 The staffing model practice guide showcases how providers across England are restoring and improving their same day workforce.
4.4 Competency framework – nursing staff
4.4.1 The SDEC competency framework (2023) aims to strengthen SDEC by supporting the learning and development of the nursing workforce. It covers the skills and competencies that nurses will acquire through a career in SDEC.
5 Activity recording
We expect a year-on-year increase in SDEC activity. Providers that have yet to achieve a third of non-elective activity on average as zero-day length of stay (0LoS) should meet this minimum average by Q1 2024/25.
5.1 Defining SDEC pathways
5.1.1 SDEC pathways involve patients being streamed or redirected from another care setting such as ED, or directly referred following an urgent referral to one of the several units that typically have both seated areas and cubicles with trollies. Such units include, but are not exclusive to, acute medical units, surgical assessment units, frailty units, paediatric assessment units (not covered in this specification), oncology day units and early pregnancy assessment units.
5.1.2 The care needs of all patients may include ongoing assessment and observation, specialist assessment, and therapies and treatments that aim to maximise the opportunity for safe discharge in a timely way.
5.1.3 An SDEC service that is seeing and treating appropriate patients should have a conversion rate of 20–30% to admission. A lower conversion rate suggests a higher proportion of lower acuity patients are being seen in SDEC; that is, they are being treated in the wrong clinical setting.
5.1.4 When a patient attends a ‘hot clinic’ (one stop appointment) they may be referred for assessment/treatment on the same day. However, this will be recorded as an outpatient attendance, not an SDEC attendance, as admission was never the intention of the ongoing episode of care. From July 2023, recording of SDEC activity as outpatient activity ceased so that recording of all SDEC activity can transition to the Emergency Care Data Set (ECDS).
5.2 Activity reporting
5.2.1 Many providers classify most of their SDEC-type pathways as zero-day non-elective episodes of care within the Admitted Patient Care (APC) dataset. By July 2024 all providers should have transitioned recording SDEC activity on ECDS.
5.2.2 A proxy measure for SDEC-type activities that are recorded in APC is:
0LoS – All non-elective spells where the patient is admitted and discharged on the same day. This is limited to specific acute treatment functions.
5.2.3 To support providers to meet this requirement, NHS England has developed the SDEC Index and SMARToll that gives an overview of activity recording, by region and provider, using a combination of records in the APC dataset, outpatient datasets and ECDS. Providers and ICBs are asked to use this information to inform the continued development of SDEC recording on ECDS as Type 5 activity.
5.2.4 Patients may need to return to SDEC for continuing care: for example, follow-up for treatment or diagnostics. We expect ongoing care (that is, a multi-SDEC episode) to be coded using the Type 6 episode introduced in ECDS version 4, as this captures the ongoing duty of care to the patient.
5.3 Emergency Care Date Set (ECDS)
5.3.1 To improve recording of UEC services, ECDS is continually evolving to allow activity to be recorded accurately where patients present in non-ED settings. SDEC activity needs to be accurately recorded to demonstrate the positive impact all services have on improving patient flow, via a consistent dataset:
- in 2019, as part of the NHS Long Term Plan, the decision was taken to record SDEC using the ECDS, which had been designed for this purpose from its inception in 2014
- in 2017 the Type 5 ECDS was introduced, which enabled the counting of SDEC activity, and in 2023 the Type 6 ECDS episode to aggregate multiple attendances (multi-SDEC), which are an increasing feature of care
- in 2023, virtual attendances can be recorded as part of patient care, for example video consultations, and the concept of hot clinics has been introduced
An SDEC dashboard has been developed to help providers monitor their activity profiles.
5.4 Recommended metrics
5.4.1 Currently there is no national reporting mechanism for SDEC performance metrics. However, metrics are being developed nationally, to be captured on ECDS. The benefits of recording SDEC activity in ECDS is described on the SDEC community of practice FutureNHS page, supported by additional information on the ECDS Forum. This will gather evidence from existing providers using ECDS to inform future policy, and support innovation and the accurate recording of patient activity.
5.5 Technology
5.5.1 The provider will provide appropriate information, management and technology (IM&T) systems to fully support the service requirements. It is the provider’s responsibility to ensure the IM&T systems are maintained and fit for purpose. This means all IM&T related infrastructure, computer hardware, software, networking, training and maintenance necessary to support and ensure effective and secure delivery of the service, management of patient care and contract management.
5.5.2 The provider’s chosen IM&T systems should integrate with emerging standards, for example the BARS (Booking And Referrals Standards), which includes the capability to integrate with other services such as NHS 111 and Directory of Services. Systems for referrals (including direct referrals), future bookings, scheduling, tracking, management and the onward referral of patients for further specialised care provision should be compliant with other IM&T systems across healthcare settings.
6 Interdependencies with other services
6.1 Whole system relationships
6.1.1 SDEC services are part of an integrated model within secondary care and across primary, community, NHS 111 and 999 service providers. The provider should work with other services such as virtual wards and UCRs to ensure that the service is streamlined and collaborative.
6.1.2 The provider should work with colleagues responsible for the provision of care within other urgent care settings such as surgery, NHS 111 and 999 clinicians to:
- establish a positive working relationship with all relevant parties
- engage with local clinical networks appropriate for the delivery of the necessary services
- engage in peer review activities with other SDEC units
- play an active role in ICB urgent care provision
6.1.3 The provider should integrate SDEC services across the ICB footprint to ensure the collaborative co-ordination of urgent care services.
6.1.4 The design of SDEC services should also consider local context and include (but not be limited to):
- reviewing admission policies to confirm all specialties’ agreement on the right team for common presentations
- agreeing the navigation process to get patients to the right team, with an ‘SDEC by default’ approach.
- a demand and capacity exercise to link workforce to demand
- an estates exercise to ensure physical space and equipment do not constrain the delivery of SDEC
- a review of the escalation process to ensure that SDEC is delivered at all times; that is, without being ‘bedded’ to avoid patient flow being compromised
- ensuring business intelligence supports key flow metrics and is available across primary, community, secondary, NHS 111 and 999 service providers
6.2 Diagnostics
6.2.1 Rapid access to diagnostics and point of care testing is an integral pathway for same day services and should support requests/reporting for diagnostics being aligned to the ED turnaround times.
6.3 Virtual wards
6.3.1 Virtual wards (also known as hospital at home) allow patients who would otherwise need to be admitted to hospital to get the acute care they need at home, safely and conveniently. SDEC, UCR and virtual wards should collaborate with each other as part of an alternative to the admission model to avoid duplication.
6.3.2 Clinicians working in SDEC should consider referrals to virtual wards for patients with acute needs who require a higher level of care in an out of hospital settings, and also how patients can be directly referred back from a virtual ward into SDEC services so that patients access the care they need, where they need it, safely and conveniently.
6.3.3 Clinical responsibility for the patient on a virtual ward will transfer to the consultant lead within the hospital or within the community provider delivering the service.
6.4 Integration
6.4.1 Same day models of care should be developed jointly, across organisations. All relevant healthcare providers and SDEC should be considered as the first point of contact for escalation if a patient requires secondary care assessment.
6.4.2 Existing processes and pathways should be reviewed to ensure that SDEC services are routinely considered as a safe alternative to admission for urgent care, to support medical, surgical, gynaecology and other subspecialty areas.
7 Service and quality standards
7.1 Service standards
7.1.1Applicable standards set out in guidance and/or issued by a competent body (for example, Royal Colleges and their constituent societies) should be met:
Royal College of Surgeons England
NHS England National SDEC Programme
Getting it Right First Time (GIRFT)
7.1.2 The provider should agree a range of metrics to monitor service quality including but not limited to:
- >33% 0LoS same day activity
- daily collection of SDEC availability versus when SDEC is bedded overnight
- from July 2024, SDEC activity will be measured as a proportion of ED attendances (exclusions will apply)
- access to diagnostics times should be equal to ED response times, and audited to demonstrate compliance
- referrals to SDEC must be provided for a minimum of 9 hours a day to meet peak demand times and allow patients to be discharged to their usual place of residence on the same day
7.2 Governance
7.2.1 The provider will establish a robust internal clinical governance structure with an identified senior clinical lead. The clinical lead is responsible for assuring the clinical quality of the service and that this is supported by a suite of robust policies and procedures. Ideally, the clinical lead should also be supported by an operational, nursing and information lead for SDEC as well as governance and safeguarding teams.
7.2.2 The provider should ensure that there is a:
- named governance lead with a clinical governance supporting structure
- clinical governance audit programme and processes to monitor clinical standards (this should be linked to the relevant Royal College’s audit toolkit or equivalent so there is a systemic approach to measuring outcomes)
7.2.3 The provider should protect the privacy and dignity of patients at all times, including provision for chaperoning patients if this is requested.
7.2.4 The named clinical lead appointed to the service should provide clinical leadership and is job planned to carry out these duties.
7.2.5 The clinical lead should be an experienced senior clinician who has the authority and responsibility to make decisions relating to the clinical direction of the service.
7.2.6 The clinical lead should engage with and participate in work to develop SDEC in the context of urgent care provision across the ICS, with an understanding of the health needs of the local population and of local healthcare services.
7.2.7 The clinical lead should participate in the development of urgent care provision locally, to fully understand how each component of an integrated urgent care system supports patients to be seen on a same day basis in and out of hospital.
7.3 Serious incidents
7.3.1 The provider should report serious incidents including Never Events in accordance with agreed guidance within the organisation.
7.2.2 The provider should have a system in place to receive national safety alerts and implement them promptly.
7.4 Raising concerns and complaints
7.4.1 The provider should ensure that people who use SDEC services know how they can raise concerns.
7.4.2 The provider should have effective means of monitoring and reviewing incidents, concerns and complaints in accordance with agreed guidance within the organisation.
7.5 Experience of care
7.5.1 The provider should have effective means of receiving and acting on feedback from people who use services, so that patients can support the development of services through co-production.
7.5.2 The provider should ensure that the care environment, staffing levels, disabled access and manual handling provision support the needs of people with physical, mental and learning difficulties in a way that promotes their privacy and dignity.
7.5.3 Providers can use the SDEC improvement framework and quality markers to support embedding positive experience of care in SDEC.
7.6 CQUIN
7.6.1 The provider should apply CQUIN goals to the service where these are applicable on an annual basis.
8 Estate
8.1 The provider should ensure SDEC is delivered from a dedicated environment.
8.2 The provider should ensure SDEC services are co-located or located close to the acute medical and/or surgical units and/or the ED where possible with easy access for ambulance or other transport services.
8.3 Infection prevention and control measures (including COVID-19 pathways) are vital in the design and location of the SDEC areas.
8.4 SDEC Health Building Note 15-02 guides providers on the planning and design of SDEC services.
9 Standards of delivery
The principles underpinning SDEC, and the wider UEC offer, should be designed to best fit local context. This would include, but not be limited to, delivering the minimum requirements within the SAMEDAY strategy and framework for delivery (Appendix 1).
All providers should ensure that SDEC services have:
- reviewed their admission policy, to confirm all specialties’ agreement on the right team for common presentations
- agreed the streaming process to ensure patient are navigated to the right team, with an ‘SDEC first’ approach
- undertaken a demand and capacity exercise to link workforce to demand
- undertaken an estates exercise to ensure physical space and equipment do not constrain the delivery of SDEC
- reviewed the escalation process to ensure that the SDEC is delivered at all times, for example not bedded (in line with the NHS OPEL framework)
- used business intelligence to ensure key flow metrics are monitored across UEC with specific focus on same day activity
9.1 SDEC national standards
9.1.1 The following standards were created with the Society for Acute Medicine (SAM), Royal College of Physicians (RCP) and Getting it Right First Time (GIRFT) Programme. There is no current mechanism to capture these standards nationally, but they should be used when reviewing services.
1. The time spent in the ED or UTC prior to transfer to an SDEC facility should be kept to a minimum. The patient should be transferred within 60 minutes of arriving into the ED or UTC.
2. Activity in SDEC must be protected, including during periods of escalation when the hospital is under pressure. Loss of this activity will likely increase pressure.
3. Waiting times for patients in SDEC should be minimised.
1. Observations contributing to a NEWS2 score (National Early Warning Score version 2 – a system to standardise response to acute illness) should be obtained within 15 minutes of a patient’s arrival.
2. Patients should be seen promptly and within 60 minutes by a clinician who has the capabilities to assess and investigate the patient’s signs and symptoms.
4. A discharge summary should be written and sent within 1 day of the episode of care’s completion. This should detail the investigations undertaken, any new therapies instigated and the follow-up plan.
If there are multiple attendances, then it is mandatory that the primary care team receive regular communication, with the mechanism and content defined locally.
For all attendances it should be clearly communicated when the SDEC episode has been completed and management transferred back to the care team in the community.
5. No patient should stay in the SDEC service longer than 8 hours (unless clinically appropriate).
Non-bedding SDEC
9.2.1 Bedding SDEC services during periods of escalation is associated with reduced SDEC capacity and increased +1LoS.
The organisation’s full capacity protocol should include de-escalation of SDEC within 2 hours of resumption of normal operating hours following periods of escalation, to restore flow across urgent care in line with the NHS OPEL framework.
9.2.2 Download Appendix 1: Self-assessment tool: Opportunities for improvement
Publication reference: PR00824

