What do children, young people, families and carers want?
Young people, their families and carers who have experienced a mental health crisis developed these statements to tell us what they want and need when in crisis.
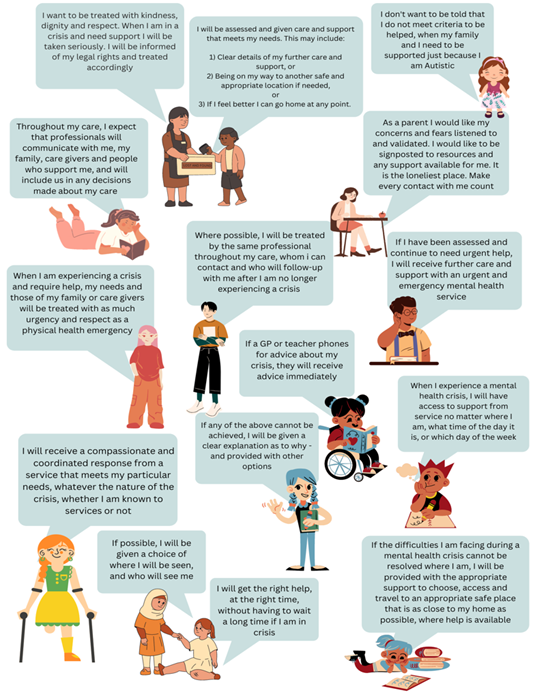
Figure 1: statements from young people, families and carers about the mental health care response they want when in crisis
Figure 1 includes statements from young people, families and carers about the mental health care response they want when in crisis. Key themes relate to receiving the right care at the right time, and being treated with dignity, respect and compassion. Young people, families and carers would like care and treatment to be provided close to home and at all times of the day and night, and young people want to be involved in all decisions about them and their care.
It is vital to seek and understand the views of children, young people, families and carers at all stages of their care journey. Ensuring that children and young people can have their say contributes to shared decision-making and will drive service improvements. Local leaders need to put appropriate governance structures in place for seeking and acting on feedback in a collaborative manner.
Figure 2: statements from young people who have experienced urgent and emergency mental health care about what it is like when they are and are not listened to
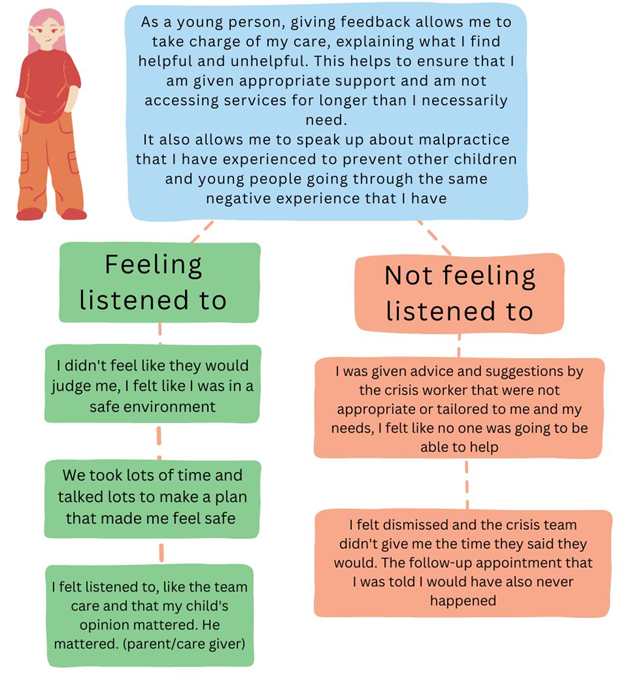
Figure 2 includes statements from young people who have experienced urgent and emergency mental health care about what it is like when they are and are not listened to. Feeling listened to included not being judged, having a safe environment and jointly planning their care. Not feeling listened to included feeling dismissed, not having follow-up appointments booked and being given advice that was not tailored to meet the young person’s needs.
Introduction
Improving the experience and outcomes of children and young people who present in a mental health crisis is a national priority. An approach that focuses on expanding the provision of care for them in their community and close to home or place of residence will reduce their need for admission, and where they do need to be admitted, provision of step-down services that are safe, effective and supportive will minimise inpatient length of stay.
This national operational guidance covers the 4 core functions of a comprehensive crisis offer for children and young people under 18 (aged up to 17 years and 364 days):
- Single point of access through NHS 111 ‘select mental health option’ to crisis support, advice and triage.
- Crisis biopsychosocial assessment in the emergency department and/or community settings.
- (a) Brief response in the emergency department and/or community settings, with (b) children and young people being offered brief interventions in the home and/or community.
- Intensive home treatment service for children and young people who might otherwise require inpatient care or intensive support that exceeds the normal capability of a generic children and young people’s mental health community team in the home and/or community.
This document is intended as supportive guidance for commissioners and providers as they continue to develop and enhance their local operational policies for the delivery of urgent and emergency mental health care for children and young people. Though primarily for commissioners and providers, this guidance will be relevant to primary care, voluntary, community and social enterprise organisations, local authorities, acute hospitals, as well as children, young people, families and carers.
This guidance updates and replaces the guidance we published on the FutureNHS platform in March 2020 (FutureNHS is a member platform that requires a log in). It reflects the significant change within the health and care system as a result of:
- the COVID-19 pandemic, which severely disrupted mental health services but also accelerated service transformation, such as with the rapid rollout of all-age urgent mental health lines
- The Health and Care Act 2022, which introduced integrated care boards (ICBs) and expanded provider collaboratives, changing the organisational landscape in which services are commissioned and provided
Promoting equality and addressing health inequalities are at the heart of NHS England’s values, and we have given due regard to this in the development of this guidance.
The guidance draws on new and innovative ways of working and up to date clinical advice, to ensure the crisis offer best meets the needs of children, young people, families and carers. It was produced in partnership with clinical, operational and policy stakeholders, and children, young people and parents with lived experience.
The guidance signposts to resources and training for staff, and resources that it may be helpful to share with children and young people, their parents or carers. Please note you need to register to access these resources on the FutureNHS platform (FutureNHS is a member platform that requires a log in).
Note: we use the terms ‘crisis’ and ‘urgent and emergency care’ interchangeably when referring to the intensive community, urgent and emergency pathway of care for children and young people experiencing mental health distress.
Background
Mental health difficulties are prevalent among children and young people and while the increasing need for mental health care has been apparent over the last decade, it exacerbated through the pandemic. The fourth (wave 4) in a series of follow-ups to the 2017 mental health of children and young people survey, conducted in 2023, identifies that 20.3% of children aged from 8 to16 years and 23.3% of young people aged from 17 to 19 years have a probable mental disorder, compared to 12.5% and 10.1% respectively in 2017. Prevalence rose between 2017 and 2020, but rates of probable mental disorder stabilised in all age groups between 2022 and 2023. In addition, a study by University College London (2020) found that 16% of young people report high levels of psychological distress by the age of 17 (based on data collected from 2018 to 2019), 24% report self-harming, and 7% report self-harming with suicidal intent at the age of 17.
Children and young people were disproportionately affected by disrupted routines and education, and a lack of social connections during the pandemic (Edwards et al 2023). More children and young people are presenting with multiple and complex needs, often in response to complex and ongoing trauma, as well as challenging personal and social circumstances. In some instances, children and young people may consequently be admitted to paediatric acute settings for their mental health needs and remain in hospital for long periods of time.
While inpatient admission can be necessary for children and young people with severe mental health difficulties, removing a young person from their local community and support structures and exposing them to a new and often unfamiliar environment can risk an escalation in their presentation and increase the risk of restriction and restraint (Hayes et al 2022). Children and young people with mental health needs should be supported in the community and hospital admissions should be avoided where possible.
The expansion of robust, intensive community-based care will improve the experience and outcomes for children, young people and their families and carers. Intensive community care services have been shown to reduce self-harm in adolescents, improve school reintegration (Ougrin et al 2018; 2020) and reduce the need for inpatient admission. Where a young person does need to be admitted, provision of safe, effective and supportive alternatives to admission and step-down services in their community can shorten their stay. Intensive community-based care will also reduce pressure on emergency departments (EDs), paediatric wards and the wider urgent and emergency mental health system.
Delivering the best possible care closer to home or in the place of residence for children and young people experiencing a mental health crisis requires collaboration across systems and pathways, including inpatient care, to develop integrated ways of working.
Policy context
The NHS Long Term Plan (2019) committed to giving all children and young people experiencing a mental health crisis access to age-appropriate crisis care 24 hours a day, 7 days a week.
The Mental Health Implementation Plan (2019) set out a national trajectory to achieve 100% coverage for children and young people’s crisis services, and an expectation that systems provide a comprehensive offer including access via the NHS 111 ‘select mental health option’, combined with crisis assessment, brief response, brief intervention and intensive home treatment functions by the end of 2023/24.
Comprehensive crisis services for children and young people should be delivered in the context of several other NHS Long Term Plan commitments:
- Continued expansion of community-based mental health services including through school and college-based mental health support teams so that, by the end of the period, an additional 345,000 children and young people aged from 0 to 25 can access NHS-funded mental health support.
- In selected areas, we will develop new services for children who have complex needs that are not currently being met. For 6,000 highly vulnerable children with complex trauma, these will provide consultation, advice, assessment, treatment and transition into integrated services.
- Increased investment in intensive, crisis and forensic community support will also enable more people who are autistic or have a learning disability to receive personalised care closer to home in the community, and reduce preventable admissions to inpatient services
- No more than 12 to 15 children and young people with a learning disability, autism or both per million population will be cared for in a mental health inpatient facility.
When considering the whole pathway of care for children and young people, the other publications and transformation programmes to consider include:
- The NHS England Learning Disability and Autism Programme. Since 2019, increased investment has enabled more autistic children and young people and those with a learning disability to receive personalised care in the community. From 2024 onwards, this investment has become recurrent to help systems embed their services. Additionally, over the last 5 years the programme has rolled out designated keyworkers for autistic children and young people and those with a learning disability who have the most complex needs, as recommended by the Lenehan Review (2017). This includes children and young people who are inpatients or at risk of being admitted, and those who face multiple vulnerabilities such as looked after and adopted children, and children and young people in transition between services. Every ICB now has an operational keyworker service.
- The children and young people with mental health needs in acute paediatric settings framework. This outlines how systems can ensure children and young people with complex mental health needs requiring care or medical stabilisation, and those who look after them, are better supported in acute paediatric settings.
- Mental Health, Learning Disability and Autism Inpatient Quality Transformation Programme. The programme has proposed core components for mental health services for children and young people (FutureNHS is a member platform that requires a log in), and is now working to agree a future service model that realises care and treatment from specialised mental health services for all children and young people who need this.
- Access and waiting time standards for children and young people’s community eating disorder services (CEDS) and early intervention in psychosis (EIP). This guidance should be read in conjunction with the updated EIP guidance and the revised guidance for children and young people’s eating disorders, due to be published in 2024.
- Mental health clinically led review of standards. The proposed standards ensure people who need care know when they can expect to receive it and support faster access to evidence-based care:
- for community-based mental health crisis services (all ages):
- for a ‘very urgent’ presentation, the patient should be seen within 4 hours from referral
- for an ‘urgent’ presentation, the patient should be seen within 24 hours from referral
- for mental health needs in an ED (all ages) a face-to-face assessment should start within 1 hour from referral, by a mental health liaison or children and young people’s equivalent service
- for community-based mental health crisis services (all ages):
At such time as the standards are implemented, we will update this guidance to reflect the changes.
A comprehensive mental health crisis care offer for children and young people
Principles of care
- Children and young people with mental health needs should be supported in the community, their place of residence or close to home (including in residential settings and paediatric wards). Mental health inpatient admissions should be avoided where possible.
- Provision of robust, intensive community-based care will prevent or reduce the need for mental health inpatient admission and reduce pressures on emergency departments (EDs), paediatric wards and the wider urgent and emergency mental health system.
- When a child or young person needs to be admitted, their length of stay will be minimised by providing appropriate alternatives to admission and step-down services that are safe, effective and supportive.
- The expansion of timely, age-appropriate and comprehensive crisis and intensive home treatment services will improve the experience and outcomes for children, young people and their families and carers.
Partnership working
Good working relationships built on trust and respect are crucial to collaborative partnership working, and partnerships support people’s access to a safe and effective response that is needs-led. There should be no wrong door in asking for help, and children, young people and their families or carers should know that when they do, they will get the help they need at the right time and in the least restrictive environment.
Multi-agency partners may include primary care and acute health services such as paediatric wards, EDs and inpatient services; emergency services such as police and ambulance; children’s local authority colleagues including social care; education, child health and universal teams; and voluntary, community and social enterprises (VCSE) services.
Integrated care systems (ICSs) and their integrated care partnerships (ICPs) should together plan how their services and organisations can be enabled to provide better support before a child or young person reaches the point of crisis, or to help integrate them back into the community as soon as possible: a proactive rather than a reactive response to mental health needs. Crisis can affect a child or young person’s rights to education and to be part of communities, so the earlier they get the right support, the greater the chances that their wider outcomes will not be adversely affected. Services will need to work with local provider collaboratives to develop an understanding of referral pathways and processes.
Proactive partnership working supports children and young people to be in the right environment and have access to the most appropriate care within their community. All partners who are identified to be part of the child or young person’s network should actively seek to build relationships with each other and understand each other’s roles and responsibilities, and to maximise the success of partnership arrangements all agencies need to be equally involved and engaged from the start.
Partners need joint mechanisms in place to support timely discussions and decision-making; otherwise, professional differences can mean a child or young person remains in an environment that may not best meet their needs. This may require clear escalation processes and structured resolution meetings.
Positive partnership working can involve:
- ensuring the voices are heard of all groups of children and young people who find themselves in mental health crisis, including those with a learning disability or who are autistic, as well as those of their families and carers, with co-production at the heart of all decision-making
- sharing system ownership of any challenges and seeking solutions. Partnership agreements developed, agreed and countersigned by all agencies can underpin this by ensuring the roles and responsibilities of each partner are clear. Local areas may consider setting up shared spaces for joint learning to break down organisational barriers
- creating a shared understanding of the needs of the child or young person and developing personalised shared care plans and risk assessments with children, young people, families, carers and the network
- ensuring regular and planned multi-agency meetings are held with key people from each organisation, with discussions focused on the interests of the child, young person and family or carers. This helps with planning together how best to support any children and young people they are concerned about or who are at risk of entering a period of crisis. Agencies should seek to come together regularly, for example monthly, and more frequently in extraordinary circumstances, to help build robust partnership working
- sharing appropriate information in the interests of the child or young person’s health and wellbeing
- having local joint approaches to monitoring the dynamic support register (DSR) and involvement in Care, Education and Treatment Reviews (CETRs) to ensure autistic children and young people and those with a learning disability who are at risk of admission to hospital are identified, and admission avoided where appropriate.
Tools/guidance for partnership discussions include:
- Situation, Background, Assessment, Recommendation (SBAR) provides a structure for discussions
- Cheshire and Merseyside children and young people’s complex needs escalation and support tool (CNEST) and Cheshire and Merseyside ICP children and young people’s mental health (CYPMH) gateway can guide multi-agency decision-making by supporting an evidence-based approach to identifying a child or young person’s risk issues, including of needing a period of care away from their home and community
- DSR and CETRs; these require cross-partner working and planning for children and young people who are autistic and/or have a learning disability
- Supporting children and young people with mental health needs in acute paediatric settings: a framework for systems
Describing a mental health crisis for a child or young person
Murphy et al (2015) suggest that a mental health crisis requires immediate risk management and stabilisation by a mental health care professional. It can have many underlying causes, diagnoses and triggers, some of which may be longstanding. These culminate in the deterioration of an individual’s mental state to the point they require an immediate response from mental health services.
Mind suggests that a mental health crisis is when a person feels at ‘breaking point’. This can include symptoms such as anxiety, suicidal thoughts and self-harm, but ultimately is when the individual may be at risk to themselves or those around them and presents in extreme psychological distress with or without self-harm (Edwards et al 2023). Distress can vary from person to person; however, it is important that the response is based on the needs of the child or young person and does not differ according to severity.
Crisis support for children and young people refers to the provision of specialised interventions and services during periods of acute mental health distress or instability. It involves a comprehensive and focused approach that addresses the immediate needs of a child or young person facing difficulties in remaining safe. This support may typically include rapid assessment and targeted therapeutic strategies to stabilise and ensure the safety of a child or young person. Timely and intensive support is critical to facilitate a journey of recovery and improved wellbeing, and often a multi-agency response is required.
The 4 core crisis functions
Collectively, the 4 functions (see table 1) aim to deliver comprehensive children and young people’s crisis care nationally.
A task and finish group consisting of clinical, operational and policy leads reviewed the functions in 2022/23 to consider the detail of each and how they combine to deliver the required 24/7 coverage of crisis provision across the country for children and young people under 18 years (up to 17 years and 364 days).
Changes were made to function 3, specifically to remove the reference to ‘assessment’ (covered by function 2) and to recommend extended hours of operation for brief intervention (rather than 24/7) as this is more clinically appropriate and complements the interventions offered in function 4 (intensive home treatment).
Table 1: 4 core crisis functions
|
Function |
Hours of operation |
|
1. Single point of access through NHS 111 ‘select mental health option’ to crisis support, advice and triage. |
24 hours a day, 7 days a week. |
|
2. Crisis biopsychosocial assessment in the emergency department and/or community settings. |
24 hours a day, 7 days a week in both the emergency department (ED) and community settings or a combination across both settings. |
|
3a. Brief response in the emergency department and/or community settings, with 3b. children and young people being offered brief interventions in the home and/or community. |
a. Brief response: 24 hours a day, 7 days a week in both the ED and community settings or a combination across both settings. b. Brief intervention: 7 days a week across locally determined extended hours in the home and/or community. |
|
4. Intensive home treatment service for children and young people who might otherwise require inpatient care or intensive support that exceeds the normal capability of a generic children and young people’s mental health community team in the home and/or community. |
7 days a week across locally determined extended hours in the home and/or community. |
Note: extended hours are hours outside the standard hours of operation (Monday to Friday, 9am to 5pm).
While we describe these functions separately in the following sections, their interdependencies across the whole urgent and emergency care pathway should be recognised. A child or young person’s journey should be thought about as a whole pathway, not discreet and separate interventions. Whole pathway in this context ranges from community support to specialist intensive support and inpatient admission (physical and mental health); for example, that created by Liverpool Child and Adolescent Mental Health Services (CAMHS).
Function 1: single point of access through NHS 111 ‘select mental health option’ to crisis support, advice and triage
Anyone seeking urgent mental health support in England can do so via NHS 111 ‘select mental health option’, as committed to in the NHS Long Term Plan. NHS England has developed pathway design principles (FutureNHS is a member platform that requires a log in) to inform rollout of the connection of urgent mental health helplines to NHS 111/integrated urgent care. This includes national minimum criteria that each area should implement to support integration of NHS 111 and urgent mental health services.
It is vital that ICSs work together across crisis pathways and support partnership working to ensure:
- the most convenient and age-appropriate crisis care services are available via NHS 111 ‘select mental health option’
- children and young people receive the most effective response to meet their needs
- all children and young people’s needs can be met, and this service has no exclusion categories
Successful implementation of urgent mental health helplines for children and young people requires local services, including primary care and local authorities, to agree and clearly define the role of each agency in supporting the child or young person in difficulty, without thresholds or boundaries. It also relies on local governance arrangements, including information sharing agreements, being in place.
A single point of access through NHS 111 provides a clear and easy route to access crisis support, advice and triage in a timely manner. Across each ICS footprint there will be an age-appropriate crisis service accessible to children, young people and their families and carers 24/7. In addition to offering children and young people a crisis response 24/7 via phone, crisis text services were introduced in August 2024. Crisis text services will ensure that services are able to meet the needs of the local populations, particularly for those who prefer to text as their primary way of seeking support; see the specification for these services (FutureNHS is a member platform that requires a log in).
Crisis practitioners, regardless of local crisis service operational models, should have age-appropriate skills and competencies to adequately triage, support and advise the child, young person, family or carer and their network. They should also be able to understand how to communicate with the network around the child or young person. Advice, support and triage may be sufficient to address the individual’s concerns, but contact may present an opportunity to signpost/refer the child or young people to a more appropriate service. Initial triage through the urgent mental health helpline may identify possible mental health needs and establish whether the child or young person requires a timely face-to-face crisis assessment with a specialist mental health professional.
Advice can be given when the crisis practitioner is able to listen and signpost to other relevant agencies. When support is being offered, this will be in the moment and through a compassionate and validating approach. It may involve safety planning, using/offering practical skills to help manage the distress, supporting the child or young person’s network if they have one in place, and often providing containment or de-escalation.
In the crisis call, the crisis practitioner needs to:
- make reasonable adjustments in line with the Equality Act 2010, including for Deaf individuals and those whose first language is not English
- establish rapport, listen and signpost or refer to appropriate services or agencies
- offer advice based on knowledge of local pathways, resources and how to access these
- undertake initial triage using an evidence-based triage tool to identify possible mental health problems and establish whether the child or young person requires a timely face-to-face crisis assessment with an age-appropriate mental health professional. The UK mental health triage scale can assist along with clinical judgement when determining timescales for responses. Locally developed frameworks are also recommended for continuity and consistency of responses. These need to be in line with urgent and emergency mental health waiting time standards categories
- conduct a brief risk assessment as part of the triage to understand the presenting risks. This will contribute to safety planning. Often a safety plan will include carers and the wider multi-agency network, and practitioners should be skilled in identifying which other agencies in the care network need to contribute to safety planning
The expectation in the NHS 111 ‘select mental health option’ national minimum criteria is that all call handlers and crisis practitioners have access to regular direct clinical supervision from a registered mental health professional. Local areas can decide how they provide access to a children and young people’s mental health professional. Local urgent mental health helplines will also determine whether they have call handlers or trained mental health professionals, or a combination of both.
All call handlers, crisis practitioners, managers and service leaders are required to complete the Oliver McGowan mandatory training on learning disabilities and autism.
Function 2: crisis biopsychosocial assessment in the emergency department and/or community settings
This function expects that a biopsychosocial assessment will be offered 24/7 face to face in the community and/or in acute settings by staff who are adequately trained and experienced in offering clinically age-appropriate assessment and formulation. A comprehensive biopsychosocial assessment will include an evaluation of the child or young person’s needs, safety considerations and vulnerabilities, a risk assessment and development of a safety plan.
A clear biopsychosocial assessment and risk assessment will enable the child or young person to feel supported and, as importantly, heard. It is key to get the assessment phase of their journey right, as this enables a more effective outcome without the child or young person having to repeat themselves. It is important to remember that the child or young person is the expert in themselves, and that the clinician’s role is to facilitate them in sharing their voice and views to enable them to access the right support for their needs. Reasonable adjustments should always be made to ensure views are heard from children and young people who may not be able to verbalise them. Considerations when conducting a biopsychosocial assessment are as follows:
- If, at the support, advice and triage stage (function 1), a more detailed biopsychosocial assessment is needed, then this should be completed face to face by clinicians trained and experienced in working with children and young people.
- This assessment can take place within the emergency department, hospital setting or community but account should be taken of the child or young person’s needs, local lone working policies and the time of the assessment. Where possible, the environment should be a private designated area to enable open and safe dialogue, and the child or young person should be given a choice in where they are seen and assessed.
- Biopsychosocial assessments that take place in the community will require careful risk planning, including to ensure clinician safety. Known risk information will be used to inform decision-making about the most appropriate environment, alongside multidisciplinary team (MDT) guidance and consultation. Further detail can be found in the operational considerations section below.
- The assessment should include gathering a clear understanding of the individual’s needs, their care and support system (including contact with other services), any physical health needs, any history of drug or alcohol use, and any safeguarding concerns. The child or young person, and where appropriate their family, carers or support network, should be involved in the decision-making process to formulate the care and safety plan.
- If the child or young person is known to other agencies, for example children’s social care, then conducting a joint assessment may be in their interest, for continuity of care, to avoid the child or young person needing to repeat their story to multiple people, and for shared safety planning. Positive practice would also suggest that ideally the young person is supported by the same professional in any follow-up appointments. The process should be therapeutic, validating the child or young person’s distress and understanding factors linked to increased risks of harm. It is essential to keep the voice of the child or young person at the heart of the assessment while taking into consideration any safeguarding concerns that arise. Clinicians should ensure that any vulnerabilities and any required reasonable adjustments are considered, and adaptations to the assessment made accordingly.
- Any safeguarding concerns that arise should be responded to in adherence with local safeguarding protocols. It is important that all clinicians are clear on roles and responsibilities in relation to safeguarding children and young people.
- It is essential to ensure reasonable adjustments are made within the assessment for children and young people with a learning disability or who are autistic. This can be supported by a joint assessment with a learning disability liaison nurse or the learning disability community team. A ‘trusted person’ could also be drawn on to aid good communication. Specific considerations for those with a learning disability within acute settings, EDs and paediatric wards can be found in the CYPMH in acute settings framework.
- There should be adequately trained children and young people mental health clinicians within this function and across the crisis pathways, who are able to conduct assessment under the Mental Health Act 1983. This will be to determine whether a mental health inpatient stay may be required but also to support the assessment of those detained under section 136 of the Mental Health Act. The assessment process will take into account the least restrictive options available, and clinicians will work in adherence with the code of practice for the Mental Health Act 1983. It will be critical that mental health trained clinicians are able to support and consult with any staff who are looking after children and young people detained under the Mental Health Act in environments outside a mental health inpatient admission, such as paediatric wards and the health-based place of safety.
- Children and young people will present with a range of needs that require specialist, tailored biopsychosocial assessment and risk planning, such as eating disorders, self-harm, suicidal ideation and psychosis. Assessing clinicians will need to draw on existing guidance where necessary to ensure the correct assessment and pathway of support is put in place. Such guidance includes but is not limited to: Community eating disorder care pathway, the Early intervention in psychosis access and waiting time standard and the psychosis pathway. Getting it Right First Time (GIRFT) has produced a psychosis in children and young people flowchart highlighting those interventions that can be provided within the crisis pathway.
- Risk assessments: as part of the biopsychosocial assessment a risk assessment will be completed and a safety plan developed, which will be derived from a formulation. When considering risk, the clinician will be considering risks to self and others, as well as from others. Risk to and from others will include any vulnerabilities and safeguarding concerns. It is also important to take account of past behaviour (for example, is this a first presentation, has there been previous harm and has this escalated?), the intention behind the presenting behaviour and any thoughts or plans to repeat the behaviour or to end their life. It is important to try and understand the context of the behaviour and what might make it more or less likely in the future; gather information on any current protective factors and the child or young person’s ability to think about the future, both short and longer term; and to gather information and formulate risk in a collaborative way to inform a detailed safety plan. In line with National Institute for Health and Care Excellence guidelines, risk should not be categorised into arbitrary measures such as low, medium and high. It should be descriptive in the context of the child or young person and the recognition that it is personalised and not static in nature.
- Safety plans, such as the Samaritans Creating a ‘safety plan’, should be written in collaboration with the child or young person, and their family or carers if appropriate, or an alternative agency or member of the support network. They should be individualised and meaningful and provided in a visual format that is accessible for the child or young person. Safety planning should include consideration of social media safety; the e-Learning for healthcare training module Internet safety, suicide and self-harm covers risks associated with social media, and the Samaritans media toolkit is useful for learning about internet safety around suicide and self-harm.
Function 3: (a) brief response in the emergency department and/or community settings, with (b) children and young people being offered brief interventions in the home and/or community
Function 3 provides all children and young people under 18 years (up to 17 years and 364 days) who present in a mental health crisis with a universal initial response regardless of ongoing needs: the offer of brief responses 24/7 and brief interventions over extended hours. The approach within both the brief response and brief intervention should be systemic, holistic, trauma informed and person centred. When considering any intervention for children and young people in urgent and emergency situations, their network of support, such as parents and carers, needs to be involved in all decision-making and planning of care. They need to be supported to feel empowered as a system to manage crisis where possible and practicable.
There is growing evidence that providing a brief response and/or intervention following a presentation of self-harm or suicidal ideation reduces re-presentation and reported negative symptoms; for example, a follow-up telephone call following discharge (Rengasamy and Sparks 2019). Zullo et al (2020) highlighted that a therapeutic approach in the assessment process significantly correlated with an increase in adolescent mood and a decrease in expressed suicidal thoughts. Focused interventions such as dialectical behavioural therapy (DBT) for adolescents and mentalisation approaches have tentatively been shown to be effective as brief interventions (Ougrin et al 2015) but, as outlined in a Cochrane review (Witt et al 2021), there is a paucity of research in this area.
Stanley et al (2018) showed that a safety plan intervention following a suicidal ideation presentation at EDs significantly correlated with a reduction in suicidal behaviour and an increase in treatment engagement in an adult population. Bettis et al (2020) found similar in the adolescent population while further highlighting the need and benefit of providing an immediate age-appropriate crisis response.
There is also growing evidence for the benefit of offering brief interventions for children and young people presenting in a mental health crisis (for example, Haruvi Catalan et al 2020; Dekel et al 2021; Cloutier et al 2022). Such targeted brief interventions following crisis can reduce suicidal ideation, depressive symptoms, anxiety and perceived stress. They are also associated with reduced waiting lists for core community teams due to a number of children and young people not needing onward therapy following the intensive intervention, and an overall reduction in hospital admissions (Kwok et al 2016).
Brief response
The brief response should be available 24/7 and is designed to be offered in the moment and the days following a presentation in crisis, usually after a biopsychosocial assessment. It will have various formats depending on the time of day and environment in which the child or young person presents.
It is a space for the child or young person to be heard and understood, and the opportunity to start building a shared understanding and plan across any existing professional and social support network, and to pull in additional services that might be needed. This will make the child or young person and their families or carers feel supported and provide them with strategies, advice and signposting. It also provides space for timely brief interventions as required.
Brief intervention
The brief intervention provides an emotionally containing space (for the child or young person and the network around them) to better understand what has led to and what is maintaining the crisis, building on and driven by the clinical formulation and risk assessment. It will likely focus more on building therapeutic alliance, providing emotional containment and regulation for the child or young person and their family or carers, and developing the clinical formulation to inform the intervention. This understanding will then inform a shared plan for interim and longer-term support.
By offering brief intervention over extended hours in the days following presentation, support can be given when and where it is most needed (for example, before school, mealtimes, medication administration times and bedtime). It is important that all brief interventions are tailored to meet the specific needs of the child or young person and their presenting symptoms. Some such presentations may include, but are not limited to, eating disorders, psychosis, suicidal risk, low mood and obsessive-compulsive disorders.
Another important aspect of offering a brief intervention will be capturing risk and the development of a safety plan. Safeguarding will need to be considered in respect of whether the child or young person is contextually safe and, if not, what services and/or plans need to be put in place to address this. If children and young people are in residential homes, this may involve working with the staff of these homes.
Unlike function 4, the brief intervention may not follow one intervention model. Approaches will likely be informed by models such as mentalisation, cognitive behavioural therapy (CBT), eye movement desensitization and reprocessing (EMDR), dialectical behaviour therapy (DBT), motivational interviewing, and acceptance and commitment therapy (see table 2 under function 4). They may also include pharmacological and medical monitoring.
Considerations for delivery of brief response and brief intervention include:
Capacity to give consent
- Capacity is assessed at the times when consent to provide an intervention is required, and among the issues to consider relating to consent for children and young people is the role of parents and carers. Further information can be found in consent to treatment – assessing capacity and making decisions – professional standards.
- Often children and young people may not feel able to accept an intervention, but their parents or carers may be able to engage in work to support the child or young person. This should be considered where clinically appropriate.
- There may also be occasions where families or carers and children and young people have differences in opinion on interventions, and clinicians will need to work with them to seek resolution, drawing on the wider MDT where these differences increase risks for the child or young person.
Timeframe
- Brief intervention will begin as soon as the child or young person is presenting in crisis. However, depending on the child or young person’s needs, there may need to be some flexibility in the overall timeframe of the intervention.
- It might include up to 4 sessions following a biopsychosocial assessment (on average) but should be brief in nature and these sessions would therefore be unlikely to span longer than 1 to 2 weeks.
- Exit from the brief response/intervention will depend on the assessed need and risk of the child or young person’s presenting crisis. It could lead to an intensive support intervention (see function 4 below), a referral into another appropriate service or involve signposting to care provision that can better meet their needs.
Flexibility in approach and reasonable adjustments
- Children and young people from the community who tend not to seek help from statutory services often need this support the most. Having flexibility in approach, choice and taking time to understand what the barriers might be for the child or young person and their family could help engage them; for example, thinking about language or cultural barriers, appropriate and available safe spaces, and their understanding and experience of mental health and care services.
- The presentation of any co-occurring needs should also be considered. For a child or young person who presents in crisis and who is autistic, has a learning disability or is neurodivergent, this means considering their presenting behaviours and whether these are indicative of a mental health crisis or other challenges because their needs are not being effectively met.
- Consider sensory preferences and use of translation services, British Sign Language interpreters or lip speakers for the Deaf, easy read information, pictorial information and any other reasonable adjustments.
- Reasonable adjustments for disabled children and young people, including those with a learning disability and/or who are autistic or neurodivergent, recognising that this group may not be able to engage with the brief response or intervention themselves without adjustments. For autistic children and young people and those with a learning disability, consider whether they have had a CETR. This supports a multi-agency plan of care that is the least restrictive and focused on community-based provision where possible.
Function 4: intensive home treatment service for children and young people who might otherwise require inpatient care, or intensive support that exceeds the normal capability of a generic children and young people’s mental health community team in the home and/or community
Function 4 offers an intensive home treatment (IHT) service for children and young people who, following assessment and formulation, are felt to:
- Need urgent and intensive support for their mental health needs to prevent inpatient admission or to transition from inpatient admission back to a community setting.
- Require time-limited intensive support that is beyond the capability of other commissioned children and young people’s mental health services.
This offer will be available 7 days a week to under 18s (up to 17 years and 364 days) and beyond normal working day hours (9am to 5pm). The exact hours will depend on local need and local partner service offers.
Points of access for IHT support may be after a biopsychosocial assessment and brief intervention or through locally agreed pathways for those children and young people whose level of risks may require more intensive support.
IHT includes home and/or community-based interventions (see table 2 below), up to at least 3 times a week and on multiple times a day if required, and usually for between 4 and 12 weeks depending on clinical need. It can be seen as a step up from brief intervention as outlined in function 3 and will be derived from the clinical formulation developed with the child or young person and their family or carers.
IHT should take a holistic approach with all relevant areas of the child or young person’s and their family’s or carer’s life considered (for example, home, school, workplace, respite), and focus on reducing the immediate risk of crisis and stabilising the child or young person’s mental state. Interventions will be goal based and have clear routine outcome measures to help with shared goal setting and understanding of issues, as well as to capture and review impact. Continuity of care and partnership working are essential to ensure the best outcomes for the child or young person.
The children and young people offered IHT will include (but not be limited to) those with eating disorders, psychosis, depression, severe obsessive-compulsive disorders, emotional dysregulation, post-traumatic stress disorders, severe anxiety and panic. The nature of the presentation should not influence or limit the involvement of the IHT service.
Research on the efficacy of home-based treatment has largely focused on the well-established home treatment services for adults. However, one review of randomised control trials comparing intensive community services with inpatient care for adolescents found both achieved similar clinical improvements, but intensive community treatment also reduced hospital stays and led to greater satisfaction in young people (Kwok et al 2016). A recent review of the provision and receipt of crisis support for children and young people (Edwards et al 2023) highlighted that crisis care should be offered as close as possible to where the child or young person lives.
Considerations for delivery of IHT include:
System-wide approach
- The network around the child or young person, including their family and carers, should be fully involved in any interventions and care planning. Factors that may disadvantage the child, young person, family or carer engagement in intensive support interventions should be considered, for example:
- parent or carer engagement may mean taking time off work; for financial and practical reasons this may put additional stress on a family
- if a child or young person needs to take time off school they may miss out on social and educational opportunities
- certain groups, including racialised groups, may be reluctant to engage because they mistrust services
Curiosity about any barriers and being mindful of the impact of any asks on a family, carer, child or young person will mean solutions are sought.
- A system-wide approach to supporting a child or young person and their parents or carers through the crisis and IHT pathway is imperative for sustainable and meaningful outcomes; this includes education, social care, VCSEs and any other relevant networks around the child or young person.
- When children and young people are known to other services (EIP, CEDS, DBT, community children and young people mental health teams), these need to work in partnership with the IHT team and be involved in care planning and transition arrangements from the IHT team once the child or young person is stable enough and it is safe to do so.
- For children and young people not known to any services but who require onward care once the intervention is completed, it is important that adequate arrangements are made to ensure a safe and swift transition into the right care team.
As an example, for a child or young person with an eating disorder/disordered eating presentation, it will be vital for the IHT team to work in partnership with the CEDS team if deemed clinically appropriate and dependent on the child or young person’s needs and formulation. This should be discussed and agreed with the CEDS team and if clinically helpful, support and evidence-based interventions may be offered via the IHT team as part of an overall treatment plan.
Continuity of care
- Interventions should follow the individual to ensure continuity of care; for example, when a child or young person is admitted to a paediatric ward or placed in a residential setting locally. If a child or young person is placed in a residential setting out of area, the IHT and local children and young people mental health services will work together to ensure a seamless transition of care, while working towards supporting the young person’s return to their local community as out of area care should be avoided where possible.
- Planning for the end of the intervention should begin as soon as it starts, with discussions around how to step down to less intensive services and achieve realistic goals. Routine outcome measures, safety planning and thinking about how ongoing risk can be safely held will all be important in guiding endings.
- Where possible the IHT team will act as a gatekeeper to inpatient admissions in collaboration with local provider collaboratives. Any child or young person for whom inpatient mental health admission is being considered should be discussed with the IHT team in the first instance. If an IHT intervention can support a child or young person to remain in the community, it should be considered as an alternative.
- Where possible the staff who engage with the child or young person and their family or carer should stay the same throughout the episode of care. This is to minimise disruption in the child or young person’s environment.
Interventions and staffing skill mix
There needs to be flexibility in the interventions offered as these need to be specific to the needs and presentation of the child or young person, but generally they should be:
- based on a clear clinical rationale (that is, drawn from assessment and formulation)
- meaningful and realistic for the child, young person and their family or carer
- evidence-based
- least intrusive and restrictive
- systemic and holistic (that is, include family or carer and wider systems around the child or young person)
- differentiated and adapted to age to meet the needs of both primary and secondary school aged children, with any reasonable adjustments made (for example, for being autistic/neurodivergent, having a learning disability, deafness)
Table 2 below lists evidence-based therapeutic models/interventions to draw from. It is not an exhaustive list of the interventions provided within crisis and intensive community support pathways.
The most recent edition of The Royal College of Psychiatry Quality Network for Crisis Resolution and Home Treatment Teams (QN-CRHTT) standards (2022) includes standards for children and young people. These can be used to consider what is important for intensive home-based crisis care services for children and young people and set standards for service provision and structure; staffing and training; assessment, care planning and treatment; and patient and family or carer experience.
Staffing considerations include:
- the staffing skill mix within the service should ideally include, but not be limited to, psychology, nursing, speech and language, social care, occupational therapy and psychiatry professionals
- pharmacological interventions will form part of the care plan for many young people receiving intensive home interventions. The workforce needs the capabilities and capacity to provide this level of intervention
- the team also needs adequately trained professionals to provide robust physical health monitoring where indicated. Children and young people’s care plans should cover physical as well as mental health needs where possible
Table 2: therapeutic models/interventions
|
Adaptive mentalisation based integrative treatment (AMBIT) |
Encourages a wraparound care approach with professionals and family coming together to provide a joined-up intervention. |
|
Dialectical behaviour therapy (DBT) |
An evidence-based psychotherapy that aims to support individuals who experience intensive emotions, through individual, group and systemic work. |
|
Cognitive behaviour therapy (CBT) |
A talking therapy that looks at the link between the way someone thinks, feels and behaves. It can be used to challenge unhelpful and intrusive thoughts, influencing how someone feels and behaves. |
|
Systemic approach |
Focuses on supporting change within the system/relationships around a child or young person, to support change in the child or young person. |
|
Positive behaviour therapy (PBT) |
Person-centred approach that aims to identify and meet the needs of individuals who are distressed and/or at risk of self-harming. It supports the individual to meet any needs in more healthy ways that reduce their distress and risk of harm. |
|
Acceptance and commitment therapy (ACT) |
A form of psychotherapy that challenges negative thinking patterns and behaviours. It encourages acceptance of circumstances and a commitment to healthy and constructive activities in line with values and goals. |
|
Developing therapeutic relationships |
Where a therapeutic approach is needed, this supersedes all other models. Clinicians and practitioners need to be compassionate, warm, responsive, have active listening skills and build relationships that are safe and meaningful to the child or young person, taking account of their needs, previous experiences and own relationships to help and care. |
|
Eye movement desensitization and reprocessing (EMDR) |
Supports children and young people to process traumatic experiences and other distressing life events. |
|
Pharmacological interventions |
Prescribing and monitoring the appropriate medications in line with guidelines and the evidence base alongside therapeutic interventions. |
|
Physical health monitoring |
Involves regular assessment and observations to ensure the physical safety and needs of a child or young person are met. It may include monitoring vital signs and assessing injuries. |
Operational considerations
Operational considerations when commissioning and delivering crisis care services for children and young people include:
- gathering feedback to support service development through co-production: services should have clear processes and systems in place for the collation and response to feedback from children, young people and families or carers, but with the flexibility to tailor their methods to meet the needs of the child or young person. Clinicians should seek to gather feedback when children, young people, families or carers feel ‘safe to share’; and to do so in several ways, such as using the Friends and Family Test, CHI-ESQ, participation groups, offering digital mechanisms, and creating easy read and language options.
“I sometimes find providing direct feedback to someone difficult and this feeling of unease is exacerbated if I am in crisis or just had a terrible interaction. Therefore, whenever a crisis worker or therapist has asked me for feedback after a meeting with them – even in the case of how I am feeling after talking to them – unless there is already a level of trust, I tend to provide positive feedback. This stops me from being put on the spot and asked to divulge information concerning why I didn’t find something helpful. It also prevents me from feeling any worse for potentially upsetting the crisis worker or therapist. Therefore, providing feedback afterwards to someone impartial or anonymously in a private space would benefit me as I would feel like I am able to speak truthfully without having to hold space for the other person’s emotions in the same way”.
- listening and responding to concerns and complaints from children, young people, their families and carers is essential to ensure safe and responsive services are provided that improve experiences
- local governance structures should be in place to support complaint handling, such as Ask Listen Do
- carers have rights themselves to support and help, including through carer contingency plans and the Carer contingency planning: recommendations for integrated care systems (ICSs)
- professionals across the crisis pathway need to build and develop positive and trusting relationships, to ensure a values-based approach is taken when addressing professional differences
- where possible, the MDT and other professionals involved in the care of the child or young person should provide continuity of care
- a multi-agency commitment to supporting children and young people in crisis. This may be between acute settings, community mental health settings, primary care, social care, education, VCSE partners, IHT or inpatient services, but will be based on the needs of the child or young person
- multi-agency protocols should be in place to provide a clear understanding of roles, responsibilities and escalation processes, should they be required
- information sharing agreements should be in place locally to enable the sharing of relevant and risk-related information across agencies without delay, so that decisions can be swiftly taken and no child or young people has to repeat their story more than is necessary. General Data Protection Regulation data management requirements and the confidentiality of the child, young person, parent or carer are always the primary consideration. A child and young person’s mental health service information passport can be used to avoid children or young people needing to repeat their stories.
- ICSs and providers should work together to understand local need through data and service user feedback, to inform models of crisis care
- to ensure equitable access to services, reasonable adjustments need to be made for disabled children and young people, those with a learning disability and/or who are autistic/neurodivergent, those whose first language is not English, and those with hearing, visual/sight or speech impairments
- the children and young people crisis pathways should be staffed with adequate clinical and operational expertise and leadership to fulfil all the requirements of the pathway. The team size and diversity will reflect local population size, geography and demands
- given the hours of operation, lone working policies and on-call arrangements should be in place to support clinicians delivering crisis care. Staff wellbeing and safety are uppermost in crisis services, and staff should have access to regular supervision, continuous professional development, training and other support mechanisms.
Health inequalities
Health inequalities are a persistent problem, with certain groups experiencing poorer health outcomes than others. These inequalities are created and exacerbated by a range of factors, including social, economic and environmental factors, and can lead to significant disparities in health outcomes. Recent societal changes, such as from the COVID-19 pandemic and the cost-of-living crisis, have further increased the inequalities that already exist nationally, making it more important than ever to address these issues.
Useful definitions of health inequalities include “avoidable, unfair, and systematic differences in health between different groups of people” (Maguire 2022) and “inequalities arising from unfair conditions faced by persons with disabilities, including stigma, discrimination, poverty, exclusion from education and employment, and barriers faced in the health system itself” (World Health Organization 2023). However, it is important to note these definitions will need to evolve as new areas for potential health inequalities emerge. For example, digital poverty is now a valid health inequality that did not exist 20 years ago.
Nationally, there has been significant focus on reducing inequalities within children and young people’s mental health. A Core20PLUS5 approach to reducing health inequalities at both a national and system level has been established for children and young people, where mental health is 1 of the ‘5’ clinical areas of focus. In addition, the Advancing mental health equalities (AMHE) strategy, published in 2020, summarises the core actions that need to be taken to ‘bridge the gap’ for communities faring worse than others in relation to mental health.
One of the key outputs from the AMHE strategy is the Patient and carer race equality framework (PCREF), which launched in October 2023. The PCREF is a mandatory anti-racism framework for all mental health trusts and service providers to embed across England. It aims to ensure that trusts and providers are responsible for co-producing and implementing concrete actions to reduce racial inequality within their services and will become part of the Care Quality Commission’s and Equality and Human Rights Commission’s inspection processes. Commissioners and service providers should consider the aims and objectives of both the PCREF and AMHE strategy when establishing how best to meet the needs of children and young people in crisis services.
Within NHS England, there is a particular focus on meeting the needs of those with a learning disability or who are autistic and also have a mental health condition. They can experience multiple health inequalities, poor outcomes and very long lengths of stay in mental health hospitals. Commissioners and providers should have a specific focus on ensuring all effective measures, including use of the dynamic support register and Care, Education and Treatment Reviews, are used to support autistic children and young people and those with a learning disability who may be at risk of admission to a mental health hospital to receive care and treatment in the community.
To support the provision of equitable health access for local populations, clinicians, service providers and/or commissioners should:
- have a good understanding of how local characteristics and related health inequalities impact on the local population, their needs and any barriers that may exist to accessing services. The Office for Health Improvement Disparities Fingertips profiling is a helpful local tool developed to support identification of needs through gathering data intelligence
- ensure that all service design and implementation consider the local population’s needs, with particular focus on how those not currently reached by the service will be catered for. (Note: the term ‘hard to reach’ is often used to refer to those experiencing health inequalities but can be problematical as it implies these individuals avoid or do not try to access health services. A change in emphasis with the better term ‘populations not reached by our service’ encourages services to reflect on their role in addressing inequalities and take steps to reduce barriers to access)
- ensure that commissioning intentions are set collaboratively with experts by experience, including those who identify within populations not reached by the service and minority groups
- instil a culture of shared learning across the system in relation to health inequalities
- engage with local communities/neighbourhood leads and local voluntary, community and social enterprises to improve awareness of the crisis support available locally and improve access for all local communities. Consider social media and local radio for engaging with communities to improve awareness of the support available
With specific reference to the workforce, systems and services should:
- ensure that clinical staff are supported to understand and reflect on the local population’s health inequalities and be supported to use data on health inequalities to adapt assessments and formulations of needs for children and young people accessing the services. There should be evidence of how this information is collated to inform future service review, redesign and commissioning
- ensure workforce development plans and training prioritise addressing health inequalities in access and support for particularly vulnerable groups of children and young people who often present in crisis situations. This includes but is not limited to:
- LGBTQ+
- looked after children
- young offenders or those involved in the criminal justice system
- homeless children and young people and those from deprived areas and/or low income backgrounds
- children and young people who are autistic, have a learning disability, are neurodivergent and/or have additional/special educational needs and disabilities
- sight/visual, speech and hearing-impaired children and young people
- children and young people from racialised and ethnic minority communities
- children and young people with addictions or substance misuse
- children and young people with poor literacy or health literacy, or those whose first language is not English
- children and young people living in remote, rural and island locations
- refugees, asylum seekers and those experiencing modern slavery
- efforts should be made to ensure that these groups receive equitable access to healthcare services and support, addressing the specific challenges they face and promoting improved health outcomes
- consider the support, education and experience clinicians need to appropriately and actively engage with those who have differing circumstances and cultural/religious backgrounds
- consider the support, education and experience clinicians need to appropriately and actively provide children and young people with a complex network of support, such as to meet their health, social care and educational needs
- consider ways of widening the diversity of the workforce so that it better reflects the local communities
- be able to evidence the knowledge and skills of clinicians when supporting those from populations not reached by their service and minority groups
- ensure that the workforce is familiar with the impact of both physical and mental health and can apply strategies to ensure there is parity across the interface of physical and mental health services
- ensure that children, young people and families or carers are enabled and empowered to routinely feedback on their experience of the staff engagement, compassion and understanding of their specific needs
- encourage clinicians to utilise clinical supervision and informal peer shared learning in addressing unconscious bias
Workforce
This section provides an overview of the key workforce knowledge and skills, and suggests the training systems should provide, as well as signposting to useful resources and the national training offer.
Workforce is the most crucial resource in crisis provision. We acknowledge the significance of nurturing essential competencies, capabilities and skills among our staff. Alongside this, we emphasise the importance of providing ongoing supervision, support and education to ensure their continuous growth. We also prioritise offering opportunities to staff to access both local and national training programmes. These measures foster a supportive environment where the workforce feels empowered, confident and equipped to support children and young people in crisis and deliver effective interventions that yield positive outcomes.
The modern approach to mental health services recognises the importance of a workforce capable of effectively engaging with children and young people facing mental health crisis and acute emotional distress. This necessitates the development of a core skill set in crisis management. However, it is equally vital for the workforce to be able to apply these skills within the specific context of children, young people and their families or carers. In the past, workforce development has often focused on one area or the other. However, with the evolving understanding of the needs of children and young people in crisis, there has been a shift towards transforming the workforce to ensure that teams and staff possess expertise in both domains. This transformation aims to provide comprehensive support and services that effectively address the unique challenges and complexities faced by children, young people and their families or carers during times of crisis.
The workforce of a children and young people’s mental health crisis service should comprise staff with the skills, training, capabilities and experience in working with children and young people and their families or carers, and effectively supporting staff in their work through clinical supervision, continuous professional development (CPD) and management arrangements. Any workforce development plans and training should also address inequalities of access and support for particularly vulnerable groups of children and young people, which will vary across the country based on local communities. For those who do not work in crisis services but are involved in caring for children and young people in emergency situations, an e-Learning for Healthcare platform has been developed to support the wider workforce. Workforce composition and size may vary in different regions, influenced by factors such as the local context and numbers requiring crisis services. Moreover, the availability nationally and locally of specific roles will shape the structure of individual teams or services. However, the following workforce principles apply to all services and teams:
- The workforce serving children and young people requires a diverse range of professionals with specialised expertise. It is essential to have staff from core professions who reflect and possess cultural competences and a deep understanding of the diverse needs, including ethnic diversity, of the local area and population they serve. This ensures the provision of tailored support that addresses the specific requirements of children and young people in the community.
- In building the workforce, it is crucial to consider all relevant protected characteristics (age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex and sexual orientation). This commitment can be achieved by implementing recruitment, retention and promotion practices that prioritise workforce equality, diversity and inclusivity.
- Children and young people’s crisis teams are most effective when they are multidisciplinary, bringing together professionals with core professional training, as well as incorporating roles such as peer support workers/social prescriber link workers, parent or carer representatives, children’s social workers, assistant psychologists and youth intensive psychological practitioners. This approach not only ensures access to a broad range of evidence-based interventions, such as pharmacological and psychological, but also promotes diversity and representation within the children and young people’s crisis workforce. A multidisciplinary team (MDT) provides essential risk and safety management within children and young people’s crisis care. By having a broad and diverse MDT there is an opportunity for critical ‘check and challenge’ among professionals. Robust discussions within the team can ensure that each child or young person receives an optimal assessment, formulation, opinion, and subsequent intervention and support as a consequence of well-informed professional debate. Core professionals may include, but are not limited to, psychological therapists, mental health nurses, child and adolescent psychiatrists and allied health professionals.
- To deliver effective crisis support to children, young people and their families or carers, it is essential for all staff to receive reflective supervision that helps them integrate their professional skills within the context of their practice. This process should involve outlining and agreeing their development needs within this specific area. Reflective supervision includes both formal specialist CPD opportunities and ongoing supervisory contact. The focus of reflective supervision will vary depending on the individual’s core competencies. It may encompass crisis mental health work or may be more centred on working with children and young people specifically. The purpose is to provide a supportive space for staff to explore and enhance their abilities in delivering children and young people’s crisis support. This includes examining their practice, identifying areas for growth and collaborating on strategies to further develop their skills. By prioritising reflective supervision, professionals can continually improve their ability to provide effective crisis support tailored to the unique needs of children, young people and their families or carers. There are a number of supervision models that teams can consider, some of which can be found at Clinical supervision models for registered professionals.
- Staff working in children and young people crisis services should have the required skills, knowledge, abilities and training to ensure they are current and capable in the following:
- work with a diverse range of needs. This entails being proficient in providing support to children and young people of all ages and their families or carers, with consideration of their unique requirements. Staff should be equipped to address the specific needs of looked after children and those with specific, complex, additional or multiple needs. For instance, staff should have the competencies to support autistic children and young people and those who have a learning disability or are neurodivergent. It is mandatory for all staff to complete the Oliver McGowan training. This training aims to enhance staff skills and knowledge when supporting children and young people who are autistic, have a learning disability or are neurodivergent. By ensuring staff possess the necessary competences, we can enhance the quality of care provided to children and young people with mental health needs, promoting inclusivity and tailored support to their specific requirements
- work within child protection and local safeguarding procedures
- understanding of the relevant key sections in the Mental Health Act, Children’s Act and Mental Capacity Act. For the Mental Health Act it is important to understand areas such as criteria for detention and patient rights, and the ability to draw on the necessary expertise to interpret and apply appropriate levels of care for those detained. It is important for clinicians to be able to communicate and explain legal processes, intervention options and rights for children and young people
- referring children and young people to their local dynamic support register to assess their risk level and consider a referral for a Care, Education and Treatment Review or assign a keyworker
- working in a systemic and holistic manner, ensuring they can engage the network around the child or young person
- in a crisis service that incorporates adult mental health practitioners, it is essential to provide them with training that enhances their comprehension of the developmental requirements specific to children and young people, as well as knowledge about the local pathways that pertain to this age group, including access to specialised inpatient services when necessary. Adult mental health staff should effectively adapt their existing crisis management skills to address the unique aspects associated with children and young people. This entails recognising appropriate developmental milestones; understanding capacity, consent and autonomy; being aware of communication differences; and emphasising the importance of working with families or carers as an integral part of the care process
- working collaboratively with colleagues from different sectors, such as ambulance services, A&E staff, children and young people’s mental health services, inpatient and paediatrics staff, primary care, local authority services, social workers and social care, as well as the voluntary, community and social enterprise (VCSE) sector
- the workforce should engage with the community they serve and with experts by experience through the development of children and young people/parent and carers forums to strengthen their understanding of children and young people’s needs and inform their services’ development by co-production
Staff core capabilities/skills
In collaboration with clinical, operational and commissioning colleagues, the diagram below illustrates the core capabilities and skills that are required across the children and young people’s urgent and emergency and crisis pathways. These are identified to assist colleagues in effectively fulfilling their roles. Underpinning the attributes, capabilities and skills are the core principles of staff adopting a compassionate, trauma-informed and empathetic approach. This includes actively listening and giving the child, young person, family and carers the opportunity to be heard.
Figure 3: core capabilities and skills that are required across the children and young people’s urgent and emergency and crisis pathways
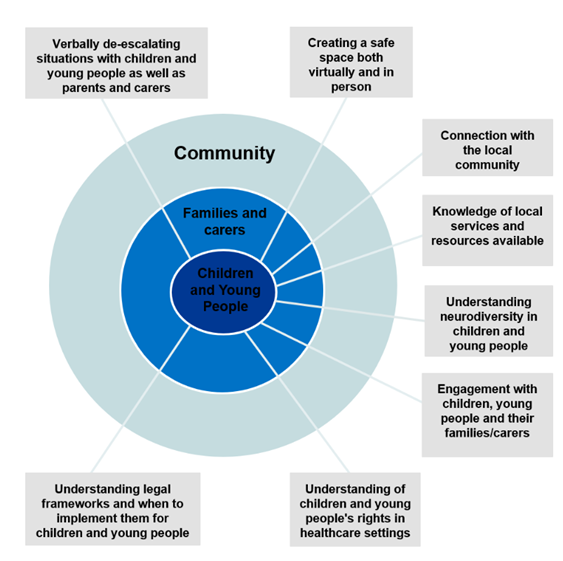
Figure 3 is a diagram that describes the core skills needed when working in crisis care with children and young people. They include understanding legal frameworks, understanding how to verbally de-escalate, the importance of engagement, connections to the local community and understanding neurodiversity.
Training
Training is of utmost importance in children and young people’s mental health teams, and it should be comprehensive and tailored to the specific client group and the existing skills, knowledge and abilities of the staff. It is crucial to incorporate training in both system-level workforce strategies and individual staff job plans as part of their ongoing professional development to ensure effective support for children and young people in crisis situations. This includes not only providing the necessary training but also ensuring the availability of supervision and in-practice support to integrate these skills into everyday work. Utilising tools such as Star can aid workforce planning for children and young people’s crisis services, helping to ensure comprehensive and effective support is provided.
Some potential approaches for education and training support may include:
- implementing a robust* induction and onboarding period that includes thorough training and orientation to ensure new staff are well-prepared for their roles and responsibilities, as well as to familiarise new staff with the specific requirements of working with children and young people in crisis
- providing targeted training to develop and enhance the key competencies identified in the diagram above
- organising in-person team training sessions or away days to foster collaboration, shared learning and skill development within the team and those supporting children and young people in the wider system, including team training days with colleagues from partner services (for example, in children’s social care, VCSEs, acute wards and A&E, youth justice, education, mental health champions in acute settings)
- facilitating MDT and peer shadowing opportunities to encourage cross-learning and knowledge exchange among colleagues
- allocating dedicated development time for staff to focus on enhancing their skills and knowledge through self-directed learning or specific training activities
- supporting CPD opportunities, which include research projects related to urgent and emergency care to build on the existing evidence base
- creating bitesize training videos or modules that offer concise and accessible learning materials on relevant topics
* A robust induction period and protected supervision time are essential components that should be built into staff work plans. Learning shared in the induction process should be revisited regularly.
By incorporating the training approaches above, children and young people’s mental health teams can enhance their capacity to provide effective support and care for children and young people in crisis situations.
It is recognised that working in children and young people’s crisis care can be impactful for staff at an individual and team level. The intensity of the emotions experienced by the child, young person and their family or carer along with the context of their crisis presentations, such as attempted suicide and/or self-harm and the risk of significant and possibly fatal harm, can understandably lead to vicarious trauma and moral injury among staff. In addition, the unpredictable and responsive nature of a crisis team can lead to a sense of heightened stimulation, leaving individuals and teams at increased risk of feeling overwhelmed and experiencing burn out. It is important that staff are given dedicated protected time and access to necessary support mechanisms such as peer support, debriefing sessions and supervision. Local leadership should prioritise leading with compassion (West 2021) and foster psychologically safe cultures within the crisis teams. This involves creating an environment where staff feel safe to openly discuss their experiences, seek support and address the emotional impact of their work. By recognising the potential impact on staff wellbeing and implementing appropriate support measures, organisations can better support the resilience and mental health of children and young people’s crisis care staff.
For training and resource materials please refer to the workforce training resource on the FutureNHS platform (FutureNHS is a member platform that requires a log in).
Routine outcome measures
Outcome measures help organisations to:
- monitor and improve the effectiveness, efficiency and quality of the service they offer to children, young people, families and carers
- support engagement and shared decision-making with the child or young person throughout the care offer
- demonstrate a service’s accountability
There are several questionnaire-based measures that report clinical outcomes from different perspectives:
- patient reported outcome measures (PROMs)
- clinician reported outcome measures (CROMs)
- patient reported experience measures (PREMs)
Using outcome measurement tools allows change to be measured and, where clinical outcomes are considered, the difference that an intervention/service is making. This change should be decided based on what is important to the child or young person and the service.
Crisis clinicians should be clear about why they are using the measures, agree on the best measure to use with the child or young person, and what they are going to do with the data from the measures. This information should be explained to the child, young person, family and carers. It is important where clinically appropriate to consider paired outcome measures for clinical interventions with children and young people. This will enable measurable change to be considered particularly when interventions are taking place:
- Children and young people should be asked for their consent to complete the measure, and this needs to be informed by content they have been given about the tool and its purpose. Children and young people should not be forced to complete outcome measures if they do not feel comfortable in doing so, but they should be offered the opportunity throughout their care.
- Reasonable adjustments should also be made for children and young people who are autistic/neurodivergent and/or who have a learning disability so that they can meaningfully engage with the outcome tool. For children and young people with severe and profound communication needs, input and support may be required from a speech and language therapist or a trusted person with whom the young person feels able to engage. They can support an alternative way of assessing outcomes.
- It may not always be appropriate to ask a child or young person to complete an outcome measure, so clinicians should assess whether it will affect the child or young person’s welfare.
- Outcome measures should be completed by the clinician in collaboration with the child or young person (and their parent or carers depending on the situation), and children or young people should be involved in choosing which measures best suit their needs and goals.
- It is important that children and young people are given options for how they complete measures, which may include them opting to complete measures privately and away from professionals/family or carers.
- Although helpful, outcome measures are only one source of information, and they should always be considered alongside clinical judgement.
Technical guidance on recording outcome measures for children and young people’s mental health services and further supporting information can be found in Children and young people’s mental health outcomes, Children and Young People’s Mental Health Transformation Programme on the Future NHS Collaboration Platform (FutureNHS is a member platform that requires a log in).
Children and young people crisis data
High quality and timely data is key to ensuring that systems can rapidly demonstrate the delivery of mental health crisis services, the extent to which they are meeting commitments set out in the NHS Long Term Plan, and the needs of children, young people and their families or carers and local populations. High quality data helps inform service planning and development, commissioning and patient outcomes.
Collecting data within children and young people’s crisis services contributes to service improvement and enables benchmarking against other services across the country. Data can support and empower clinicians and service leaders. Children and young people’s crisis data serves the dual purpose of both benchmarking the service and monitoring service improvement. It is crucial to share this data with service clinicians and leads to empower them in driving data quality initiatives.
Additionally, children and young people’s crisis data is collected through the NHS benchmarking data and the Getting It Right First Time (GIRFT) gateway metrics. The ability for services to benchmark their performance against these metrics is of paramount importance. By leveraging children and young people’s crisis data, service providers can gain valuable insights into their performance and identify areas for enhancement. Sharing this data with clinicians and service leads enables them to actively contribute to data quality improvements and fosters a culture of continuous service development. Furthermore, benchmarking against established metrics allows services to gauge their performance relative to industry standards and identify opportunities for growth and progress.
The key risk of poor data quality is that mental health metrics are not a true representation of service delivery, access and overall activity across the system. This leads to duplicate collections being instated, which is burdensome for providers and the wider system, and risks further impacting on the data quality of the Mental Health Services Data Set (MHSDS). It is therefore important that systems leaders create mechanisms that support clinicians to adequately capture and review clinical data activity.
Currently crisis care activity is captured in 2 datasets: the MHSDS and the Emergency Care Data Set (ECDS).
The MHSDS is the primary data source for mental health and learning disability services and includes information relating to referrals to community crisis teams, crisis alternative (including 24/7 crisis line) activity and liaison psychiatry.
The ECDS is a record-level dataset relating to urgent and emergency activity and includes information about why people attend the emergency department as well as the treatment they receive. This can be used to identify mental health-related attendances to A&E. For more on children and young people’s crisis data please refer to the resources on the FutureNHS platform (FutureNHS is a member platform that requires a log in).
Signposting to resources for children, young people and their families or carers
Children and young people crisis teams are in a unique position to provide valuable guidance, signposting and support to children, young people, their families and carers. Ensuring that every interaction is meaningful plays a crucial role in aiding the care and recovery of children and young people. The significance of managing mental health conditions within the community should not be overlooked. Individual, peer and community support are essential components. Therefore, it is important to have readily available written information and resources in children and young people crisis settings and during appointments. It should not be assumed that other professionals have already provided signposting or any other written information/material. Such resources could provide vital support to the entire family.
Resources for children and young people and their families or carers are available on the FutureNHS platform (FutureNHS is a member platform that requires a log in).
Acknowledgments
Sheena Gohal, National Services Advisor, Children and Young People’s Mental Health team, NHS England
Diana Gomes, Senior Project Manager, Children and Young People’s Mental Health team, NHS England
Suzanne Howes, Lived Experience Partner, Children and Young People’s Mental Health team, NHS England
Jo Lam, Lived Experience Partner, Children and Young People’s Mental Health team, NHS England
Clare Cooper, Advanced Nurse Practitioner, Cheshire and Wirral Partnership NHS Foundation Trust
Dr Ann Cox, Child and Adolescent Mental Health Service Nurse Consultant and Clinic Academic, Midlands Partnership NHS Foundation Trust
Vivienne Crosbie, Clinical Lead for Eating Disorder for Young People Services and Crisis Care team and Consultant Clinical Psychologist, Alder Hey
Emma Holland, Child and Adolescent Mental Health Service Crisis Clinical Service Lead, East London NHS Foundation Trust
Michelle Rudd, Transformation Lead for Children and Young People’s Mental Health Services, Clinical Lead West Midlands NHS England Clinical Network, Coventry and Warwickshire Partnership Trust
Sarah Stockham, Children and Young People’s Mental Health Clinical Lead Advisor for NHS England South West
Dr Michelle Trollope, Consultant Clinical Psychologist, Crisis Assessment and Intensive Support team, Norfolk and Suffolk Foundation Trust
With thanks also to the Children and Young People Crisis Task and Finish Group members for their contributions to this guidance. They included national clinical and operational leaders of children and young people crisis services, paramedics, nursing, psychological therapists, allied health professionals, psychiatry, lived experience partners, regional delivery leads, NHS England urgent and emergency care policy colleagues, children’s social care, workforce, NHS England Workforce, Training and Education directorate colleagues and policy representatives from the children and young people community, adult crisis care and children and young people acute care. NHS England’s Quality Transformation and Children’s Learning Disability and Autism Programmes also contributed.
References
Bettis AH, Donise KR, MacPherson HA, Bagatelas P, Wolff JC (2020). Safety planning intervention for adolescents: provider attitudes and response to training in the emergency services setting. Psychiatry Services 71(11): 1136-1142.
Cloutier P, Gray C, Sheridan N, Silverman A, Cappelli M, Zemek R, et al (2022) Building Resilience and Attachment in Vulnerable Adolescents (BRAVA): a brief group intervention for adolescents with mild-to-moderate suicidal ideation and their caregivers. Child and Adolescent Mental Health 27(4): 343-351.
Dekel I, Hertz-Palmor N, Dorman-Ilan S, Reich-Dvori M, Gothelf D, Pessach IM (2021) Bridging the gap between the emergency department and outpatient care: feasibility of a short-term psychiatric crisis intervention for children and adolescents. European Child and Adolescent Psychiatry Epub.
Edwards D, Carrier J, Csontos J, Evans N, Elliott M, Gillen E, et al (2023) Review: Crisis responses for children and young people – a systematic review of effectiveness, experiences and Service Organisation (camh‐crisis). Child and Adolescent Mental Health [Preprint].
Haruvi Catalan L, Levis Frenk M, Adini Spigelman E, Engelberg Y, Barzilay S, Mufson L, et al (2020) Ultra-brief crisis IPT-A based intervention for suicidal children and adolescents (IPT-A-SCI) pilot study results. Frontiers in Psychiatry 11.
Hayes D, Thievendran J, Kyriakopoulos M (2022) Adolescent inpatient mental health services in the UK. Archives of Disease in Childhood 107(5): 427-430.
Kwok KHR, Yuan SNV, Ougrin D (2016) Review: Alternatives to inpatient care for children and adolescents with mental health disorders. Child Adolescent Mental Health 21(1): 3-10.
Maguire EWBB (2022) What are health inequalities? The King’s Fund.
Murphy SM, Irving CB, Adams CE, Waqar M (2015) Crisis intervention for people with severe mental illnesses. Cochrane Database of Systematic Reviews Issue 12: CD001087.
Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR (2015) Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry 54(2): 97-107.
Ougrin D, Corrigall R, Poole J, Zundel T, Sarhane M, Slater V, et al (2018) Comparison of effectiveness and cost-effectiveness of an intensive community supported discharge service versus treatment as usual for adolescents with psychiatric emergencies: A randomised controlled trial. Lancet Psychiatry 5(6):477-485.
Ougrin D, Corrigall R, Stahl D, Poole J, Zundel T, Wait M, et al (2020) Supported discharge service versus inpatient care evaluation (site): A randomised controlled trial comparing effectiveness of an intensive community care service versus inpatient treatment as usual for adolescents with severe psychiatric disorders: Self-harm, functional impairment, and educational and clinical outcomes. European Child & Adolescent Psychiatry 30(9):1427-1436.
Rengasamy M, Sparks G (2019) Reduction of post discharge suicidal behaviour among adolescents through a telephone-based intervention. Psychiatric Services 70(7): 545-552.
Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, et al (2018) Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry 75(9): 894-900.
West M (2021) Compassionate leadership. Sustaining Wisdom, humanity and presence in health and social care. The Swirling Leaf Press, pp31-45, 87-106.
Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al (2021). Interventions for self-harm in children and adolescents. Cochrane Database of Systematic Reviews Issue 3.
World Health Organization (2023). Disability.
Zullo L, Meza JI, Rolon-Arroyo B, Vargas S, Venables C, Miranda J, et al (2020). Enhancing safety: Acute and short-term treatment strategies for youths presenting with suicidality and self-harm. The Behaviour Therapist.
Publication reference PRN00503