Introduction
This urgent and emergency care (UEC) acute patient flow clinical and operational improvement guide provides a range of change ideas for how UEC services can improve both patient care and productivity, with the 2 principal aims of:
- making care safer and patient experience better by increasing the adoption of evidenced best practice
- maximising the value of patients’ and clinicians’ time and the productivity of services by tackling waste and addressing inefficient processes
We know, for example, that patients who stay in the emergency department (ED) for more than 6 hours have a higher risk of dying within 30 days. A length of stay (LoS) of 10 days or more results in serious deconditioning and loss of muscle mass. With more than 1 in 10 patients in 2023/24 staying in ED for longer than 12 hours, and 20% of G&A beds consistently occupied by patients with a 21+ days LoS, improving flow is critical to improving the quality and safety of care.
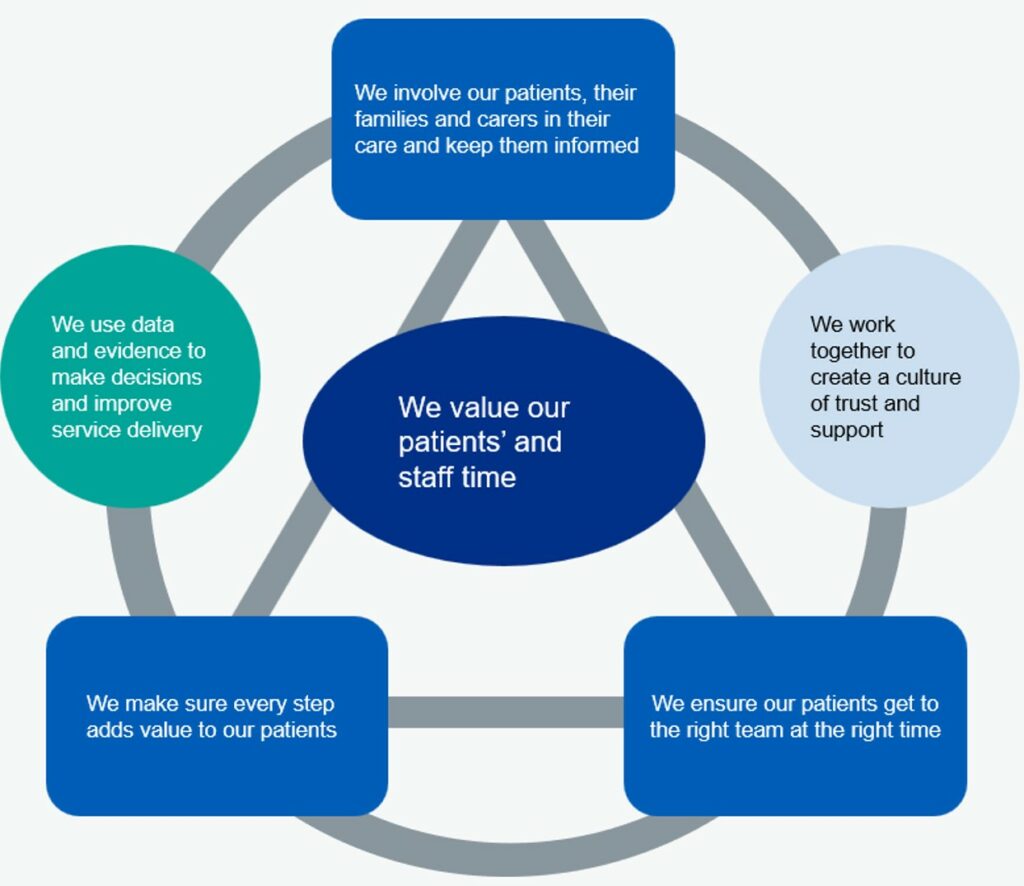
The improvement ideas in this guide are intended to be supportive, particularly for winter planning. Those closest to delivering care should be supported with senior sponsorship to apply improvement methods to test, adapt and build on the ideas for your local context. Ensuring improvement work uses the 5 universal flow principles as the basis for making changes will help gain traction with teams and provide a framework through which to capture hearts and minds in this important work.
This guide is part of a suite of tools and interventions that will be released over the coming months to support clinical and operational teams. In particular, the improvement analytics tool in the Model Health System will bring together the tracking indicators referenced in this guide. These indicators cover a range of process, outcome and quality metrics that trusts and systems can use to diagnose issues, identify opportunities to improve care and to track improvement over time. The improvement analytics tool also includes dashboards to help you see how improvements are being realised over time and how you compare to others.
We want to understand how this guide works for you and your teams, and how we can further develop and improve it to make it as useful as possible to support local improvement programmes. Therefore, this is an interim guide – our intention is it will be refined, developed and updated as we learn what works through your teams. Please share your thoughts on the guide and your ideas to include in it – details on how to do this are at the end of this guide.
UEC flow driver diagrams


Right place
How to ensure patients are cared for in the most appropriate setting for their needs: identify those patients who may not need to be admitted
Criteria to admit
The criteria to admit (CTA) decision support tool is an algorithm that clinicians can use in real-time to check or assess whether a patient needs to be admitted, and to identify potential alternatives. Admission is highly likely if the response to any of the questions the algorithm asks is ‘yes’.
The tool cannot replace or override the senior clinician’s decision to admit and should not be used unless the multidisciplinary team (MDT) is considering a patient admission.
Consistent use of the CTA decision support tool can help identify those patients who will not benefit from admission and identify suitable alternatives. It minimises variation in decisions to admit and helps ensure only patients who need acute hospital beds are admitted and therefore reduces delays and waste.
The tool can also be used retrospectively as an audit tool to determine:
- bed days utilisation
- number of bed days that would have been saved, if the tool was used at the point of attendance
- gaps in service provision
Optimise admissions
If you optimise admissions, you can improve flow and clinical outcomes by reducing:
- length of stay
- bed occupancy
- the number of non-elective (NEL) admissions
Change ideas
- Establish CTA as a real-time tool for confirming patient admissions.
- Ensure senior decision-makers use CTA early in the patient journey, ideally at the point of attendance.
- Establish team job plans to support the early review of all patients by a senior decision-maker.
- Extend CTA to resident doctors and other healthcare professionals with senior decision-maker oversight.
- Use CTA audits to establish the right capacity to meet the demand for alternatives to admission.
- Review CTA for admitted patients after 24 hours to determine whether patients are fit for discharge.
Tracking indicators
In addition to local process measures linked to your change ideas, the improvement analytics in the Model Health System include the following measures:
- proportion of patients admitted with a record of a decision to admit review (data should be locally collected and audited)
- conversion rate from ED attendance to NEL admission
Systems should review the implications of overcrowded EDs and, first and foremost, the impact on patients of being cared for in corridors when there is no bed for them. They should also review the additional costs incurred, particularly bank and agency spend.
Resources
- Emergency Care Improvement Support Team (ECIST) resources on criteria to admit
- criteria to admit flow chart
- ECIST bitesize podcast series on criteria to admit
- criteria to admit audit tool and user guide
Alternatives to admission
Alternatives to a NEL admission should include:
- virtual wards
- same day emergency care (SDEC)
Increase the use and impact of virtual wards
A virtual ward (also known as hospital at home) is an acute clinical service with staff, equipment, technologies, medication and skills usually provided in hospitals delivered to selected people in their usual place of residence, including care homes.
The service can support admission avoidance (step-up care) and be accessed directly from home and/or via a range of services such as general practice, a single point of access (SPoA), urgent community response (UCR), 999/111, SDEC or an ED. It can also facilitate earlier discharge or transfer from a hospital inpatient ward (step-down care), enabling individuals who are not medically optimised for discharge to continue to receive medical treatment, oversight and diagnostics at home.
Virtual wards should operate for a minimum of 12 hours a day (8am to 8pm), 7 days a week, with locally arranged provisions for out-of-hours cover. The length of stay on a virtual ward can be different for each person but is expected to be short (up to 14 days).
Change ideas
- Work towards the 10 core components of a virtual ward outlined in the virtual wards operational framework, including point of care testing for timely diagnosis; hospital-level interventions such as IV therapies (diuretics, fluids and antibiotics as a minimum); integrated pharmacy services to support safe and effective use of prescribed medicines and devices; access to remote monitoring to ensure safe monitoring of patients and flexible deployment of staff.
- Ensure capacity is adequately scaled to deliver efficiencies and respond to UEC demand (with broad criteria to accept patients providing they meet a high test of acuity).
- Link with SPoA to maximise access to step-up virtual wards and ensure there is closer working with UCR and SDEC services and accurate profiling on the Directory of Services (DoS). Prioritise referrals from care homes and 999/111.
- Consider developing virtual hubs staffed by dedicated teams that can take referrals from across hospital specialties to maximise referrals to step-down virtual wards and ensure access to specialist support is considered as part of virtual ward care.
- Ensure referrals to virtual wards are considered as part of twice-daily hospital ward rounds, and consider in-reach initiatives in both ED and inpatient wards to identify patients who could benefit from virtual ward care.
- Consider closer working with community respiratory, heart failure and UCR to enable shared care approaches and flexible deployment of the workforce across services.
Tracking indicators
In addition to local process measures linked to your change ideas (such as accepted and rejected referrals, LoS and acuity), the improvement analytics in the Model Health System feature the following process measures:
- number of virtual ward ‘beds’
- virtual ward occupancy (at least 80% in all virtual wards)
Hospitals should improve their recording of input costs for virtual wards (for example, workforce, digital infrastructure, diagnostics, medications and transport).
Resources
- Virtual wards operational framework
- GIRFT guide on making the most of virtual wards
- Pathways for acute respiratory illness, frailty and heart failure
- Access to diagnostics on virtual wards guidance
- Guide to setting up technology-enabled virtual wards
- virtual wards network
- case studies:
Increase the use and impact of SDECs
The SDEC service should operate for a minimum of 12 hours a day, 7 days a week in every acute hospital with a Type 1 ED in England. SDEC allows specialists, where possible, to care for patients on the same day of their arrival to hospital, as an alternative to an inpatient hospital stay. Direct access from 999, 111, primary and community care will help prevent overcrowding in EDs and improve the quality of care and experience for patients, and therefore the SDEC estate must never be bedded and used as inpatient capacity.
If, in the second half of 2024/25, every hospital increases the use of SDEC by 0.5% compared to 2023/24, 9,000 bed days will be freed up and 9,000 admissions avoided by the end of the year.
Resources
- SAMEDAY strategy and framework for development and delivery of SDEC
- SDEC index and SMARTool
- SDEC case studies
- SDEC collaboration platform
- SDEC workforce roles toolkit
- SDEC webinars
Change ideas
- Local profiling of demand for SDEC and adapting core opening hours to meet that demand.
- Local review of SDEC provision at weekends to meet demand.
- Local agreements to not bed SDEC overnight to maintain flow.
- Establish team job plans that support early review of all patients by a senior decision-maker as soon as possible or within a maximum of 14 hours of being in the hospital.
- Ensure there is appropriate resource to deliver SDEC services operationally and clinically.
- Ensure SDEC services are profiled in the DoS to enable direct access.
- Establish standardised, local access criteria for ambulance referral.
- Ensure SDEC activity is recorded on ECDS to enable system-wide monitoring and evaluation.
- Establish plans to co-locate SDEC services with specialties.
- Use self-assessment tools to benchmark and address gaps in SDEC provision.
Tracking indicators
In addition to local process measures linked to your change ideas, the following are in the improvement analytics:
- use of SDEC: SDEC activity as recorded in the Emergency Care Data Set (ECDS)
- size of the SDEC opportunity: volume of activity for non-elective patients with conditions amenable to SDEC (patients with an ‘SDEC index’ diagnosis) who have a 1, 2 or 3 day LoS
Systems should also record key input costs for SDEC including workforce, estate (for example, square meterage), digital infrastructure and diagnostics for all days of the week.
Right process
Optimising operational effectiveness by making best use of resources and minimising waste and delay
Standardised care processes
Internal professional standards (IPS) state, in writing, the expectations on all clinicians and other staff in the delivery of care. They ensure there are agreed values, behaviours, response times and escalation chains for each specialty and service where processes are not followed, or standards not achieved. These work best when:
- every clinical service agrees IPS that are consistent and complement each other
- they contain an unambiguous description of the values and behaviours expected and set measurable standards for which everyone is accountable
- they centre on patient care, are written with clinicians and are championed by the executive team
- they operate 7-days a week across all services and specialties
Robust IPS designed collaboratively with staff lead to:
- safer, more effective, timely UEC services
- timely standards for key internal processes: for example, inpatient scans, specialty opinion, treatment
- consistency of response and turnaround times across all patient pathways
- reduced waste and delays, minimal clinical handovers and bed moves
- empowered clinical leadership
- increased clinical and operational collaboration
- improved visibility of performance and the factors that affect it
Standardise care processes
If the change ideas are adopted, a 5% reduction in the total beds occupied by patients admitted for 14 days or longer on a non-elective pathway is deliverable.
This work will also help reduce 12-hour+ stays in ED.
Change ideas
- Where IPS do not exist or are not complete for all services, undertake executive-sponsored collaborative work to create and implement them, and make the core service standards explicit.
- After reviewing current compliance with existing IPS, assess the performance of each specialty and make the measurable time standards, for example diagnostic turnaround time, more explicit or more challenging. Consider implementing the standards in the GIRFT acute patient care standards.
- Designate an executive as IPS sponsor with a remit for holding the organisation and teams to account, as well as managing escalations and unblocking any issues identified.
- Undertake a thorough review of demand and capacity, taking into account UEC flow from ED and elective/cancer/diagnostic demand and capacity; ensure capacity is in place to meet IPS.
- Test IPS during times of overcrowding and increased pressure in ED; particularly the escalation process, which will involve medicine and surgery reaching into ED to support decision-making, flow and referrals.
- Implement changes to rostering and job planning to ensure the right resource to support delivery of IPS (see Right people section).
- Implement agile referrals to specialties – allowing, for example, conversations by telephone or secure messaging rather than electronic or paper referrals – or move to a full trusted assessor model.
- Review and standardise respiratory and cardiology pathways to reduce variation in specialty LoS.
- Ensure consistent access to diagnostics 7 days a week.
- Deliver networked rotas to access advice from low volume specialties and, out-of-hours, from high volume specialties.
- Minimise ward moves during an inpatient stay; get the patient to the right team first time.
Tracking indicators
These should be determined in line with the time standards you record locally: for example, the proportion of requests for specialty input actioned within 30 minutes.
Note: We do not advise looking at mean LoS as this is an overly simplistic measure that will be more sensitive to the ‘right place’ change actions for NEL admissions.
Resources
- GIRFT acute patient care standards
- ECIST rapid improvement guide
- NHS England Admitted Pathways Programme
- GIRFT 6 to help fix
Right pathway
Ensure all patients have a care plan, which they have been involved in, and the care plan is delivered
Care planning
If Internal Professional Standards (IPS) are how the UEC pathway works at an organisational level, care plans are the patient-level equivalent: how patients move through their care in a way that meets their individual needs. Consistent and standardised hospital processes are crucial to ensure everyone delivers care plans every day. Achieve this by:
- a senior clinical decision-maker carrying out a review within 12 hours of the patient being in the hospital, supported by shared decision-making conversations between the senior clinical decision-maker and patient
- developing a comprehensive care plan, with input from clinical teams, allied health professionals, discharge teams, patients (where they have the capacity to do so) and their carers and families, using the 4 patient questions, with set clinical criteria for discharge and an estimated discharge date within 14 hours of admission
- completing daily board rounds and starting ward rounds by 10am with a senior clinical decision-maker, senior nurse and members of the wider MDT, and an afternoon huddle to ensure all actions have been or are being delivered and, if not, to ensure these actions are escalated to the right colleagues or teams to urgently address them.
- continuously reviewing and updating care plans, supported by clear escalation processes
Optimise care and discharge planning
Having comprehensive care and discharge plans, with input from patients, their carers and families, that are delivered every day minimises waste and delays in patient care, reducing length of stay and the harm associated with it.
If change ideas are adopted, a 5% reduction in the total beds occupied by patients admitted for 14 days or longer on a non-elective pathway is deliverable.
Note: We do not advise looking at mean LoS as it is overly simplistic and will be affected by changes to NEL admissions generated by the ‘right place’ change actions.
Change ideas
- Ensure 100% of patients have comprehensive care plans. These plans are always developed by a consultant with the patient and their carer/family within 14 hours of admission.
- Ensure all patients can answer the 4 patient questions every day.
- Deliver comprehensive discharge plans, from the point of admission, for all patients. These must include the estimated discharge date and clinical criteria for discharge (clinical and physiological criteria with clear parameters for each, plan and follow up action as a minimum). Ensure patients requiring referral to care transfer hubs, and social care for those with more complex needs, are identified early.
- Implement criteria led discharge (CLD)
- Implement reconditioning/get up get dressed
- Embed a ‘home first’ approach in board and ward rounds and minimise decisions made about people’s long-term care needs when they return home, outside of their usual environment.
- Establish team job plans which support the early review of all patients by a senior decision maker and 7-day ward and board rounds (see Right people section).
- Where they exist, implement best practice, evidence based clinical pathways including #NOF, STEMI and stroke.
- Embed the flow principles throughout the patient pathway to eradicate overcrowding. This will involve making the best use of automated bed systems and embedding the principles of 7-day working.
- Maximise use of step-down virtual wards and hot clinics to reduce the time patients spend in hospital.
- Undertake weekly multi-disciplinary long length of stay reviews.
- Reduce variation in exit pathways between teams and days of the week and time of the day.
Tracking indicators
In addition to local process measures linked to your change ideas, the following can be used:
- number of beds occupied by patients with 14+ days LoS
- proportion of emergency admissions with 21+ days LoS
- patient reviews by senior decision-maker (local audit)
- proportion of comprehensive care plans in place where the 4 patient questions can be answered by patients or their carers / family members (local audit)
Resources
- NHS England Admitted Pathways Programme
- The 4 patient questions
- RCP modern ward rounds
- Hospital discharge and support guidance
- NHS England UEC pathway maturity self-assessment
- NHS England Universal Support Offer 2023
Right people
Utilising your workforce more effectively through high quality operational workforce planning and deployment will help improve staff experience and retention, support service improvement and further improve productivity by optimising the skills and capacity of your workforce.
Optimising the valuable skills and capacity of clinical workforces
Good quality workforce planning and deployment is about optimising the valuable skills and capacity of our clinical workforce by ensuring the right people are in the right place at the right time to deliver high quality, efficient patient care. It is about supporting the development of staff and services and providing the visibility of clinical capacity required to plan services effectively and match valuable clinical capacity to patient need.
Improvement requires targeted action on workforce planning and transformation, workforce deployment, governance and measurement.
Follow the resources on clinical workforce productivity on FutureNHS. In particular, we recommend the following resources for each of the 3 pillars of excellence, which are workforce planning and deployment; workforce transformation; and governance and measurement.
Workforce planning and deployment
Workforce planning and deployment resources
- e-job planning and e-rostering for effective planning and deployment of all staff:
- the Advancing levels of attainment handbook and related resources: helps organisations establish what their e-rostering and e-job planning levels of attainment are and what is required at each level to progress, based on local need and current position
- the e-job planning toolkit and e-rostering toolkit: provide a step-by-step guide to optimising system usage and embedding effective associated processes and governance
- e-rostering as an enabler to flexible working: provides resources to support team leaders working in clinical areas to develop ways to roster their staff more flexibly, thereby improving work-life balance and experience at work for staff. The case studies showcase the innovative initiatives that are being implemented and their impacts on staff wellbeing and retention
- medical consultant job planning improvement guide
- demand and capacity planning: provides resources to support service and system-level demand and capacity planning, including modelling tools and approaches, case studies, webinars and e-learning
- digital staff passport: enables NHS employees to use their smart phone to share employment, education and training, and occupational health details with hospitals 24/7, to support their moves between those hospitals
- agency toolkit: supports organisations to reduce their agency staff bills and encourage workers back into substantive and bank roles
Retention resources
- improving staff retention guide: supports line managers and employers to consider the key areas that affect workforce retention
- international retention toolkit: actions employers can take, such as mapping skillset and qualifications and setting up pastoral support, to ensure internationally recruited staff will want to stay, thrive and build lasting careers in the NHS
- NHS Emeritus: an initiative that connects recently retired and peri-retired clinicians across England with NHS providers of acute care who need the help only experienced clinicians can offer
Workforce transformation
Workforce transformation resources
- Clinically-Led Workforce and Activity Redesign (CLEAR) programme: supports clinicians and organisations to deliver transformation and workforce redesign projects to enhance patient care, by equipping frontline staff with skills in data analysis, innovation and leadership
- Star: accelerating workforce redesign: a model and workshop for workforce transformation, enabling you to explore workforce challenges, develop bespoke action plans and use resources in the Star online directory
- Roles explorer: provides resources for workforce redesign, such as introducing new roles or innovative adaptations to existing roles within a service or system
- Calderdale Framework: an evidence-based workforce transformation tool used in acute and community settings to rapidly identify skill sets required by services and their populations in acute, sub-acute and rehabilitation phases
Governance and measurement
Governance resources
- National Quality Board (NQB): safe sustainable and productive staffing guidance (2016): an improvement resource that builds on the NQB’s 2013 expectations and framework within which organisations and staff should make decisions about staffing that optimise productivity and efficiency while maintaining focus on improving quality
- e-rostering and e-job planning meaningful use standards: support hospitals to implement and use e-job planning and e-rostering software to its full potential, which includes the use of board reporting and metrics for improvement
Measurement resources
- care hours per patient day: guidance on the principal measure of nursing, midwifery and healthcare support staff deployment on inpatient wards
- Model Health System: data-driven improvement tool that enables NHS health systems and hospitals to benchmark quality and productivity
- Workforce Productivity Diagnostic Tool: supporting systems and hospitals to understand and benchmark their workforce productivity
Change ideas
Collect workforce data to understand your workforce capacity:
- capture and review data for all staff who work in urgent and emergency care on a permanent or temporary basis. Include data from/on ESR, temporary spend, recharge, recruitment and retention rates, turnover, sickness absence, age profile and demographics
- review your consultant-level capacity (including direct clinical care and supporting professional activity time)
Understand your retrospective and prospective activity:
- collect activity data and review any service plans that may impact on future activity levels (such as work transferring from location or changes in mode of delivery)
- this review should include key hours of operation
Undertake a systematic review of your workforce requirements:
- map your pathway and consider which staff are required at each stage
- review the roles, skills and capacity required to meet your expected activity. Consider whether any new roles are required or would improve productivity
- review your pay spend run rates and compare these to your budget
- consider recruitment, training and retention needs, including specific equipment or specialty training requirements
Review national policy when building your establishment and optimising deployment:
- Developing workforce safeguards: Supporting providers to deliver high quality care through safe and effective staffing
- GIRFT guidance
- appropriate Royal College guidance
Please share your ideas and feedback with us
Thank you for engaging with this guide. While we have collected a wide range of improvement ideas, we want to gather your local improvement ideas for inclusion in an updated version of this guide early in 2025.
Please share your ideas and feedback with us. There are 2 ways you can do this:
- by emailing us at england.clinops@nhs.net
- by feeding back through your local Learning and Improvement Network. Details on the networks are on the FutureNHS platform
Publication reference: PRN01435_iv (interim version)

