Introduction
This improvement guide is one in a series designed to support you to deliver clinical and operational improvement. It sets out the evidence for the most impactful interventions that can create greater value for patients and more productive services.
It provides a range of change ideas, and we encourage teams, organisations and systems to consider testing, adapting and building on them for their local context and local improvement work. This should be led by those closest to the point of care, supported by senior sponsorship, and applying rigorous improvement methods to test, learn and adapt rapidly.
We want to understand how this guide works for you and your teams, and how we can further develop and improve it to make it as useful as possible to support local improvement programmes. Therefore, this is an interim guide – our intention is it will be refined, developed and updated as we learn what works through your teams. Please share your thoughts on the guide and your ideas to include in it – details on how to do this are at the end of this guide.
This guide focuses on all-age solutions. Links will take you, where appropriate, to age group and condition specific guidance.
To complement this guide, an improvement analytics compartment for theatres and perioperative care has been launched in the Model Health System, which brings into one place the tracking indicators referenced in this guide for ease of access. The indicators cover a range of process, outcome and quality metrics that trusts and systems can use to track their progress in implementing the change ideas in this guide. Many are presented using statistical process control (SPC) charts to help you easily see where improvements are being made.
The ‘theatre productivity’ multidisciplinary team
Actions before and after the actual surgery in theatres will impact on theatre productivity. Inefficiencies already identified pre-Covid were amplified during the pandemic. Ensuring hospitals reset their surgical pathways and processes, while maintaining capacity to teach and train, is vital to improve theatre productivity and efficiency. It will enable more efficient use of the sessions we can currently staff and run and will provide a firm base on which to increase our estate usage.
Improvements to theatre productivity require a full team effort and should not be seen as the sole responsibility of theatres. Input and action are required across the surgical and perioperative pathways and providers should ensure this work is taken forward by relevant teams working collaboratively and in an aligned way with dedicated clinical ownership and executive support. Improving productivity means delivering as much clinical value for patients as possible with the resources we have, while maintaining safety and improving staff engagement and morale. A whole provider approach is needed with all clinical, operational and theatre teams considering how the elements within their control contribute to the overall value of surgical services and care. For example:
- the effectiveness of current processes in ensuring patients are on the right surgical pathways for their care, and moving procedures down the gradient of care as appropriate (moving from admissions to day case procedures)
- the effectiveness of preoperative processes in ensuring patients are well prepared and ready for surgery (reducing cancellations and improving outcomes)
- the efficiency of intraoperative processes in theatres and what the variation is between specialties and individual teams within the specialty
- the effectiveness of postoperative processes to aid recovery, improve outcomes and reduce length of stay
Providers should already have named clinical, operational and executive senior responsible officers for theatre productivity who report to the board, and we would expect them to engage relevant stakeholders in this work.
Teams that will need to be involved to ensure sustainable change is made are likely to include:
- surgical specialty management teams
- booking teams
- preoperative assessment
- therapies
- surgeons
- anaesthetists
- theatres
- ward staffing
- critical care/enhanced care
- surgical specialty nursing and allied health professionals
- sterile services
- portering and estates
Each team will need access to local data to evaluate their successes and identify areas where they can realise improvement.
Overarching ambition
This diagram sets out the elements needed to deliver greatest value from surgical procedures and processes.
Improving theatre and surgery productivity 24/25 – driver diagrams

Measures

When considering how to approach this, the actions you need to prioritise are to:
- Understand the data and variation to identify opportunities.
- Review and address the operational process issues and opportunities highlighted in the data.
- Consider intraoperative and clinical transformation opportunities (change ideas) including moving procedures down the gradient of care settings.
The importance of data
Using local data and intelligence to identify improvement opportunities
It is vital that hospitals have well-developed systems to capture relevant data and monitor key metrics associated with delivering surgery efficiently and effectively. Many of these metrics are already available and it is important that hospitals:
- submit complete and accurate data to national datasets (such as the theatres dataset)
- build Model Health System metrics into business-as-usual monitoring processes for clinical specialty and theatre teams
- use local data and insights to drive continuous improvement
Data resources
National improvement analytics data
Providers can use the in the Model Health System to ensure they have a clear picture of data and trends compared with peers:
- theatre metrics compartment
- theatre data quality dashboard (to monitor and support improved quality of theatre data)
- British Association of Day Surgery metrics (this compartment will soon include outpatient procedures as well as daycase procedures)
- high volume, low complexity
- surgical length of stay metrics; available for key procedures in GIRFT specialty compartments, for example, for primary hip replacement (12 months to quarter end)
Internal hospital data:
- utilisation of theatre estate (metrics will soon be available within the theatres compartment of the Model Health System)
- surgical cancellation rates (metrics will soon be available within the theatres compartment of the Model Health System)
- surgical length of stay (length of stay metrics for key procedures are available in the GIRFT specialty compartments of the Model Health System)
- the GIRFT SPaedIT dashboard brings together provider-level data for paediatric surgical specialties summarising demand, capacity, flow and outcomes in one place
Identifying trends
The rich data theatres generate (including the qualitative data from theatre debriefs) should be used to identify opportunities to improve efficiency and productivity. However, unless trends are identified in the data, there is a risk that events – for example, cancellations and late starts – are reviewed in isolation, preventing operational and clinical teams from identifying the key areas where changes could be made or what will need to be monitored to measure the impact of changes in process or pathways. Hospitals should ensure areas such as reason for cancellation are monitored over time to identify their impact on productivity.
Taking a whole pathway approach
High-level metrics such as capped theatre touchtime (the time the theatre team was actively hands-on with patients) are influenced by factors at all stages of the theatre pathway and solutions are not always within the gift of theatre or clinical teams. Using a collection of metrics will help you identify the barriers to increased productivity, such as booked versus actual utilisation and reason for cancellation.
Improving data ownership
To support continuous improvement, clinical and operational teams should own the data; this includes data being visible and, where practical, signed off by teams. As an example, clinical teams should, as part of theatre sign out and debrief, agree the surgical timestamps and wider data entered into the theatre system. This will provide confidence in using data to inform discussions on improvement opportunities.
Efficiency: optimising pre-admission processes
Optimising theatre efficiency and maximising activity
The GIRFT operational modules help hospitals get more value from theatre time. The 6 modules (available on the GIRFT FutureNHS platform) span the theatres pathway and set out the key elements of what a good service should look like:
- Module 1: Theatre booking
- Module 2: Theatre waiting list management and list allocation
- Module 3: Theatre scheduling
- Module 4: Patient preparation and effective theatre flow
- Module 5: Surgical discharge
- Module 6: Workforce: Workforce planning and deployment
The Anaesthetics and perioperative medicine (APOM) and theatres and other specialty ‘further faster’ handbooks also provide resources.
Early risk stratification and patient optimisation
Well managed, standardised pre-admission processes are critical to delivering smooth pathways for patients, improving both experience and outcomes and helping to avoid unnecessary cancellations by ensuring patients are prepared and ready for surgery when they are listed.
Early screening is vital in preoperative patient management to enable efficient surgical pathways.
Risk stratification/triage happens before preoperative assessment and can identify a need to optimise a patient’s health with respect to various co-morbidities. This work reduces postoperative morbidity, leading to shorter length of stay, and fewer readmissions, cancellations and admissions to critical care. It also supports a shift to daycase surgery and improves health outcomes and quality of life – particularly in deprived populations and for patients with long-term conditions.
Important principles to follow for early screening and risk stratification include:
- patients are screened for perioperative risk factors as early as possible in their pathway. This should be as soon as surgery is being considered and, at the latest, as soon as possible after the patient has been added to the waiting list. Digital tools can be particularly helpful at this early screening stage
- patients identified through a screening assessment as having risk factors for poor perioperative or surgical outcomes (for example, diabetes, anaemia, obesity) receive proactive, personalised support to optimise their health before surgery or, if it becomes clear during screening that surgery may not be in a patient’s best interests, they should be signposted for shared decision-making
- patients waiting for inpatient procedures are contacted by their hospital at least every 3 months to check they still require the procedure and their health status has not changed
Patients waiting for inpatient procedures should only be given a date to come in for surgery after being confirmed as fit and ready for surgery. When a patient requires further optimisation, a senior clinical decision-maker determines whether they should remain on the admitted waiting list while this happens, mindful of the time required for optimisation and local waiting times – for example, if optimisation is expected to take 2 months but the waiting list is 6 months, it would not be in the patient’s interest to remove them from the waiting list as they would wait considerably longer.
Maximising patient fitness for surgery and effective preoperative planning will reduce the need to admit the patient as an inpatient for procedures that can be undertaken as a daycase.
Preoperative optimisation should also reduce the need for a postoperative critical care or enhanced care bed, either planned (because the patient is high risk) or unplanned (because the patient has incurred a complication).
Preoperative assessment
Patients undergoing inpatient surgery should be admitted on the morning of the procedure, unless there is an absolute clinical indication for earlier admission. Improving day of surgery admission rates will release inpatient capacity.
Hospitals should evaluate their enhanced and critical care capacity to ensure lack of access to a higher acuity bed is not a reason for last minute cancellations. Follow this guidance for establishing and delivering enhanced care services.
Preoperative assessment (POA) teams play a vital role in the perioperative care pathway by ensuring patients are ready for surgery and providing surgical teams with information about patient co-morbidities and risk factors so these can be managed in theatre with appropriate prevention and recovery strategies.
Effective POA ensures:
- patients are not offered ‘to come in’ dates until passed fit at POA. This reduces cancellations and improves patient experience
- more effective and predictable scheduling of theatre time
- less likelihood of complications
- faster recovery as patients are optimised for surgery, giving both better outcomes and increased productivity
Detailed guidance on POA is in the APOM Further Faster handbook.
Suppliers provide a range of digital tools to enhance and streamline the preoperative pathway for patients. These can contribute to productivity if they are implemented well, but this must be planned effectively, including how a tool integrates with existing systems. However, the most important principle before considering implementing a digital solution is to check the pathway is correct. Read the guide to digital preoperative assessment tools on FutureNHS.
Minimising avoidable cancellations
Cancellations are a major source of lost value in theatre pathways and are mostly avoidable. Patients must be well-informed, well-prepared and have been involved in the decision-making process for surgery – this reduces cancellations. It is the responsibility of every healthcare professional (HCP) involved in perioperative care to make every contact count by confirming that patients have the right information and clear expectations around their admission for surgery and discharge.
Ensuring effective selection and preparation of patients by applying the preoperative processes described above will minimise patient-related cancellations and avoidable postponements.
Other things that can avoid cancellations are:
- regular review (3 monthly) of the patient up to the point of admission
- contact with the patient 3 to 5 days before admission to confirm attendance
- patients given clear information and guidance on what to expect and the appointments they need to attend, and the opportunity to ask any questions. Information should be inclusive, accessible and centred on their individual needs
- clear patient information on what to expect before, during and after their procedure, including practical information such as where they will have their surgery and how to get there, parking, contact numbers, facilities, visiting policies and requirements for being accompanied home
It is also important to understand where weaknesses in current processes mean services cancel surgeries such as:
- bed availability (including critical care) and discharge processes. Consider whether ‘criteria to reside’ are being monitored and applied
- equipment availability
- late start times and over-runs
- not having the right staff skill mix for the procedures listed
Sessions may need to be changed as required but many of these issues can be avoided by improving operational and intraoperative management.
Mitigating the impact of cancellations is also important, particularly while improving processes. It helps to have a late cancellation standard operating procedure and to maintain a list of standby patients who can fill gaps in theatre lists at short notice.
Effective theatre scheduling and preparation
Effective theatre scheduling
Efficient booking practices are pivotal for maximising theatre utilisation. Inefficiently managed booking will significantly hamper productivity. Detailed guidance is provided in the GIRFT theatres scheduling practical guides.
Theatre preparation
Having clear, standardised processes to manage theatre preparation should reduce late starts; timely starts sets things up for a productive day. Processes should be in place to ensure theatre teams replenish stocks at the end of each day, ready for the next day (including drugs and fluids).
Following theatre cleaning, night teams should use the equipment prepared by the day shift and the individual anaesthetic and surgeon preference cards to set up equipment for the next day’s identified golden patient. For teams without a night shift, all the equipment should be ready for the day shift to bring into the clean theatre at the start of the next day shift.
Prepared instrumentation and equipment should be re-confirmed in the morning, before any team brief including, for example (not exhaustive), instrumentation by case; equipment, including operating table; positioning aids; anaesthetic equipment (to include block equipment/trolley/pumps); fluids and drugs.
Tracking indicators
In addition to local indicators linked to your change ideas for optimising pre-admission processes, the theatres improvement analytics within the Model Health System include metrics so you can benchmark yourself against peers and track your improvement.
We are developing a surgical cancellations metric and this will be available later in 2024/25 in this compartment.
Resources
- guide for early screening, risk assessment and optimisation for adult patients
- GIRFT operational implementation and support guide for early screening, risk assessment and optimisation for adult patients
- GIRFT practical tips on how to build a pool of patients
- GIRFT theatre scheduling practical guide
- GIRFT patient preparation and effective theatre flow
- digital preoperative assessment tools
- professional guidance (CPOC/FICM) on establishing and delivering enhanced perioperative care services
- implementation guidance for enhanced perioperative care
Efficiency: Optimising intraoperative processes and flow
Effective theatre flows
Designing effective theatre flows is complicated as multiple clinical, operational and administrative teams are involved across many related processes. When these work together effectively, we can deliver the most value for patients.
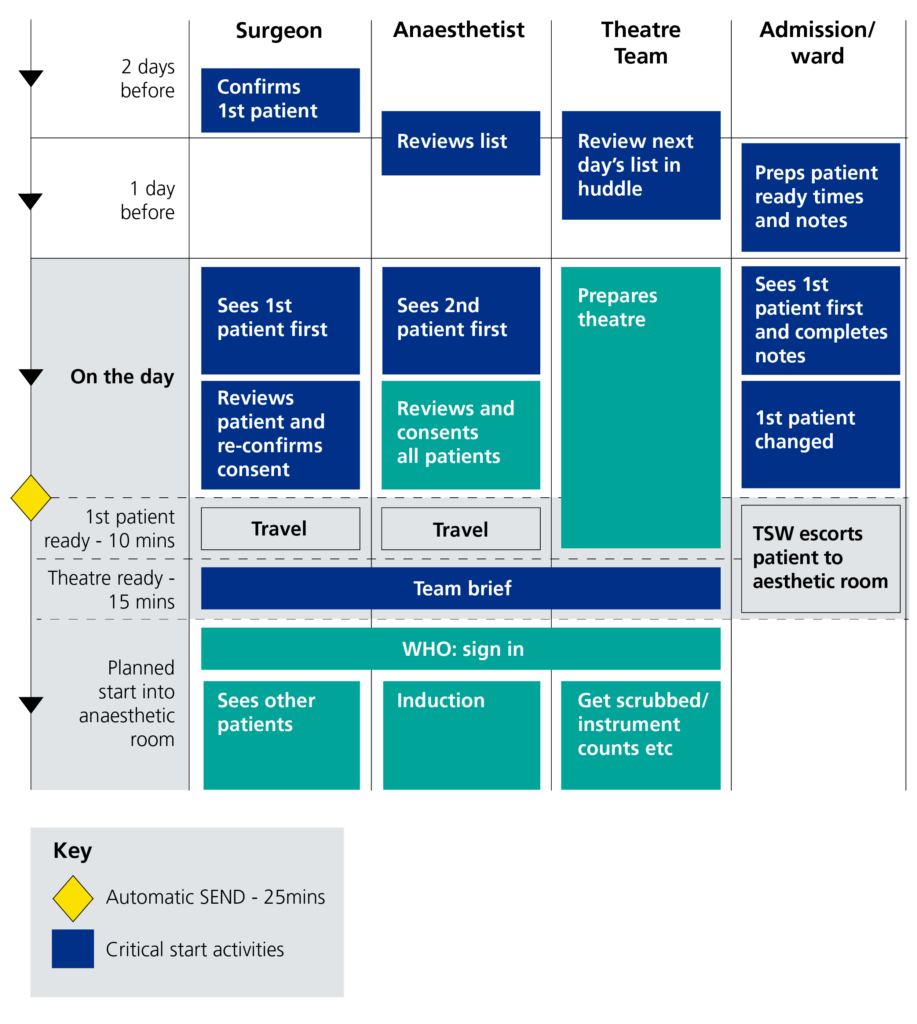
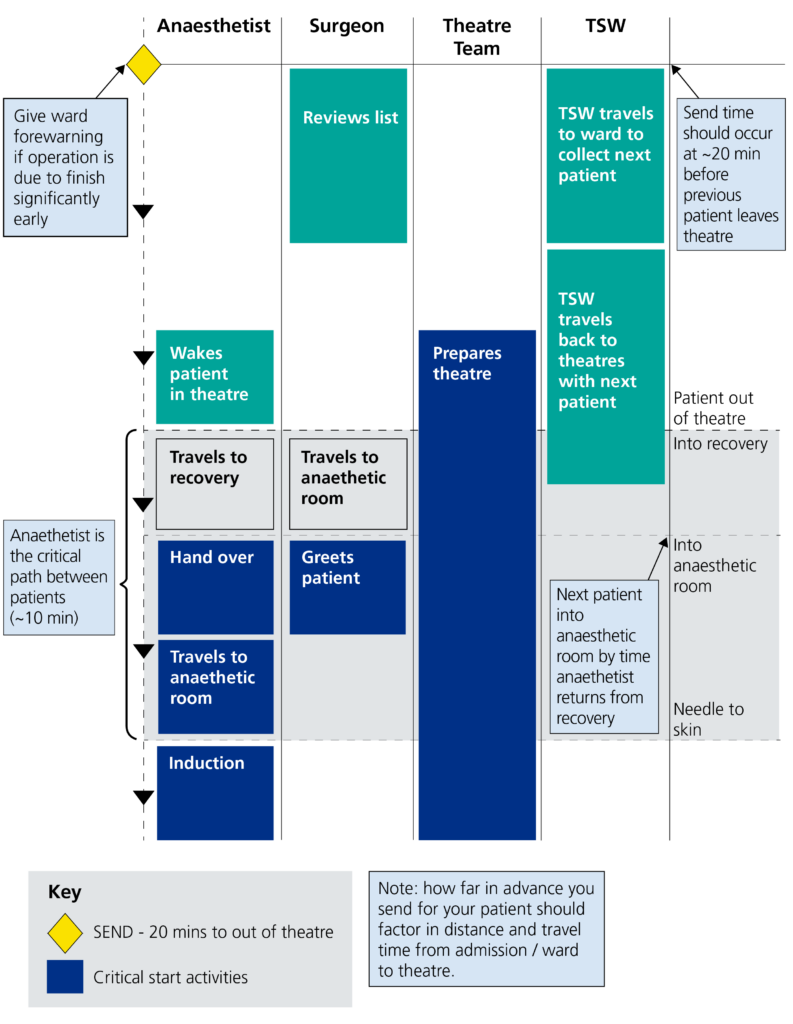
Appendices 1 (patient journey – the refined start process) and 2 (patient journey – turnaround process) provide examples of how effective flows can improve the patient’s journey on the day of surgery, while delivering more value and reducing over-runs and cancellations. Hospitals should develop similar clear process flows (specific to their service) to understand where improvements can be made.
A selection of the case studies on the GIRFT FutureNHS workspace that focus on improving flows and increasing daycase rates is:
- Sheffield Children’s Hospital NHS Foundation Trust ENT rapid lists
- Croydon Trust increases elective cholecystectomy daycase rates
- physiotherapy approaches to support daycase arthroplasty at South West Orthopaedic Hub
- optimising the general surgery pathways at Trafford Elective Hub
- Newcastle Hospitals NHS Foundation Trust improving daycase rates in gynaecology
- introducing daycase hysterectomy at University Hospitals Sussex
- introducing high flow lists to achieve the GIRFT standard of 8 cataracts per list
- faster turnover cataract pathway at Nottingham University Hospitals
Effective communication
Optimising theatre flows to deliver the most value for patients hinges on the effectiveness of the whole team. Appropriate systems should be in place to support co-ordinating theatres ensuring that everyone involved is well informed about all patients, procedures, equipment requirements and planned timings. The team leader for the day should be identified and the roles within the team must be clearly defined.
Huddles and team briefings are helpful in keeping all staff informed before starting lists including, for example, to provide or discuss:
- introductions
- overview of the list
- individual cases
- patient specific concerns, for example, diabetes, anticoagulants, allergies, learning difficulties or capability concerns
- surgical plan (including positioning) and specific meds, for example, antibiotics, anticoagulants
- anaesthetic plan
- confirmation of list order
- planned bed status postoperatively
- staffing requirement and issues
- educational and training needs
Intraoperative process optimisation
Efficient, process-driven management of operating theatres is paramount for optimal productivity. An efficient start to the day of surgery from the time the patient arrives is essential for a smooth patient experience for both day patients and inpatients. The GIRFT theatre productivity programme practical guide module 4: patient preparation and effective theatre flow offers advice on streamlining operations within the surgical environment.
Some key principles are:
- a dedicated day surgery area is used whenever possible, and patients remain in the waiting area until they need to change for theatre
- consultation rooms are available for preoperative review by the surgical and anaesthetic team
- the theatre’s operational policy sets clear expectations for key daily milestones, for example, patient arrival times to the hospital on the day of surgery, list start and finish times, golden patient arrival time to theatre
- instrumentation and equipment are confirmed for the golden patient before the team briefing and ward staff send the golden patient at the time stated in the operational policy
- staff work in parallel not in sequence to minimise turnover over times, for example, anaesthetic and scrub staff prepare for the next patient while the current patient’s procedure is ending and the next patient is being sent for
- lists run continuously without interruptions, for example due to missing equipment. Staff are supported to have breaks, and these are scheduled during turnover to avoid interruptions, and communicated at the team brief
Minimising turnaround time
Preparation for next patient
During the current procedure, the anaesthetic practitioner should prepare the anaesthetic room for the next patient. In theatres with a functioning set up room, the scrub team can start to prepare kit for the next patient. If there is no set up room, and a case needs a lot of equipment, for greatest efficiency the scrub team can double scrub for the set-up phase.
Sending for the next patient
The precise timing of sending for the next patient will depend on the patient pathway / hospital estate team make up but should always be before sign out and allow time for transfer and preoperative checks. This will ensure the next patient is in the anaesthetic room as their predecessor is leaving the theatre. Patient experience needs to be considered alongside productivity if the patient is being admitted directly to the anaesthetic room so they are not waiting in excess of 5 to 10 minutes. Theatre teams should monitor waits as a quality indicator.
Auto-send
An auto-send process should be embedded to give theatre and surgical teams the confidence to start the theatre list without waiting for postoperative bed confirmation. This process is essential to support lists with complex cases, and any concerns regarding intensive care / high dependency unit capacity that could affect it should be highlighted and discussed in the forward look huddle the day before.
Starting on time
Patient admission times should correspond with theatre start times, and this should mean the admission team can admit the first patient ahead of the surgical and anaesthetic teams arriving to review the patients.
Departmental huddles should be timed so list start times aren’t delayed, and patients should be transferred into the anaesthetic room/theatre after the team brief, in time for the theatre session start time.
Tracking indicators
In addition to local indicators linked to your change ideas for optimising intraoperative processes, the theatres improvement analytics within the Model Health System include a range of measures for you to benchmark yourself against peers and track your improvement.
Resources
- GIRFT theatre training: theatre booking module
- national safety standards for invasive procedures
- GIRFT national day surgery delivery pack
- NICE Quality Standard 138 Tranexamic acid for adults
- NHS Blood and Transplant blood transfusion audit
- Bilku et al (2014) Role of preoperative carbohydrate loading: a systematic review
- Perioperative Quality Improvement Programme (PQIP) report 4
Reducing acuity of care
Minimising the amount of time patients need to stay postoperatively and ensuring the optimal setting for their care
Right pathway initiatives
Productive surgical pathways start by ensuring the patient is on the right pathway for their needs. This means moving the procedures as far down the gradient of care as possible, maximising delivery as daycase and outpatient procedures where appropriate.
It is still practice in many hospitals to deliver certain procedures in an inpatient setting despite clear evidence that daycase surgery provides similar or better outcomes. Focusing on ‘daycase by default’ and taking this further by moving daycases into outpatient procedure settings, where appropriate, can deliver significant productivity gains, while reducing the amount of resource required to deliver care and providing a better experience for patients.
Resources for identifying appropriate shifts from inpatient to daycase surgery and daycase to outpatient procedures are in the Right Procedure, Right Place workspace.
Right Procedure, Right Place
The Right Procedure, Right Place (RPRP) initiative is about optimising theatre staffing resources for a specific group of elective procedures carried out under local anaesthetic (Right Procedure) that with a different staffing template can be safely and effectively delivered outside a theatre environment (Right Place).
This can enable hospitals to:
- increase throughput for high volume, low complexity local anaesthetic procedures
- reduce the number of long waiters for the defined list of procedures
- reduce the number of cancelled lists due to theatre staffing
- improve theatre staff retention and morale
- improve patient satisfaction
- develop an approach that is scalable at trust / system / regional level
GIRFT surgical pathways
The Getting it Right First Time (GIRFT) programme has developed numerous surgical pathways that offer hospitals a blueprint for delivering effective and efficient care. In addition, specialty and procedure specific guides on increasing daycases and shifting care to outpatient procedure settings are available – see resources below.
Elective hubs
There has been considerable investment in elective hubs over the last 2 years and most hospitals now have access to dedicated, ring-fenced resources for elective surgery that are often shared across systems.
It is vital that local systems understand and regularly review the use of this capacity, both in terms of the pathways and procedures delivered and the overall efficiency of hub utilisation.
The most productive elective hubs are those that rigorously enforce the ring-fencing of their facilities and workforce, and invest in dedicated operational management capacity to ensure effective referral pathways into the hub and efficient patient flow management.
Tracking indicators
In addition to local indicators linked to your change ideas for reducing the acuity of care, the theatres improvement analytics in the Model Health System include the following measures for you to benchmark yourself against peers and track your improvement:
- British Association of Day Surgery metrics (this compartment will soon include outpatient procedures as well as daycase procedures)
- high volume, low complexity procedures
Case studies
- Right Procedure, Right Place
- Southwest Ambulatory Orthopaedic Centre ambulatory hip and knee replacements operational pathway (video)
- optimising the general surgery pathways at Trafford Elective Hub
- supporting hospitals through system working: Sulis Hospital
- using orthopaedic consultant rotation to increase utilisation of elective hub
Resources
- Right Procedure, Right Place
- GIRFT pathways
- GIRFT national day surgery delivery pack
- GIRFT daycase paediatric tonsillectomy analysis
- GIRFT/SWLEOC surgical hub toolkit
- GIRFT surgical pathway guides can be found on these relevant specialty links
Optimising postoperative and discharge processes
Timely, criteria-driven postoperative care is an essential element for successful delivery of daycase pathways and reducing length of stay for inpatients.
The GIRFT day surgery delivery pack provides guidance on postoperative care in the day case pathway, and the PQIP and NHS England are promoting the Drinking, Eating and Mobilising (DrEaMing) care bundle.
Key principles for effective postoperative care include:
- daycase patients who have received spinal or reginal anaesthesia should be able to quickly transit through recovery
- daycase patients are discharged when they meet the discharge criteria rather than after a minimum time period. This includes those daycase patients requiring 1:1 nursing care in recovery
- there is an agreed process for the admission to a hospital bed of patients deemed unsafe to discharge, and the need for admission is regularly reviewed
- the hospital provides nurse-led follow-up to offer patients advice after discharge or, if they were not discharged on the day of surgery, to review the benefit of their overnight stay
- 80% of surgical inpatients are supported to drink, eat and mobilise within 24 hours of surgery ending, unless all or some of the DrEaMing care bundle is contraindicated for a procedure (see legacy 2023/24 coding guidance)
Patient preparation
The elements of preoperative preparation and care outlined earlier are equally important for enabling effective postoperative care and early discharge; they set patient expectations for length of stay.
Enhanced recovery and DrEaMing
Enhanced care (level 1) provides a higher acuity environment for patients at high risk of postoperative complications and is tailored to the needs of surgical patients on recovery pathways as opposed to deteriorating patients at risk of organ failure (for whom care should be provided in level 2 or 3 critical care settings). Enhanced care can provide a more holistic recovery environment for higher risk surgical patients and reduce the demand on level 2 and 3 services, while also reducing the risk of surgical cancellation or postoperative complications and therefore increased cost and postoperative length of stay.
Traditional specialty-specific pathways have many elements that are complex to implement and are challenging to monitor. A simplified care bundle approach to enhanced recovery for all surgical specialties – DrEaMing – has been an NHS England CQUIN since April 2022. This incentivises hospitals to support patients to achieve the following within 24 hours of surgery ending:
- drinking – free fluids
- eating – soft diet (enteral feeding major H&N and upper GI)
- mobilising – bed to chair (exclusions: sedated, spinal fluid leak, spinal cord injury; airway concerns)
- evidence from the PQIP report 4 shows that hospitals with high compliance of DrEaMing within 24 hours of surgery ending (>80%) have a length of stay 2 days shorter than those with lower compliance
Criteria-led discharge
Criteria-led discharge releases capacity with more streamlined patient discharge. It empowers registered HCPs to discharge patients against agreed clinical criteria while enhancing the safety of patient discharge, through robust and audited processes. Evidence suggests that discharge can be achieved earlier in the day when using criteria-led discharge, which in turn improves patient experience.
Discharge lounge
Organisations should use a discharge lounge for patients who are fit and waiting to leave the hospital on that day. This allows the early preparation of inpatient elective activity and prevents theatre delays due to the unavailability of beds.
Tracking indicators
In addition to local indicators linked to your change ideas for optimising postoperative and discharge processes, the national improvement analytics for theatres include:
- British Association of Day Surgery metrics in the Model Health System
- surgical length of stay metrics in the GIRFT specialty compartments in the Model Health System, for example, length of stay for primary hip replacement
Resources
- GIRFT theatre training: surgical discharge
- DrEaMing CQUIN for 2023/24 to ensure more patients drink, eat and mobilise within 24 hrs of surgery
- Oliver et al (2022) Delivery of drinking, eating and mobilising (DrEaMing) and its association with length of hospital stay after major noncardiac surgery: observational cohort study
- Professional guidance (CPOC/FICM) on establishing and delivering enhanced perioperative care services
- Implementation guidance for enhanced perioperative care
- South Warwickshire programme for enhancing recovery following hip and knee arthroplasty
- Lancashire NHS Trust reduces average length of stay in elective arthroplasty through enhancing recovery
- Discharge lounge standard operating procedure
Right people
Utilising your workforce more effectively through high quality operational workforce planning and deployment will help improve staff experience and retention, support service improvement and further improve productivity by optimising the skills and capacity of your workforce.
Optimising the valuable skills and capacity of clinical workforces
Good quality workforce planning and deployment is about optimising the valuable skills and capacity of our clinical workforce by ensuring the right people are in the right place at the right time to deliver high quality, efficient patient care. It is about supporting the development of staff and services and providing the visibility of clinical capacity required to plan services effectively and match valuable clinical capacity to patient need.
Improvement requires targeted action on workforce planning and transformation; workforce deployment; and governance and measurement.
Follow the resources on clinical workforce productivity on FutureNHS. In particular, we recommend the following resources for each of the 3 pillars of excellence, which are workforce planning and deployment; workforce transformation; and governance and measurement.
Workforce planning and deployment
Workforce planning and deployment resources
- e-job planning and e-rostering for effective planning and deployment of all staff:
- the Advancing levels of attainment handbook and related resources: helps organisations establish what their e-rostering and e-job planning levels of attainment are and what is required at each level to progress, based on local need and current position
- the e-job planning toolkit and e-rostering toolkit: provide a step-by-step guide to optimising system usage and embedding effective associated processes and governance
- e-rostering as an enabler to flexible working: provides resources to support team leaders working in clinical areas to develop ways to roster their staff more flexibly, thereby improving work-life balance and experience at work for staff. The case studies showcase the innovative initiatives that are being implemented and their impacts on staff wellbeing and retention
- medical consultant job planning improvement guide
- Demand and capacity planning: provides resources to support service and system-level demand and capacity planning, including modelling tools and approaches, case studies, webinars and e-learning
- Digital staff passport: enables NHS employees to use their smart phone to share employment, education and training, and occupational health details with hospitals 24/7, to support their moves between those hospitals
- Agency toolkit: supports organisations to reduce their agency staff bills and encourage workers back into substantive and bank roles
Retention resources
- Improving staff retention guide: supports line managers and employers to consider the key areas that affect workforce retention
- International retention toolkit: actions employers can take, such as mapping skillset and qualifications and setting up pastoral support, to ensure internationally recruited staff will want to stay, thrive and build lasting careers in the NHS
- NHS Emeritus: an initiative that connects recently retired and peri-retired clinicians across England with NHS providers of acute care who need the help only experienced clinicians can offer
Workforce transformation
Workforce transformation resources
- Clinically-Led Workforce and Activity Redesign (CLEAR) programme: supports clinicians and organisations to deliver transformation and workforce redesign projects to enhance patient care by equipping frontline staff with skills in data analysis, innovation and leadership
- Star: accelerating workforce redesign: a model and workshop for workforce transformation, enabling you to explore workforce challenges, develop bespoke action plans and use resources in the Star online directory
- Roles explorer: provides resources for workforce redesign, such as introducing new roles or innovative adaptations to existing roles within a service or system
- Calderdale Framework: an evidence-based workforce transformation tool used in acute and community settings to rapidly identify skill sets required by services and their populations in acute, sub-acute and rehabilitation phases
- workforce transformation case studies: an interactive map of good workforce transformation practice, including examples from theatres
Governance and measurement
Governance resources
- National Quality Board (NQB): safe sustainable and productive staffing guidance (2016): an improvement resource that builds on the NQB’s 2013 expectations and framework, within which organisations and staff should make decisions about staffing that optimise productivity and efficiency while maintaining focus on improving quality
- e-rostering and e-job planning meaningful use standards: support hospitals to implement and use e-job planning and e-rostering software to its full potential, which includes the use of board reporting and metrics for improvement
Measurement resources
- Care hours per patient day: guidance on the principal measure of nursing, midwifery and healthcare support staff deployment on inpatient wards
- Model Health System: data-driven improvement tool that enables NHS health systems and hospitals to benchmark quality and productivity
- Workforce Productivity Diagnostic Tool: supporting systems and hospitals to understand and benchmark their workforce productivity
Change ideas
Collect workforce data to understand your workforce capacity:
- capture and review data for all staff who work in theatres on a permanent or temporary basis. Include data from / on ESR, temporary spend, recharge, recruitment and retention rates, turnover, sickness absence, age profile and demographics
- review your consultant-level capacity (including direct clinical care and supporting professional activity time)
Understand your retrospective and prospective activity:
- collect activity data and review any service plans that may impact on future activity levels (such as work transferring from location or changes in mode of delivery)
- this review should include key hours of operation
Undertake a systematic review of your workforce requirements:
- map your pathway and consider which staff are required at each stage
- review the roles, skills and capacity required to meet your expected activity. Consider whether any new roles are required or would improve productivity
- review your pay spend run rates and compare these to your budget
- consider recruitment, training and retention needs, including specific equipment/ specialty training requirements
Review national policy when building your establishment and optimising deployment:
- Developing workforce safeguards: Supporting providers to deliver high quality care through safe and effective staffing
- GIRFT guidance
- appropriate Royal College guidance
Please share your ideas and feedback with us
Thank you for engaging with this guide. While we have collected a wide range of improvement ideas, we want to gather your local improvement ideas for inclusion in an updated version of this guide early in 2025.
Please share your ideas and feedback with us. There are 2 ways you can do this:
- by emailing us at england.clinops@nhs.net
- by feeding back through your local Learning and Improvement Network. Details on the networks are on the FutureNHS platform
Appendix 1: Patient journey – the refined start process
Appendix 2: Patient journey – turnaround process
Publication reference: PRN01435_ii (interim version)

